Anterior Cerebral Infarction by Fronto-Basal Meningioma
278
A B
C D
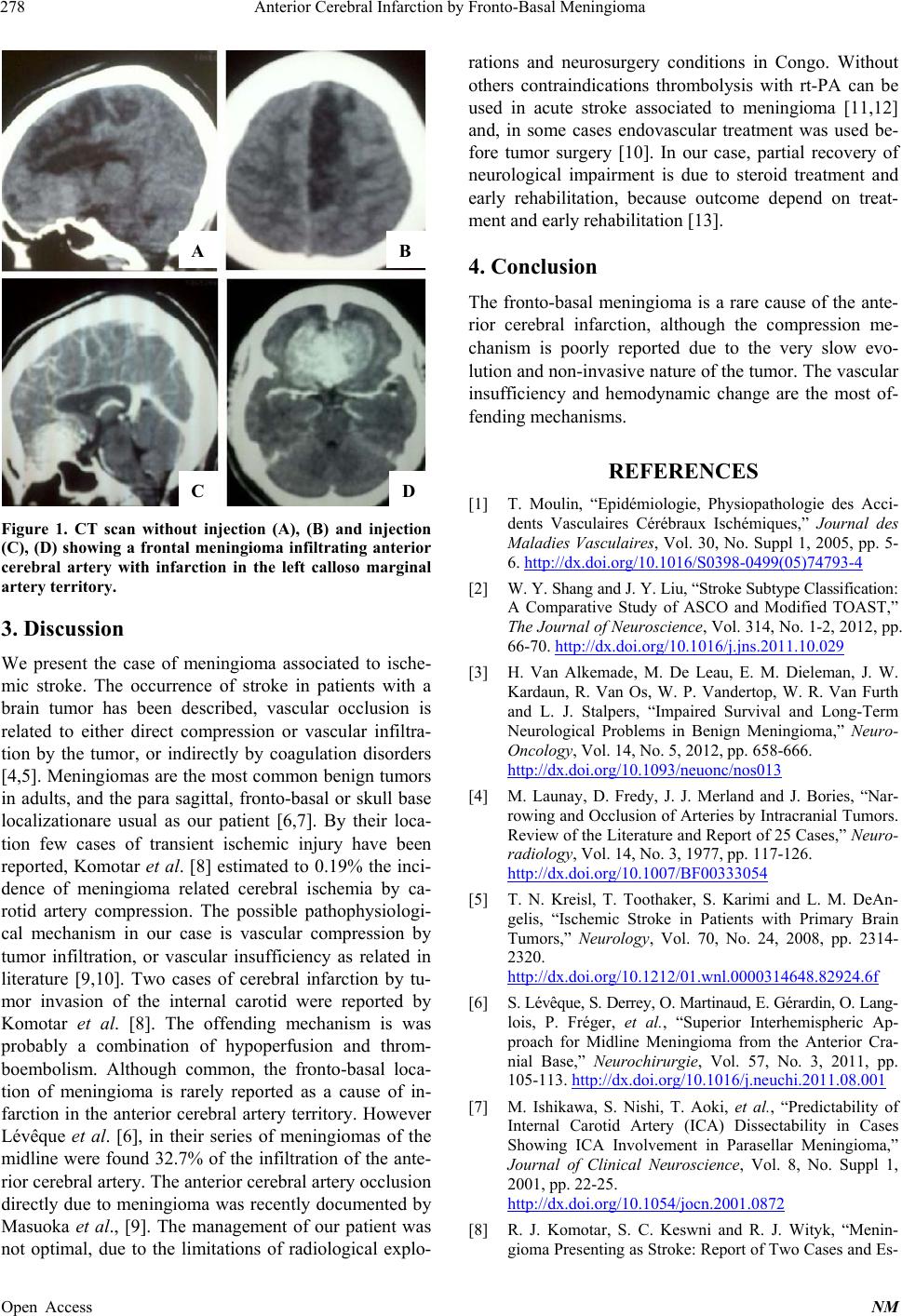
Figure 1. CT scan without injection (A), (B) and injection
(C), (D) showing a frontal meningioma infiltrating anterior
cerebral artery with infarction in the left calloso marginal
artery territory.
