Paper Menu >>
Journal Menu >>
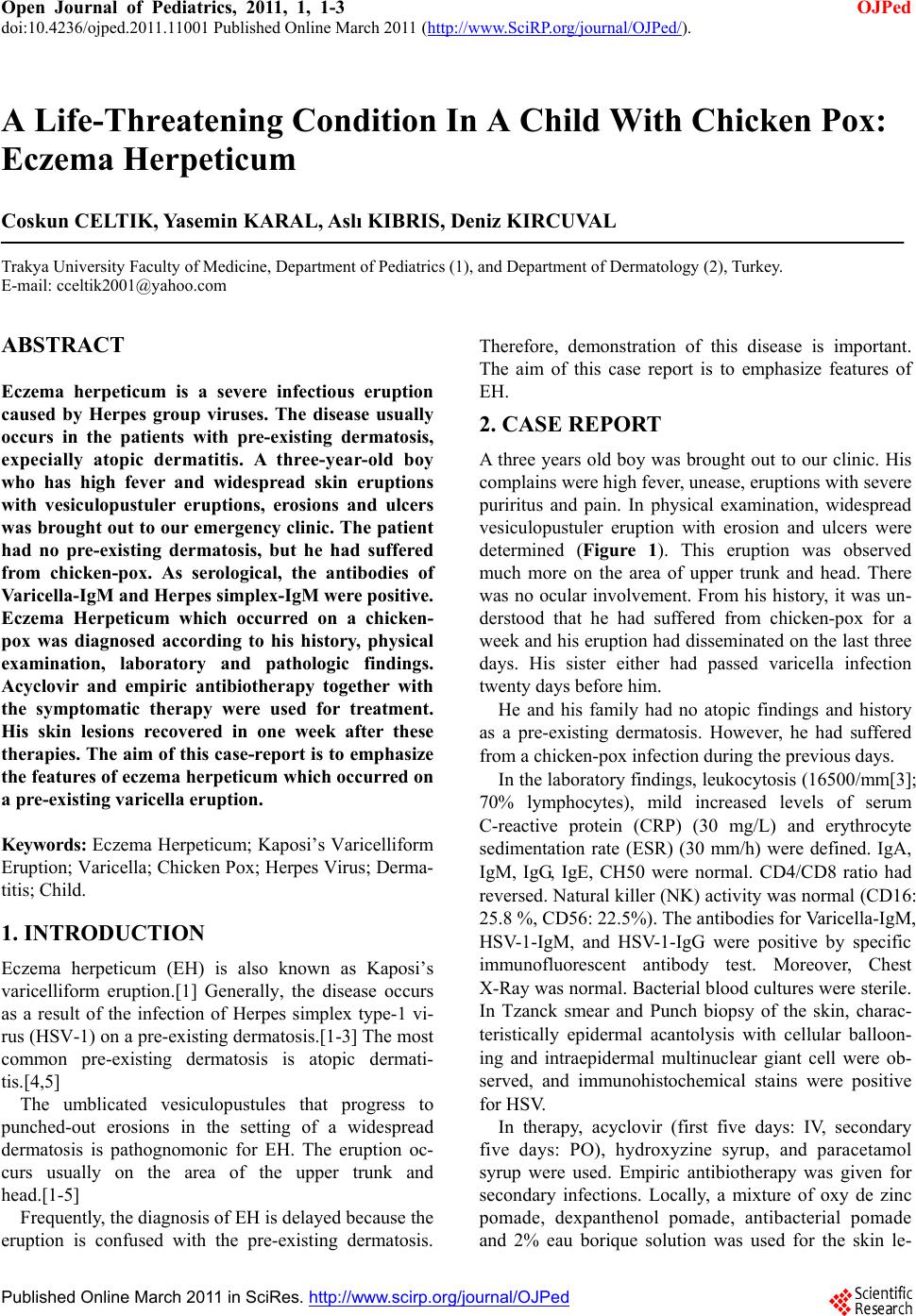 Open Journal of Pediatrics, 2011, 1, 1-3 doi:10.4236/ojped.2011.11001 Published Online March 2011 (http://www.SciRP.org/journal/OJPed/ OJPed ). Published Online March 2011 in SciRes. http://www.scirp.org/journal/OJPed A Life-Threatening Condition In A Child With Chicken Pox: Eczema Herpeticum Coskun CELTIK, Yasemin KARAL, Aslı KIBRIS, Deniz KIRCUVAL Trakya University Faculty of Medicine, Department of Pediatrics (1), and Department of Dermatology (2), Turkey. E-mail: cceltik2001@yahoo.com ABSTRACT Eczema herpeticum is a severe infectious eruption caused by Herpes group viruses. The disease usually occurs in the patients with pre-existing dermatosis, expecially atopic dermatitis. A three-year-old boy who has high fever and widespread skin eruptions with vesiculopustuler eruptions, erosions and ulcers was brought out to our emergency clinic. The patient had no pre-existing dermatosis, but he had suffered from chicken-pox. As serological, the antibodies of Varicella-IgM and Herpes simplex-IgM were positive. Eczema Herpeticum which occurred on a chicken- pox was diagnosed according to his history, physical examination, laboratory and pathologic findings. Acyclovir and empiric antibiotherapy together with the symptomatic therapy were used for treatment. His skin lesions recovered in one week after these therapies. The aim of this case-report is to emphasize the features of eczema herpeticum which occurred on a pre-existing varicella eruption. Keywords: Eczema Herpeticum; Kaposi’s Varicelliform Eruption; Varicella; Chicken Pox; Herpes Virus; Derma- titis; Child. 1. INTRODUCTION Eczema herpeticum (EH) is also known as Kaposi’s varicelliform eruption.[1] Generally, the disease occurs as a result of the infection of Herpes simplex type-1 vi- rus (HSV-1) on a pre-existing dermatosis.[1-3] The most common pre-existing dermatosis is atopic dermati- tis.[4,5] The umblicated vesiculopustules that progress to punched-out erosions in the setting of a widespread dermatosis is pathognomonic for EH. The eruption oc- curs usually on the area of the upper trunk and head.