Clinical Comparison of Pencil Beam Convolution and Clarkson Algorithms for Dose Calculation
1488
can be seen that the difference between Clarkson and
PBC algorithms for minimum, mean and maximum
doses was less than 1%. Wilcoxon test showed that there
was no statically significant difference, (p > 0.05). In
Table 2, it seems clearly that, the dose calculated for
OARs by Clarkson algorithm was higher than PBC algo-
rithm. The comparison of the dose constraints showed
that the recommendation for dose constraints in all OARs
were respected using the two algorithms.
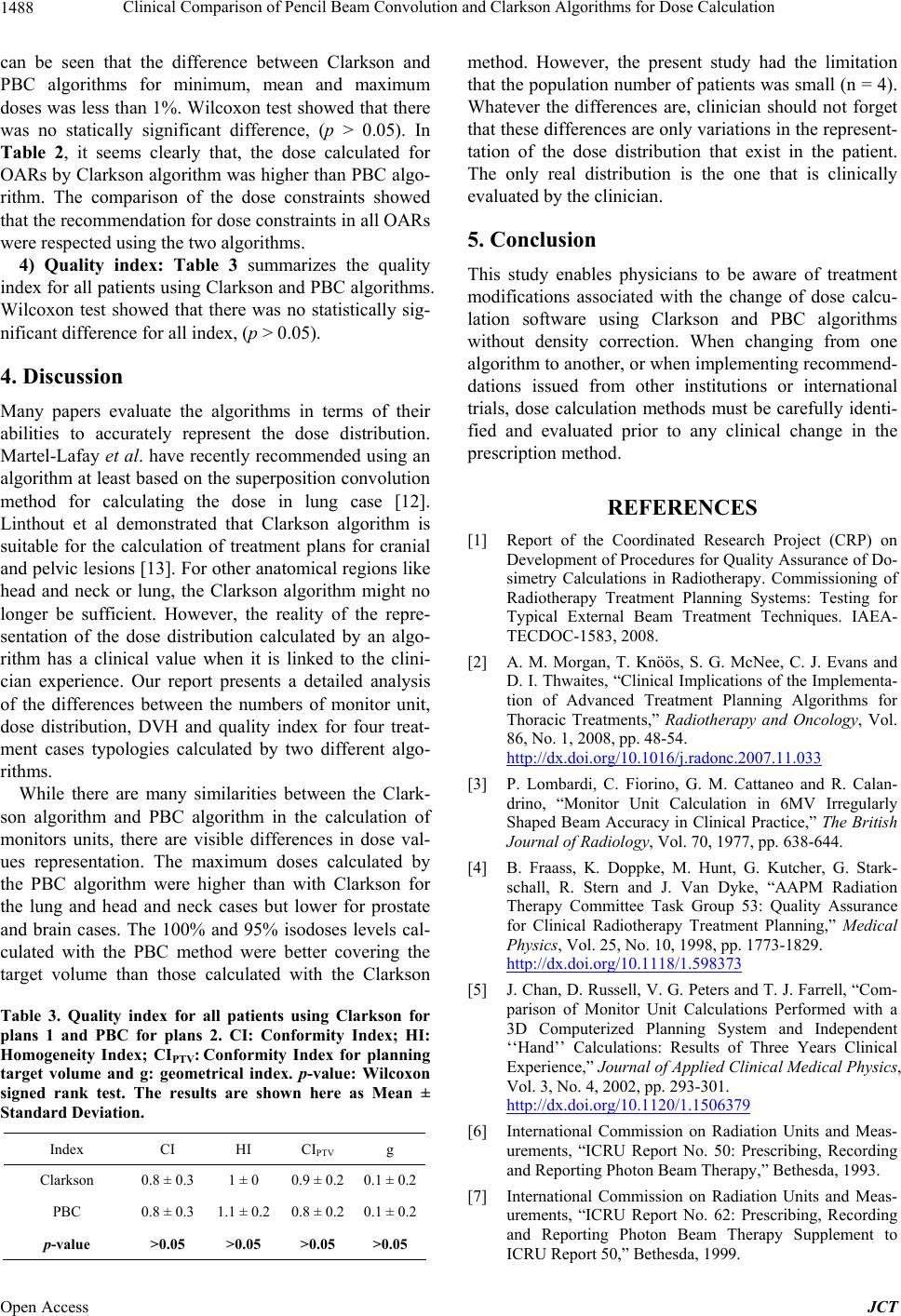
4) Quality index: Table 3 summarizes the quality
index for all patients using Clarkson and PBC algorithms.
Wilcoxon test showed that there was no statistically sig-
nificant difference for all index, (p > 0.05).