3. Discussion
We present the case of meningioma associated to ische-
mic stroke. The occurrence of stroke in patients with a
brain tumor has been described, vascular occlusion is
related to either direct compression or vascular infiltra-
tion by the tumor, or indirectly by coagulation disorders
[4,5]. Meningiomas are the most common benign tumors
in adults, and the para sagittal, fronto-basal or skull base
localizationare usual as our patient [6,7]. By their loca-
tion few cases of transient ischemic injury have been
reported, Komotar et al. [8] estimated to 0.19% the inci-
dence of meningioma related cerebral ischemia by ca-
rotid artery compression. The possible pathophysiologi-
cal mechanism in our case is vascular compression by
tumor infiltration, or vascular insufficiency as related in
literature [9,10]. Two cases of cerebral infarction by tu-
mor invasion of the internal carotid were reported by
Komotar et al. [8]. The offending mechanism is was
probably a combination of hypoperfusion and throm-
boembolism. Although common, the fronto-basal loca-
tion of meningioma is rarely reported as a cause of in-
farction in the anterior cerebral artery territory. However
Lévêque et al. [6], in their series of meningiomas of the
midline were found 32.7% of the infiltration of the ante-
rior cerebral artery. The anterior cerebral artery occlusion
directly due to meningioma was recently documented by
Masuoka et al., [9]. The management of our patient was
not optimal, due to the limitations of radiological explo-
rations and neurosurgery conditions in Congo. Without
others contraindications thrombolysis with rt-PA can be
used in acute stroke associated to meningioma [11,12]
and, in some cases endovascular treatment was used be-
fore tumor surgery [10]. In our case, partial recovery of
neurological impairment is due to steroid treatment and
early rehabilitation, because outcome depend on treat-
ment and early rehabilitation [13].
4. Conclusion
The fronto-basal meningioma is a rare cause of the ante-
rior cerebral infarction, although the compression me-
chanism is poorly reported due to the very slow evo-
lution and non-inv asive nature of th e tumor. The vascu lar
insufficiency and hemodynamic change are the most of-
fending mechanisms.
REFERENCES
[1] T. Moulin, “Epidémiologie, Physiopathologie des Acci-
dents Vasculaires Cérébraux Ischémiques,” Journal des
Maladies Vasculaires, Vol. 30, No. Suppl 1, 2005, pp. 5-
6. http://dx.doi.org/10.1016/S0398-0499(05)74793-4
[2] W. Y. Shang and J. Y. Liu, “Stroke Subtype Classification:
A Comparative Study of ASCO and Modified TOAST,”
The Journal of Neuroscience, Vol. 314, No. 1-2, 2012, pp.
66-70. http://dx.doi.org/10.1016/j.jns.2011.10.029
[3] H. Van Alkemade, M. De Leau, E. M. Dieleman, J. W.
Kardaun, R. Van Os, W. P. Vandertop, W. R. Van Furth
and L. J. Stalpers, “Impaired Survival and Long-Term
Neurological Problems in Benign Meningioma,” Neuro-
Oncology, Vol. 14, No. 5, 2012, pp. 658-666.
http://dx.doi.org/10.1093/neuonc/nos013
[4] M. Launay, D. Fredy, J. J. Merland and J. Bories, “Nar-
rowing and Occlusion of Arteries by Intracranial Tumors.
Review of the Literature and Report of 25 Cases,” Neuro-
radiology, Vol. 14, No. 3, 1977, pp. 117-126.
http://dx.doi.org/10.1007/BF00333054
[5] T. N. Kreisl, T. Toothaker, S. Karimi and L. M. DeAn-
gelis, “Ischemic Stroke in Patients with Primary Brain
Tumors,” Neurology, Vol. 70, No. 24, 2008, pp. 2314-
2320.
http://dx.doi.org/10.1212/01.wnl.0000314648.82924.6f
[6] S. Lévêque, S. Derrey , O. Mart inaud, E. Gérardin, O. Lang-
lois, P. Fréger, et al., “Superior Interhemispheric Ap-
proach for Midline Meningioma from the Anterior Cra-
nial Base,” Neurochirurgie, Vol. 57, No. 3, 2011, pp.
105-113. http://dx.doi.org/10.1016/j.neuchi.2011.08.001
[7] M. Ishikawa, S. Nishi, T. Aoki, et al., “Predictability of
Internal Carotid Artery (ICA) Dissectability in Cases
Showing ICA Involvement in Parasellar Meningioma,”
Journal of Clinical Neuroscience, Vol. 8, No. Suppl 1,
2001, pp. 22-25.
http://dx.doi.org/10.1054/jocn.2001.0872
[8] R. J. Komotar, S. C. Keswni and R. J. Wityk, “Menin-
gioma Presenting as Stroke: Report of Two Cases and Es-
Open Access NM