[1-5] Frequently, the diagnosis of EH is delayed because the eruption is confused with the pre-existing dermatosis. Therefore, demonstration of this disease is important. The aim of this case report is to emphasize features of EH. 2. CASE REPORT A three years old boy was brought out to our clinic. His complains were high fever, unease, eruptions with severe puriritus and pain. In physical examination, widespread vesiculopustuler eruption with erosion and ulcers were determined (Figure 1). This eruption was observed much more on the area of upper trunk and head. There was no ocular involvement. From his history, it was un- derstood that he had suffered from chicken-pox for a week and his eruption had disseminated on the last three days. His sister either had passed varicella infection twenty days before him. He and his family had no atopic findings and history as a pre-existing dermatosis. However, he had suffered from a chicken-pox infection during the previous days. In the laboratory findings, leukocytosis (16500/mm[3]; 70% lymphocytes), mild increased levels of serum C-reactive protein (CRP) (30 mg/L) and erythrocyte sedimentation rate (ESR) (30 mm/h) were defined. IgA, IgM, IgG, IgE, CH50 were normal. CD4/CD8 ratio had reversed. Natural killer (NK) activity was normal (CD16: 25.8 %, CD56: 22.5%). The antib od ies for Varicella-IgM, HSV-1-IgM, and HSV-1-IgG were positive by specific immunofluorescent antibody test. Moreover, Chest X-Ray was normal. Bacterial blood cu ltures were sterile. In Tzanck smear and Punch biopsy of the skin, charac- teristically epidermal acantolysis with cellular balloon- ing and intraepidermal multinuclear giant cell were ob- served, and immunohistochemical stains were positive for HSV. In therapy, acyclovir (first five days: IV, secondary five days: PO), hydroxyzine syrup, and paracetamol syrup were used. Empiric antibiotherapy was given for secondary infections. Locally, a mixture of oxy de zinc pomade, dexpanthenol pomade, antibacterial pomade and 2% eau borique solution was used for the skin le- 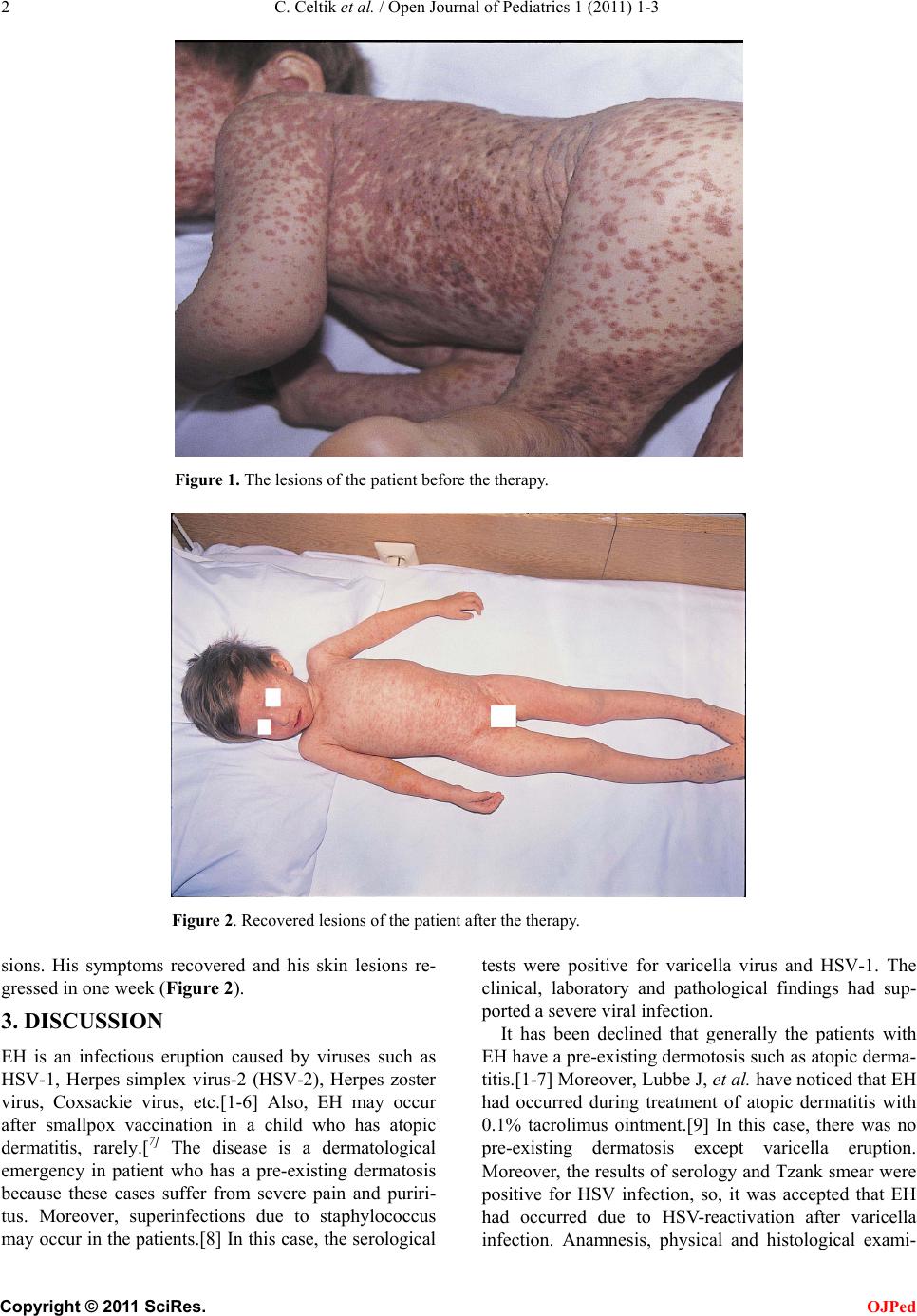 2 C. Celtik et al. / Open Journal of Pediatrics 1 (2011) 1-3 Figure 1. The lesions of the patient before the therapy. Figure 2. Recovered lesions of the patient after the therapy. sions. His symptoms recovered and his skin lesions re- gressed in one week (Figure 2). 