 Journal of Biosciences and Medicines, 2014, 2, 12-17 Published Online August 2014 in SciRes. http://www.scirp.org/journal/jbm http://dx.doi.org/10.4236/jbm.2014.26003 How to cite this paper: Minami, M., et al. (2014) Prevalence and Antimicrobial Susceptibility Pattern of Streptococcus pneumoniae at General Hospital in the Central Region of Japan from December 2013 to February 2014. Journal of Bio- sciences and Medicines, 2, 12-17. http://dx.doi.org/10.4236/jbm.2014.26003 Prevalence and Antimicrobial Susceptibility Pattern of Streptococcus pneumoniae at General Hospital in the Central Region of Japan from December 2013 to February 2014 Masaaki Minami1*, Ryoko Sakakibara2, Taichi Imura2, Hideo Morita2, Naoto Kanemaki3, Michio Ohta4 1Department of Bacteriology, Graduate School of Medical Sciences, Nagoya City University, Nagoya, Japan 2Department of Clinical Investigation, Daido Hospital, Nagoya, Japan 3Department of Gastroenterology, Daido Hospital, Nagoya, Japan 4School of Nursing, Sugiyama Jyogakuen University, Nagoya, Japan Email: *mina mi@ med.n ago ya -cu.ac.jp Received June 2014 Abstract Streptococcus pneum on ia infection is important cause of morbidity and mortality. This study was conducted to find out the prevalence and antimicrobial susceptibility pattern of Streptococcus pneum on ia e isolates at general hospitalin the central region of Japan from December 2013 to February 2014. Streptococcus pneumoniae was identified by standard laboratory procedure. An- timicrobial susceptibility testing was performed by micro dilution assay according to CLSI rec- ommend ati on. One hundred fifty-three Streptococcus pneumoniae were isolated among which 80 (52.2%) were males and 73 (47.8%) were females. Nasal discharge (134%/87.6%) contributed more than other biological materials. The age incidence of (0 - 1) years, (1 - 10) years, (11 - 40) years, (41 - 60) years and >60 years age groups were 26 (17.0%), 110 (71.9%), 3 (2.0%), 10 (6.5%), and 4 (2.6%) respectively. Positive samples were received mostly from the pediatrics (137%/89.5%), respiratory medicine (12%/ 7.8%) and lowest from gastroenterology (1%/0.6%) and neurology (1/ 0.6%) department. Vancomycin and rifampicin were the most active antibiotics with 100% susceptibility rates. The next best were levofloxacin, penicillin G and ceftriaxone. Our study revealed that 82 Streptococcus pneumonia isolates had multidrug resistant ability (53.6%). Streptococcus pneumoniae infection spreads among community easily and inappropriate use of antibiotics contributes to their resistance. Continuous antimicrobial susceptible surveys are es- sential to guide policy on the adequate use of antibiotics to reduce the morbidity and mortality and reduce the emergency of antimicrobial resistance. Keywords Streptococcus pneumoniae, Susceptibility, Antimicrobial Resistance, Multi Drug Resistance *  M. Minami et al. 1. Introduction Streptococcus pneumoniae is one of the most common bacteria causing pneumonia, meningitis, bacteremia and many other infections, and continues to be an important cause of morbidity and mortality in the world [1]. Globall y, an estimated 1.6 million people including 1 million children less than 5 years old die of invasive pneumonia disease