78 M. SIGAROUDINIA ET AL.
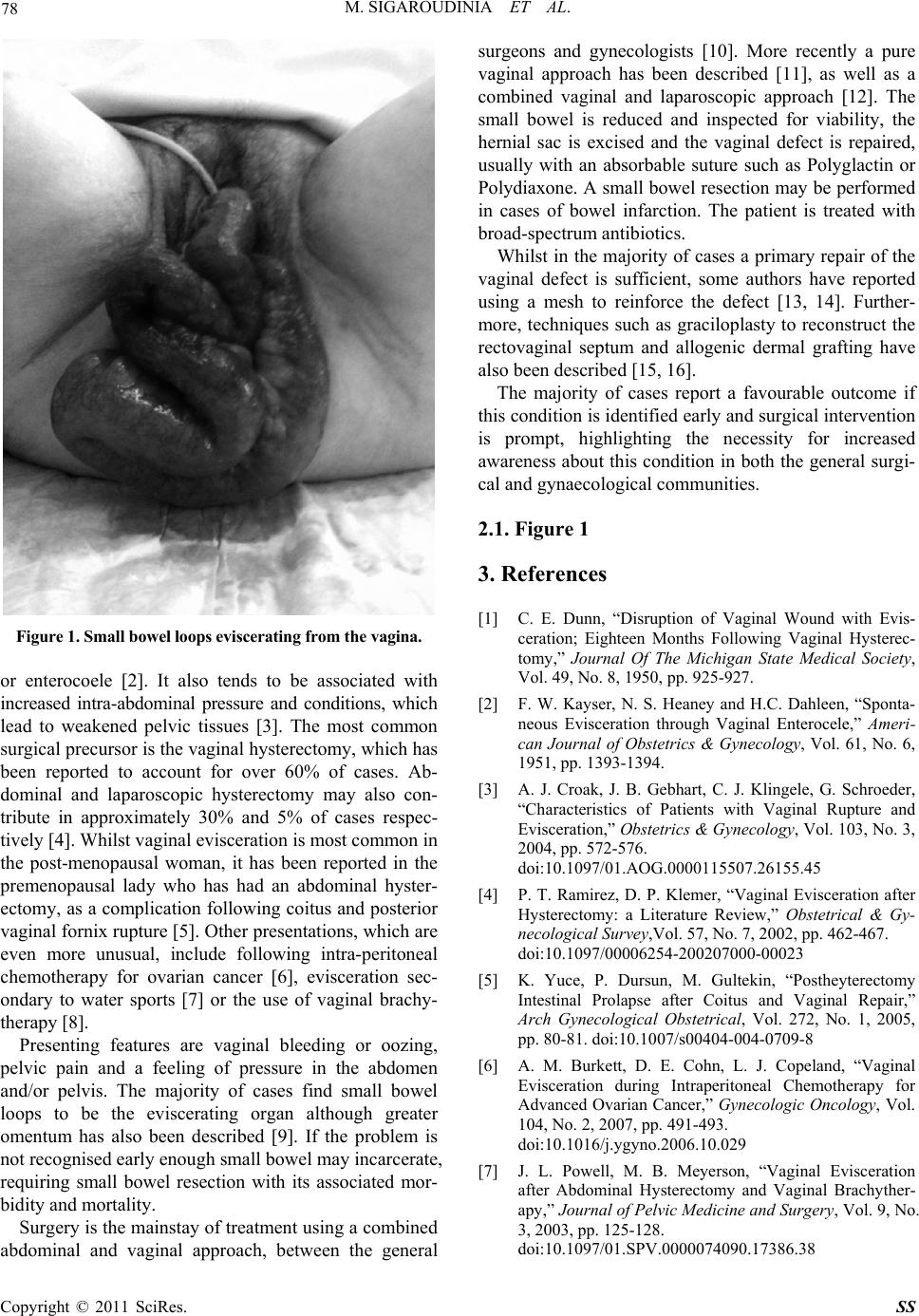
Figure 1. Small bowel loops eviscerating from the vagina.
or enterocoele [2]. It also tends to be associated with
increased intra-abdominal pressure and conditions, which
lead to weakened pelvic tissues [3]. The most common
surgical precursor is the vaginal hysterectomy, which has
been reported to account for over 60% of cases. Ab-
dominal and laparoscopic hysterectomy may also con-
tribute in approximately 30% and 5% of cases respec-
tively [4]. Whilst vaginal evisceration is most common in
the post-menopausal woman, it has been reported in the
premenopausal lady who has had an abdominal hyster-
ectomy, as a complication following coitus and posterior
vaginal fornix rupture [5]. Other presentations, which are
even more unusual, include following intra-peritoneal
chemotherapy for ovarian cancer [6], evisceration sec-
ondary to water sports [7] or the use of vaginal brachy-
therapy [8].