3. DISCUSSION EH is an infectious eruption caused by viruses such as HSV-1, Herpes simplex virus-2 (HSV-2), Herpes zoster virus, Coxsackie virus, etc.[1-6] Also, EH may occur after smallpox vaccination in a child who has atopic dermatitis, rarely.[7] The disease is a dermatological emergency in patient who has a pre-existing dermatosis because these cases suffer from severe pain and puriri- tus. Moreover, superinfections due to staphylococcus may occur in the patients.[8] In this case, the serological tests were positive for varicella virus and HSV-1. The clinical, laboratory and pathological findings had sup- ported a severe viral infection. It has been declined that generally the patients with EH have a pre-existing dermotosis such as atopic derma- titis.[1-7] Moreover, Lubbe J, et al. have noticed that EH had occurred during treatment of atopic dermatitis with 0.1% tacrolimus ointment.[9] In this case, there was no pre-existing dermatosis except varicella eruption. Moreover, the results of serology and Tzank smear were positive for HSV infection, so, it was accepted that EH had occurred due to HSV-reactivation after varicella infection. Anamnesis, physical and histological exami- C opyright © 2011 SciRes. OJPed  C. Celtik et al. / Open Journal of Pediatrics 1 (2011) 1-3 3 nations are usually adequate for th e diagnosis of the dis- turbances. Frequently, viral cultures and PCR-techniques are not necessary for the diagnosis, because these meth- ods are too expensive and not routine. Therefore, in this case, viral cultures and PCR- techniques have not been used. Physiopatology of this disease is described as a defect in T-cell mediated immunity and reduction of NK activity.6-10 In this case CD4/CD8 ratio had reversed, but immune defect could not be defined. If EH occurs due to HSV, usually it involves the face and ocular involvement may lead to blepharoconjunctiv- itis, keratitis and uveitis.[1,11,1 2] In this case, there was no ocular involvement, but his face was diseased. The therapy approach of this disease is primarily symptomatic and supportive. As an antiviral drug; acy- clovir should be used, corticosteroid therapy mustn’t be applied because the disease may worsen.