4. Discussion
Many papers evaluate the algorithms in terms of their
abilities to accurately represent the dose distribution.
Martel-Lafay et al. have recently recommended using an
algorithm at least based on the superposition convolution
method for calculating the dose in lung case [12].
Linthout et al demonstrated that Clarkson algorithm is
suitable for the calculation of treatment plans for cranial
and pelvic lesions [13]. For other anatomical regions like
head and neck or lung, the Clarkson algorithm might no
longer be sufficient. However, the reality of the repre-
sentation of the dose distribution calculated by an algo-
rithm has a clinical value when it is linked to the clini-
cian experience. Our report presents a detailed analysis
of the differences between the numbers of monitor unit,
dose distribution, DVH and quality index for four treat-
ment cases typologies calculated by two different algo-
rithms.
While there are many similarities between the Clark-
son algorithm and PBC algorithm in the calculation of
monitors units, there are visible differences in dose val-
ues representation. The maximum doses calculated by
the PBC algorithm were higher than with Clarkson for
the lung and head and neck cases but lower for prostate
and brain cases. The 100% and 95% isodoses levels cal-
culated with the PBC method were better covering the
target volume than those calculated with the Clarkson
Table 3. Quality index for all patients using Clarkson for
plans 1 and PBC for plans 2. CI: Conformity Index; HI:
Homogeneity Index; CIPTV: Conformity Index for planning
target volume and g: geometrical index. p-value: Wilcoxon
signed rank test. The results are shown here as Mean ±
Standard Deviation.
Index CI HI CIPTV g
Clarkson 0.8 ± 0.3 1 ± 0 0.9 ± 0.2 0.1 ± 0.2
PBC 0.8 ± 0.3 1.1 ± 0.2 0.8 ± 0.2 0.1 ± 0.2
p-value >0.05 >0.05 >0.05 >0.05
method. However, the present study had the limitation
that the population number of patients was small (n = 4).
Whatever the differences are, clinician should not forget
that these differences are only variations in the represent-
tation of the dose distribution that exist in the patient.
The only real distribution is the one that is clinically
evaluated by the clinician.
5. Conclusion
This study enables physicians to be aware of treatment
modifications associated with the change of dose calcu-
lation software using Clarkson and PBC algorithms
without density correction. When changing from one
algorithm to another, or when implementing recommend-
dations issued from other institutions or international
trials, dose calculation methods must be carefully identi-
fied and evaluated prior to any clinical change in the
prescription method.
REFERENCES
[1] Report of the Coordinated Research Project (CRP) on
Development of Procedures for Quality Assurance of Do-
simetry Calculations in Radiotherapy. Commissioning of
Radiotherapy Treatment Planning Systems: Testing for
Typical External Beam Treatment Techniques. IAEA-
TECDOC-1583, 2008.
[2] A. M. Morgan, T. Knöös, S. G. McNee, C. J. Evans and
D. I. Thwaites, “Clinical Implications of the Implementa-
tion of Advanced Treatment Planning Algorithms for
Thoracic Treatments,” Radiotherapy and Oncology, Vol.
86, No. 1, 2008, pp. 48-54.
http://dx.doi.org/10.1016/j.radonc.2007.11.033
[3] P. Lombardi, C. Fiorino, G. M. Cattaneo and R. Calan-
drino, “Monitor Unit Calculation in 6MV Irregularly
Shaped Beam Accuracy in Clinical Practice,” The British
Journal of Radiology, Vol. 70, 1977, pp. 638-644.
[4] B. Fraass, K. Doppke, M. Hunt, G. Kutcher, G. Stark-
schall, R. Stern and J. Van Dyke, “AAPM Radiation
Therapy Committee Task Group 53: Quality Assurance
for Clinical Radiotherapy Treatment Planning,” Medical
Physics, Vol. 25, No. 10, 1998, pp. 1773-1829.
http://dx.doi.org/10.1118/1.598373
[5] J. Chan, D. Russell, V. G. Peters and T. J. Farrell, “Com-
parison of Monitor Unit Calculations Performed with a
3D Computerized Planning System and Independent
‘‘Hand’’ Calculations: Results of Three Years Clinical
Experience,” Journal of Applied Clinical Medical Physics,
Vol. 3, No. 4, 2002, pp. 293-301.
http://dx.doi.org/10.1120/1.1506379
[6] International Commission on Radiation Units and Meas-
urements, “ICRU Report No. 50: Prescribing, Recording
and Reporting Photon Beam Therapy,” Bethesda, 1993.
[7] International Commission on Radiation Units and Meas-
urements, “ICRU Report No. 62: Prescribing, Recording
and Reporting Photon Beam Therapy Supplement to
ICRU Report 50,” Bethesda, 1999.
Open Access JCT