annually [2]. Its clinical burden is concentrated among the very old and very young [2]. De- spite this high toll, the vast majority of Streptococcus pneumoniae are found in asymptomatic nasopharyngeal carriage, the prevalence of which varies by age and region [3]. The carriage state is responsible for transmission, and is the stage of Streptococcus pneumoniae life history at which interventions such as antibiotics and vaccines exert their selective pressure [4]. The present study was conducted to find out the recent prevalence and antimicrobial susceptibility pattern of Streptococcus pneumoniae isolates at general hospital in the central of Japan. Our result would be useful in es- tablishing empiric therapy guidelines and to contribute to larger more extensive surveillance study. 2. Materials and Methods 2.1. Strains and Clinical Data Collection A total of 153 Streptococcus pneumoniae were obtained from various clinical specimens at Daido Hospital from December 2013 to February 2014. Daido Hospital is a 404-bed private general hospital in the central region of Japan. We used medical records appended to clinical species for the analysis of clinical feature at Daido Hospit- al. We considered several isolates from the same region of the same patient as one isolate per one patient for the analysis in this study. All streptococcal isolates were identified by standard conventional biochemical methods or the VITEK2 system (b ioMé rieux, Durham NC, USA). Our experimental design was approved by the ethics committee at Daido hospital. 2.2. Antimicrobial Susceptibility Analysis Streptococcus pneumoniae isolates were examined for 15 antibiotic susceptibilities as follows; PCG, penicillin G; AMPC, amoxicillin; CTX, cefotaxime; CTRX, ceftriaxone; IPM, imipenem; MEPM, meropenem; LVFX, levofloxacin; OFLX, ofloxacin; CAM, clarithromycin; EM, erythromycin; VCM, vancomycin; TC, tetracycline; CP, chloramphenicol; RFP, rifampicin, ST, Trimethoprim-sulfamethoxazole. Minimal inhibitory concentration (MICs) were determined at clinical laboratory in Daido Hospital using broth micro dilution methodology with the VITEK2 system. MICs were calculated as MIC90 (MIC causing inhibition of 90% of isolates). Percentage susceptibilities were calculated based on Clinical Laboratory Standard Institute (CLSI) break point [5]. We used two separate interpretive breakpoints for meningeal and non-meningeal isolates to define penicillin. Multidrug resistance (MDR) was defined as non-susceptibility to more than any three antimicrobial agents [6]. 2.3. Statistical Analysis of the Dat a We conducted the statistical analysis with the chi-squared test or Fisher’s exact test when appropriate. Differ- ences were considered significant when p was <0.05. 3. Results One hundred fifty-t hre e Streptococcus pneumoniae were isolated among which 80 (52.2%) were from male pa- tient and 73 (47.8%) were from females. Nasal discharge 134 (87.6%) [male-69, female-65], sputum 15 (9.7%) [ma le-9, female-6], tonsil 2(1.3%) [mal e-1, female-1], pharyngeal mucus 1(0.7%) [mal e-1, fema le -1], and blood 1 (0.7%) [male-1, female-1] were the source of Streptococcus pneumoniae isolates (Table 1). There was no sig- nificant difference between male and