[1-6] In this case, acyclovir, oxy de zinc pomade and eau borique solution were used. In addition, empiric antibiotherapy was us ed for the pre vention of s econd ary bacte rial infec- tions. These therapies had been very beneficial for this case and his lesions clearly regressed in one week. If corticosteroid therapy is used in these patients because of misdiagnosis, the lesions may worsen. Therefore, if skin lesions aggravate after varicella or another pre-existing dermatitis, EH must be consid- ered and antiviral therapy must be started, immedi- ately. REFERENCES [1] Stanberry LR. Herpes Simplex Virus. In Kliegman RM, Behrman RE, Jenson HB, Stanton BF, eds. Nelson Text- book of Pediatrics, 18th ed, Philadelphia; WB Saunders Co. 2007; 1360-1365. [2] Hill CO, Sterling JC, Kurtz JB. Viral infections. In Champion RH, Burton JL, Burns DA, Brethnach SM, eds. Textbook of Dermatology, 6th ed, London; Blackwell Science Ltd., 1998: 995-1095 [3] Brook I, Frazier EH, Yeager JK. Microbiology of in- fected eczema herpeticum. J Am Acad Dermatology 1995; 627-629 [4] Mooney MA, Janniger CK, Schwartz RA. Kaposi’s varicelliform eruption. Cutis 1994; 53: 243-245 [5] Kristal L, Klein PA. Atopic Dermatitis in Infant and Children. Pediatric Clinics of North America (Pediatric Dermatology) 2000; 47:877-895 [6] Crumpacker CS: Herpes simplex. In Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI et al, eds. Dermatology in General Medicine, 5th edition, Newyork; Mc Graw, 1999; 2414-2426 [7] Engler RJM, Kenner J, Leung DYM. Smallpox vaccina- tion: Risk considerations for patient with atopic dermati- tis. J Allergy Clin Immunol 2002; 110: 357-365. [8] Mackley CL, Adams DR, Anderson B, Miller JJ. Eczema herpeticum: a dermatolojic emergency. Dermatol Nurs 2002; 14: 307-310 [9] Lubbe J, Pournaras CC, Saurat JH. Eczema herpeticum during treatment of atopic dermatitis with 0.1% tac- rolimus ointment. Dermatology 2000; 201: 249-251 [10] Goodyear HM, McLeish P, Randall S. Immunological studies of herpes simplex virus infection in children with atopic eczema. Br J Dermatol 1996; 134: 85-93 [11] Fivenson DP, Breneman DL, Wander AH. Kaposi’s varicelliform eruption. Absence of ocular involvement. Arch Dermatol 1990; 126: 1037-1039 [12] Bestue M, Cordero A. Kaposi’s varicelliform eruption in a patient with healing peribucal dermabrasion. Dermatol Surg 2000; 26: 939-940. C opyright © 2011 SciRes. OJPed |