Presenting features are vaginal bleeding or oozing,
pelvic pain and a feeling of pressure in the abdomen
and/or pelvis. The majority of cases find small bowel
loops to be the eviscerating organ although greater
omentum has also been described [9]. If the problem is
not recognised early enough small bowel may incarcerate,
requiring small bowel resection with its associated mor-
bidity and mortality.
Surgery is the mainstay of treat ment using a combined
abdominal and vaginal approach, between the general
surgeons and gynecologists [10]. More recently a pure
vaginal approach has been described [11], as well as a
combined vaginal and laparoscopic approach [12]. The
small bowel is reduced and inspected for viability, the
hernial sac is excised and the vaginal defect is repaired,
usually with an absorbable suture such as Polyglactin or
Polydiaxone. A small bowel resection may be performed
in cases of bowel infarction. The patient is treated with
broad-spectrum antibiotics.
Whilst in the majority of cases a primary repair of the
vaginal defect is sufficient, some authors have reported
using a mesh to reinforce the defect [13, 14]. Further-
more, techniques such as graciloplasty to reconstruct the
rectovaginal septum and allogenic dermal grafting have
also been descr i b ed [15, 16].
The majority of cases report a favourable outcome if
this condition is iden tified early and surgical interv ention
is prompt, highlighting the necessity for increased
awareness about this condition in both the general surgi-
cal and gynaecological communities.
2.1. Figure 1
3. References
[1] C. E. Dunn, “Disruption of Vaginal Wound with Evis-
ceration; Eighteen Months Following Vaginal Hysterec-
tomy,” Journal Of The Michigan State Medical Society,
Vol. 49, No. 8, 1950, pp. 925-927.
[2] F. W. Kayser, N. S. Heaney and H.C. Dahleen, “Sponta-
neous Evisceration through Vaginal Enterocele,” Ameri-
can Journal of Obstetrics & Gynecology, Vol. 61, No. 6,
1951, pp. 1393-1394.
[3] A. J. Croak, J. B. Gebhart, C. J. Klingele, G. Schroeder,
“Characteristics of Patients with Vaginal Rupture and
Evisceration,” Obstetrics & Gynecology, Vol. 103, No. 3,
2004, pp. 572-576.
doi:10.1097/01.AOG.0000115507.26155.45
[4] P. T. Ramirez, D. P. Klemer, “Vaginal Evisceration after
Hysterectomy: a Literature Review,” Obstetrical & Gy-
necological Survey,Vol. 57, No. 7, 2002, pp. 462-467.
doi:10.1097/00006254-200207000-00023
[5] K. Yuce, P. Dursun, M. Gultekin, “Postheyterectomy
Intestinal Prolapse after Coitus and Vaginal Repair,”
Arch Gynecological Obstetrical, Vol. 272, No. 1, 2005,
pp. 80-81. doi:10.1007/s00404-004-0709-8
[6] A. M. Burkett, D. E. Cohn, L. J. Copeland, “Vaginal
Evisceration during Intraperitoneal Chemotherapy for
Advanced Ovarian Cancer,” Gynecologic Oncology, Vol.
104, No. 2, 2007, pp. 491-493.
doi:10.1016/j.ygyno.2006.10.029
[7] J. L. Powell, M. B. Meyerson, “Vaginal Evisceration
after Abdominal Hysterectomy and Vaginal Brachyther-
apy,” Journal of Pelvic Medicine and Surgery, Vol. 9, No.
3, 2003, pp. 125-128.
doi:10.1097/01.SPV.0000074090.17386.38
Copyright © 2011 SciRes. SS