female. The age incidence among 0 - 1 years age group was 26 (17%) [ma le-17, female-9], among 1 - 10 years age group, 110 (71.9%) [male-52, female-58] (p < 0.05), among 11 - 40 years age group, 3 (1.7%) [male-2, fe- male -1], in 41-60 years it was 10 (6.5%) [male-8, female-2] and in >60 years age group it was 4 (2.6%) [male-2, fema le -2] (Table 2). There was no significant difference between male and female. Most of the Streptococcus pneumoniae isolates were from the pediatrics (137/89.5%) [male-69, female-68] followed by respiratory medicine (12/7.8%) [male-9, Female-3], general medicine (2/1.3%) [male -1, female-1] 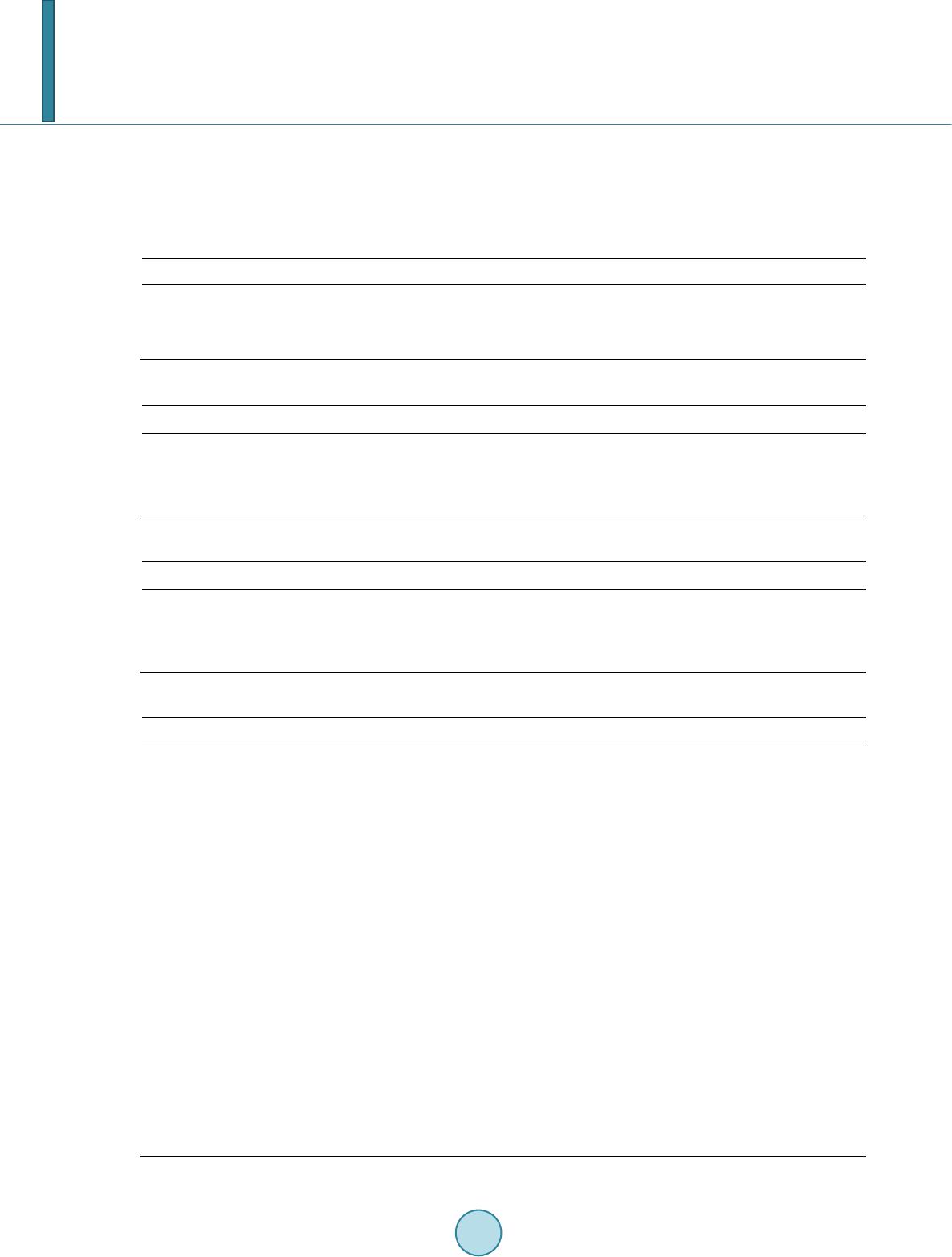 M. Minami et al. and lowest from gastroenterology (1/0.6%) [mal e-0, femal e -1], and neurology department (1/0.6%) [male-1, fema le -0] (Table 3). There was no significant difference between male and female. The results of antimicrobial susceptibility of Streptococcus pneumoniae isolates to various antibiotics tested in this study are shown in Table 4. Vancomycin and rifampicin were the most active antibiotics with 100%. Table 1. Biological material wise distribution of Streptococcus pneumoniae isolates. biological material nasal discharge sputum tonsil pharyngeal mucus blood male 69 9 1 0 1 female 65 6 1 1 0 total 134 15 2 1 1 Table 2. Age wise distribution of Streptococcus pneumoniae isolates. age groups (0 - 1) years (1 - 10) years (11 - 40) years (41 - 60) years >60 years male 17 52 1 8 2 female 9 58 2 2 2 total 26 110 3 10 4 Table 3. Clinical department wise distribution of Streptococcus pneumoniae isolates. clinical department pediatrics respiratory medicine general medicine gastroenterology neurology male 69 9 1 0 1 female 68 3 1 1 0 total 137 12 2 1 1 Table 4. Antimicrobial susceptibility of Streptococcus pneumoniae isolates. antimicrobial agents MIC90 (mg/mL) range % susceptibility PCG 2 ≤0.06 - 4 97.4 AMPC 2 ≤0.06 - 4 92.8 CTX 1 ≤0.06 - 4< 93.5 CTRX 1 ≤0.06 - 4< 96.1 IPM 0.25 <0.03 - 0.5 74.5 MEPM 1 ≤0.06 - 0.12 73.9 LVFX 2 ≤0.5 - 8≤ 98.7 OFLX 4 ≤1 - 8≤ 88.9 CAM 1≤ ≤0.25 - 1≤ 6.5 EM 1≤ ≤0.25 - 1≤ 7.2 VCM ≤1 ≤1 100.0 TC 16≤ ≤1 - 16≤ 8.5 CP 16 ≤2 - 32≤ 87.6 RFP ≤0.25 ≤0.25 100.0 ST 20 ≤10 - 80 79.7  M. Minami et al. susceptibility rates. The next best antibiotics with over 95% susceptibility rates were levofloxacin (98.7%), pe- nicillin G (97.4%), and ceftriaxone (96.1%). Significant resistant were observed in tetracycline (8.5%), eryt- hromycin (7.2%), clarithromycin (6.5%). Our study revealed that 82 Streptococcus pneumoniae isolates had multidrug resistant ability (53.6%). The most common pattern of MDR was resistant to clarithromycin, tetracycline, and imipenem (25.5%), followed by resistant to clarithromycin, tetracycline, and trimethoprim - sulfamethoxazole (16.3%). Most Streptococcus pneumoniae isolates with MDR were resistant to at least one of the macrolides tested. 