 Open Journal of Stomatology, 2013, 3, 31-36 OJST http://dx.doi.org/10.4236/ojst.2013.39A005 Published Online December 2013 (http://www.scirp.org/journal/ojst/) Assessment of alveolar defect volume in unilateral cleft lip and palate patients using a free software program Patricia Picolli1, Luciane Macedo de Menezes2*, Márcia Brucker 3, Fabiane Azeredo2, Susana Maria Deon Rizzatto2 1Private Practice, Porto Alegre, Brazil 2Department of Orthodontics, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil 3Department of Radiology, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil Email: *luciane.menezes@pucrs.br Received 11 September 2013; revised 19 October 2013; accepted 13 November 2013 Copyright © 2013 Patricia Picolli et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT The purpose of this study was to assess the alveolar defect volume in unilateral cleft lip and palate (UCLP) subjects using computed tomography (CT) and a free software program to evaluate the intra- and inter- rater measurements, and to compare the cleft volume between age and affected side. The sample of this retrospective study consisted of 20 UCLP individuals, 12 boys and 8 girls, mean age 10.3 ± 2.4 years at the beginning of orthodontic treatment. All subjects re- quired alveolar bone grafting. CT scans of the cleft area were obtained prior to secondary bone grafting, and were analyzed using Image J. software program. The cleft volume was calculated based on axial cross- sectional CT images by two raters (orthodontist and radiologist) and by the same rater (orthodontist) at two different moments. Linear mixed model, Bland- Altman, Pearson’s and intraclass correlation coeffi- cient (ICC) were used. The mean cleft volume was 7.53 ± 1.55 mm³. The intra- and inter-rater measure- ments were reproducible (ICC = 0.976 and 0.963, re- spectively) with no significant difference between them. There were no statistically significant differ- ences in the cleft volume related to age or cleft loca- tion. The assessment of cleft volume in UCLP using CT images and a free software program was a re- producible method. There was no significant relation between alveolar defect volume and age or cleft loca- tion. Keywords: Alveolar Process; Cleft Palate; Computed Tomography; Volumetric Assessment 1. INTRODUCTION Secondary bone grafting is considered the gold standard for repairing the cleft region [1]. It is indicated for most patients with an alveolar cleft, the best stage for this procedure is in the mixed dentition when the canine ad- jacent to the cleft has completed half to three quarters of its root formation [2]. Its major benefit is to restore al- veolar integrity to induce spontaneous migration of per- manent teeth adjacent to the cleft in the newly formed bone [3,4]. The outcome of the surgery is considered satisfactory when sufficient volume of normally remod- eled bone tissue is obtained [5]. Secondary bone grafting enhances the dental alveolus for eruption and periodontal support of the teeth adjacent to the cleft, usually the ca- nine and the lateral incisor [2,6,7]. This allows, through orthodontic treatment, the closing of the residual space, and in many cases it does not require rehabilitation with prosthesis or implants. Furthermore, the alveolar bone graft bridges the cleft defect with bone, providing an alar base support and allowing closure of the communication between the oral and n asal cavities [5,8,9]. Fresh autogenous bone is the ideal bone graft material because it supplies living immunocompatible bone cells essential to osteogenesis [10,11]. For optimum osteo- conductive, osteoinductive and osteogenic properties, autogenous cancellous bone from the ilium is preferred [12] due to the easy access and the large amount of bone tissue that can be obtained from this area [11,13]. How- ever, even though the iliac crest can produce an abundant amount of bone tissue for grafting [14], it is important to obtain an accurate estimation of the alveolar cleft volume and its architecture to determine the quantity of bone to be collected prior to the surgery and thus, to avoid in- adequate bone harvesting (reduced or excessive) as well as to reduce the postoperative morbidity of the donor *Corresponding a uthor. OPEN ACCESS 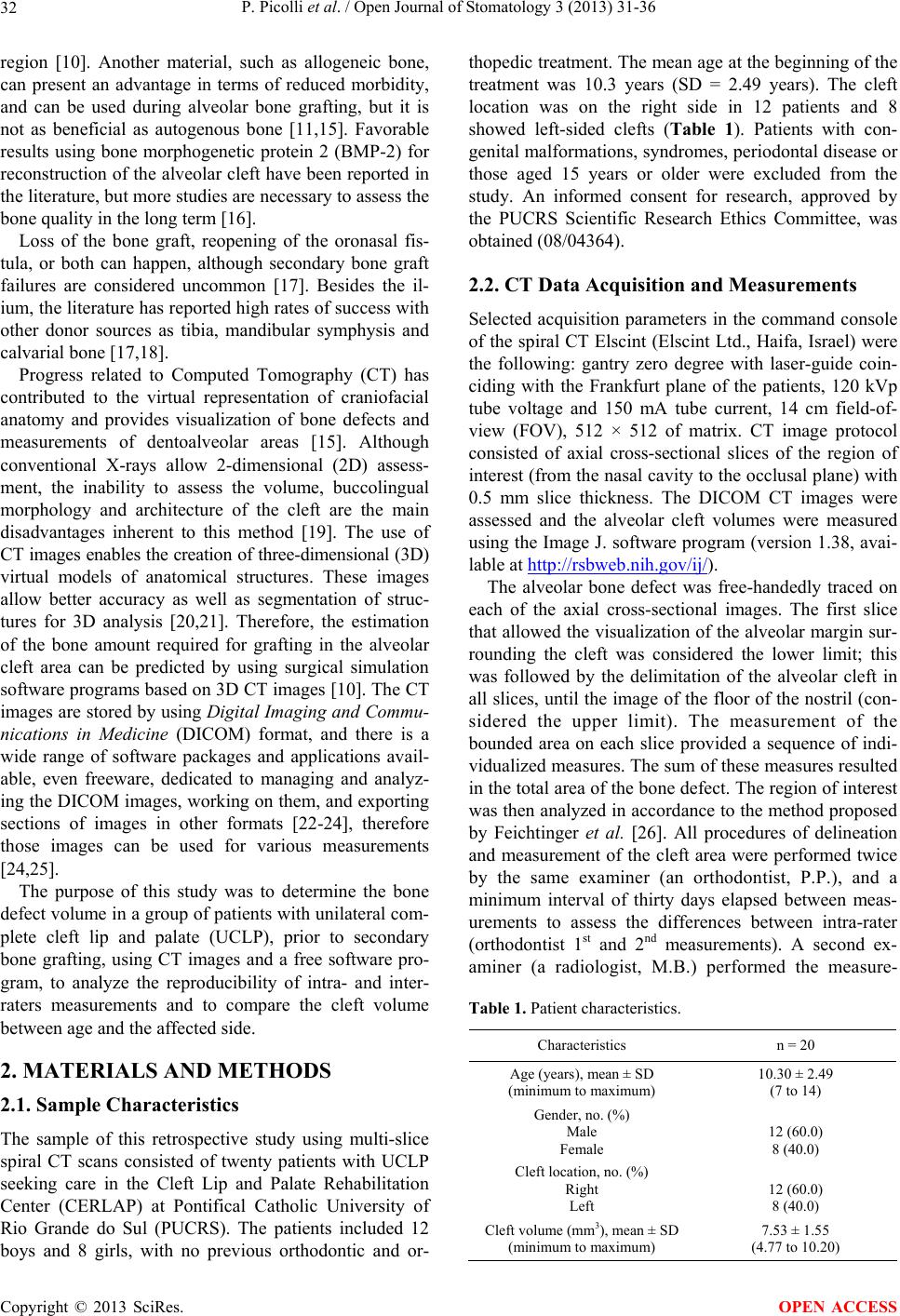 P. Picolli et al. / Open Journal of Stomatology 3 (2013) 31-36 32 region [10]. Another material, such as allogeneic bone, can present an advantage in terms of reduced morbidity, and can be used during alveolar bone grafting, but it is not as beneficial as autogenous bone [11,15]. Favorable results using bone morphogenetic protein 2 (BMP-2) for reconstruction of the alveolar cleft have been reported in the literature, but more studies are necessary to assess the bone quality in the long term [16]. Loss of the bone graft, reopening of the oronasal fis- tula, or both can happen, although secondary bone graft failures are considered uncommon [17]. Besides the il- ium, the literature has reported high rates of success with other donor sources as tibia, mandibular symphysis and calvarial bone [17,18]. Progress related to Computed Tomography (CT) has contributed to the virtual representation of craniofacial anatomy and provides visualization of bone defects and measurements of dentoalveolar areas [15]. Although conventional X-rays allow 2-dimensional (2D) assess- ment, the inability to assess the volume, buccolingual morphology and architecture of the cleft are the main disadvantages inherent to this method [19]. The use of CT images enables the creatio n of three-dimensional (3D) virtual models of anatomical structures. These images allow better accuracy as well as segmentation of struc- tures for 3D analysis [20,21]. Therefore, the estimation of the bone amount required for grafting in the alveolar cleft area can be predicted by using surgical simulation software programs based on 3D CT images [10]. The CT images are stored by using Digital Imaging and Commu- nications in Medicine (DICOM) format, and there is a wide range of software packages and applications avail- able, even freeware, dedicated to managing and analyz- ing the DICOM images, working on them, and exporting sections of images in other formats [22-24], therefore those images can be used for various measurements [24,25]. The purpose of this study was to determine the bone defect volume in a group of patients with unilateral com- plete cleft lip and palate (UCLP), prior to secondary bone grafting, using CT images and a free software pro- gram, to analyze the reproducibility of intra- and inter- raters measurements and to compare the cleft volume between age and the affected side. 2. MATERIALS AND METHODS 2.1. Sample Characteristics The sample of this retrospective study using multi-slice spiral CT scans consisted of twenty patients with UCLP seeking care in the Cleft Lip and Palate Rehabilitation Center (CERLAP) at Pontifical Catholic University of Rio Grande do Sul (PUCRS). The patients included 12 boys and 8 girls, with no previous orthodontic and or- thopedic treatment. The mean age at the beginning of the treatment was 10.3 years (SD = 2.49 years). The cleft location was on the right side in 12 patients and 8 showed left-sided clefts (Table 1). Patients with con- genital malformation s, syndromes, periodontal disease or those aged 15 years or older were excluded from the study. An informed consent for research, approved by the PUCRS Scientific Research Ethics Committee, was obtained ( 08/04364). 