4. Discussion In this study, we described the characteristics of Streptococcus pneumonia isolates from December 2013 to February 2014 at general hospital in the central region of Japan. With respect to gender group, Streptococcus pneumoniae were isolated more from female patients than male patients. Although previous report showed that the number of male patient was significant greater than that of female patient [7], our study showed the male to female ratio was about 1.1 time and there was no significant differences among gender. We clarified Streptococcus pneumoniae with age distribution. The present study reveals the prevalence of Streptococcus pneumonia more in extremes of age group as seen in 0 - 1 years age group, it is 17%, increasing to 71.9% in 1 - 10 years age group, diminishing to 2% in 11 - 40 years age group, again increasing to 6.5% in 41% - 60 years age group and finally diminished to 2.6% in more than 60 years age group. Although young pa- tients under 10 years frequently caused Streptcococcus pneumoniae infection, the large numbers of Streptc o- coccus pneumoniae were not isolated from over 60 years age patients in o ur study. Previous report showed that high incidence of pneumonia in children and elder people in different parts of world [7] [8]. It is suggested to decrease immunity in the extremes of age groups. In the analysis of clinical departments, we found that department where most patients with Streptococcus pneumoniae were detected was pediatrics. Streptococcus pneumoniae infection, especially acute pharyngitis and tonsillitis, was usually popular as pediatric diseases [1]. The disease burden of Streptococcus pneumoniae infections has increased due to widespread emergence of antimicrob ial resistance in many countries from 1990’s [2]. Previous studies documented very high prevalence rates of beta-lactam and macrolide resistance in Streptococcus pneumoniae in Asian countries [2] [9]-[13]. Par- ticularly, macroride resistance has remarkably increased in many Asian countries, where over 70% of clinical isolates were fully resistant [2] [9] [12] [13]. Antimicrobial susceptible analysis of Streptococcus pneumoniae revealed that macrolide was no longer effective against these bacteria because macrolide resistant rates of Streptococcus pneumoniae were more than 90%. Recently Clarithromycin and Azithromycin, which we call new macrolide, have been used frequently against respiratory tract infectious disease. Thus, we need further antimi- crobial surveillance to prevent the spread of new macroride resistant Streptococcus pneumoniae. Streptococcus pneumoniae also had tetracycline - resistant pattern. This result implies that Streptococcus possesses the same pathogenic island including both macrolide and tetracycline resistant genes [4]. We found a low prevalence of penicillin resistance in non-meningeal isolates according to the revised CLSI breakpoints for resista nce to parenteral penicillin, although penicillin MICs have increased in some countries such as China and India compared with past investigation [9]. Most of the non-meningeal isolates from Asian countries were sus- ceptible to parenteral penicillin, a finding consistent with other study worldwide (<7%) [2] [9] [13]. As the emergence of penicillin resistant Streptococcus pneumoniae is low, our result showed that the prevalence of im- ipenem non-susceptibility was not low in Japan. We need to focus on the carbapenem susceptible pattern in Streptococcus pneumonia hereafter. The overall rates of resistance to fluoroquinolone in Streptococcus pneumo- niae remained low in most countries including Japan [2] [9] [13]. Thus, given the popular use of respiratory flu- oroquinlone in clinical practice, the emergency of these strains highly resistant to fluoroquinolone could be a concern in the future in the treatment of Streptococcus pneumoniae pneumonia. In addition, MDR Streptococcus pneumonia was also very prevalent in Asian countries (59.3%), particularly in China (83.3%), Vietnam (75.5%), South Korea (63.9%), Hong Kong (62.2%), and Taiwan (59.7%) [9]. From our result, multi drug resistance was 53.6% in Japan. But this rate in Japan was much higher than those in other parts world such as 9% to 24% in North America and 0% to 43% in Europe [2] [9] [14]. The emergence of MDR Streptococcus pneumonia in- cluding macrolide, tetracycline, and carbapenem resistant strains will raise the serious problem in Asian coun-  M. Minami et al. tries including Japan [13] [15 ]. 5. Conclusions Incidence of Streptococcus pneumoniae infection is increasing worldwide affecting the children and aged adult population which may lead to severe invasive infection by dissemination to other organs of the body if not treated adequately. The indiscriminate and inadvertent use of antibiotics has led to the emergence of multidrug resistance among commonly used antibiotics. Our investigation aims to guide medical officer on appropriate use of antibiotics. This aim is not only to re- duce the morbidity and mortality in the patients but also to control the emergence and spread of resistance among Streptococcus pneumoniae. Continuous surveillance of the use of antibiotics helps in preserving the ef- fectiveness of antibiotics. The results from our study strongly emphasize the need for continuous epidemiologi- cal monitoring of antibiotic resistant. Acknowledgements We thank Mr. Shoji Ishihara and Ms. Miwako Fujimura for special encouragement. This study was supported by a grant-in-aid for research from the Nagoya City University, Japan. References [1] Mitchell, A.M. and Mitchell, T.J. (2010) Streptococcus pneumoniae: Virulence Factors and V ariation. Clinical Micro- biology and Infection, 16, 411-418 . http://dx.doi.org/10.1111/j.1469-0691. 2010 .03 18 3.x [2] Lynch, J.P. and Zhanel, G.G. (2009) Streptococcus pneumoniae: Epidemiology, Risk Factors and Strategies for Pre- vention. Seminars in Respiratoryand Critical, Care Medicine, 30, 189-209. http://dx.doi.org/10.1055/s-0029-12029 38 [3] Crook, D.W., Brueggemann, A.B., Sleeman, K.L. and Peto, T.E.A. (2004) Pneumococcal Carriage. In: Tuomanen, E.I., Mitchell, T.J., Morrison, D.A. and Spratt, B.G., Eds., The Pneumococcus, American Society for Microbiology, Was h- ington DC, 136-148. [4] Willems, R.J.L., Hanage, W.P., Bessen, D.E. and Feil, E.J. (2011) Population Biology of Gram-Positive Pathogens: High -Risk Clones for Dissemination of Antibiotic Resistance. FEMS Microbiology Review, 35, 872-900. http://dx.doi.org/10.1111/j.1574-6976.2011.00284.x [5] Clinical and Laboratory Standards Institute (CLSI) (2014) Performance Standards for Antimicrobial Susceptibility Testing: 24st Informational Supplement. Clinical and Laboratory Standards Institute M100-S24, Wa y ne . [6] Magiorakos, A.P., Srinivasan, A., Carey, R.B., Carmeli, Y., Falagas, M.E., Giske, C.G., et al. (2012) Multidrug-Re- sistant, Extensively Drug-Re sistant and Pandrug-Resistant Bacteria: An International Expert Proposal for Interim Standard Definitions for Acquired Resistance. Clinical Microbiology and Infection, 18, 268-281. http://dx.doi.org/10.1111/j.1469-0691.2011.03570.x [7] Geng, Q., Zhang, T., Ding, Y., Tao, Y., Lin, Y., Wang, Y., et al. (2014) Molecular Characterization and Antimicrobial Susceptibility of Streptococcus pneumoniae Isolated from Children Hospitalized with Respiratory Infections in Suzhou, China. PLoS One, 9, e93752. http://dx.doi.org/10.1371/journal.pone.0093752 [8] H of ma n, J., Cetron, M.S. and Farley, M.M. (1995) The Prevalence of Drug Resistant Streptococcus pneumoniae in At- lanta. New England. Journal of Medicine, 333, 48 1 -486. http://dx.doi.org/10.1056/NEJM199508243330803 [9] Kim, S.H., Song, J.H., Chung, R.D., Thamlikitkul, V., Yang, Y., Wang, H., et al. on Behalf of ANSORP Study Group (2012) Changing Trends in Antimicrobial Resistance and Serotypes of Streptococcus pneumoniae Isolates in Asian Countries: An Asian Network for Surveillance of Resistant Pathogens (ANSORP) Study. Antimicrobial Agents and Chemotherapy, 56, 1418-142 6. [10] Xue, L., Yao, K., Xie, G., Zheng, Y., Wang, C., Shang, Y., et al. (2010) Serotype Distribution and Antimicrobial Re- sistance of Streptococcus pneumoniae Isolates That Cause Invasive Disease among Chinese Children. Clinical Infec- tious Disease, 50, 741-744. http://dx.doi.org/10.1086/650534 [11] Zhao, C., Zhang, F., Chu, Y., Liu, Y., Cao, B., Chen, M., et al. (2013) Phenotypic and Genotypic Characteristic of In- vasive Pneumococcal Isolates from Both Children and Adult Patients from a Multicenter Surveillance in China 2005-2011. Plos One, 8, e82361. http://dx.doi.org/10.1371/journal.pone.0082361 [12] Zhang, Y., Chen, Y., Wang, Z., Li Y., Wang, D., Shang, Y., et al. (2013) Serological and Molecular Capsular Typing, Antibiotic Susceptibility and Multilocus Sequence Typing of Streptococcus pneumoniae Isolates from Invasive and Non-Invasive Infections. Chinese Medical Journal, 126, 2296-2303. [13] Okade, H., Funatsu, T., Eto, M., Furuya, Y., Mizunaga, S., Nomura, N., et al. (2014) Impact of the Pneumococcal  M. Minami et al. Conjugate Vaccine on Serotype Distribution and Susceptibility Trends of Pediatric Non-Inv asive Streptococcus pneu- moniae Isolates in Tokai, Japan over a 5-Year Period. Jour nal of Infection and Chemotherapy. http://dx.doi.org/10.1016/j.jiac.2014.03.010 [14] Dunais, B., Bruno-Bazureault, P., Carsenti-Dellamonica, H., Touboul, P. and Pradir, C. (2011) Adecade-Long Surveil- lance of Nasopharyngeal Colonization with Streptococcus pneumoniae among Children Attending Day-Care Centres in South-Eastern France: 1999-2008. European Journal of Clinical Microbiology and Infection Disease, 30, 837-843. http://dx.doi.org/10.1007/s10096-011-1154-9 [15] Tajima, T., Sato, T., Toyonaga, Y., Hanaki, H. and Sunakawa, K. (2013) Nationwide Survey of the Development of Drug-Resistant Pathogens in the Pediatric Field in 2007 and 2010: Drug Sensitivity of Streptococcus pneumoniae in Japan (Second Report). Journal of Infection and Chemotherapy, 19, 510-516. http://dx.doi.org/10.1007/s10156-013-0593-x
|