2.2. CT Data Acquisition and Measurements Selected acquisition parameters in the command console of the spiral CT Elscint (Elscint Ltd., Haifa, Israel) were the following: gantry zero degree with laser-guide coin- ciding with the Frankfurt plane of the patients, 120 kVp tube voltage and 150 mA tube current, 14 cm field-of- view (FOV), 512 × 512 of matrix. CT image protocol consisted of axial cross-sectional slices of the region of interest (from the nasal cavity to the occlusal plane) with 0.5 mm slice thickness. The DICOM CT images were assessed and the alveolar cleft volumes were measured using the Image J. software program (version 1.38, avai- lable at http://rsbweb.nih.gov/ij/). The alveolar bone defect was free-handedly traced on each of the axial cross-sectional images. The first slice that allowed the visualization of the alveo lar margin sur- rounding the cleft was considered the lower limit; this was followed by the delimitation of the alveolar cleft in all slices, until the image of the floor of the nostril (con- sidered the upper limit). The measurement of the bounded area on each slice provided a sequence of indi- vidualized measures. The sum of these measures resulted in the total area of the bone defect. The region of interest was then analyzed in accordance to the method proposed by Feichtinger et al. [26]. All procedures of delineation and measurement of the cleft area were performed twice by the same examiner (an orthodontist, P.P.), and a minimum interval of thirty days elapsed between meas- urements to assess the differences between intra-rater (orthodontist 1st and 2nd measurements). A second ex- aminer (a radiologist, M.B.) performed the measure- Table 1. Patient characteristics. Characteristics n = 20 Age (years), mean ± SD (minimum to maximum) 10.30 ± 2.49 (7 to 14) Gender, no. (%) Male Female 12 (60.0) 8 (40.0) Cleft location, no. (%) Right Left 12 (60.0) 8 (40.0) Cleft volume (mm3), mean ± SD (minimum to maximum) 7.53 ± 1.55 (4.77 to 10.20) Copyright © 2013 SciRes. OPEN ACCESS  P. Picolli et al. / Open Journal of Stomatology 3 (2013) 31-36 33 ments once and differences between inter-rater (ortho- dontist and radiologist) were evaluated. The examiners were blinded to perform the measurements. 2.3. Statistical Analysis Continuous data were described using mean, standard deviation, minimum and maximum values. Categorical data were presented as counts and percentages. To evaluate observer agreement (within and between com- ponents) it was initially calculated th e Pearson’s correla- tion coefficient. This approach was followed by the in- traclass correlation coefficient (ICC) and Bland-Alt- man’s plot with difference bias and 95% limits of agreement. The influence of selected factors (age and affected side) on cleft volume was explored using a lin- ear mixed model considering all three measurements available for each patient. Significance level was set at α = 0.05. Data were analyzed using SPSS version 18.0. 3. RESULTS The intra- and inter-rater measurements were reproduce- ble (ICC = 0.976 and 0.963, respectively) and compare- sons showed a strong association with no significant dif- ference among measurements (Figure 1). The mean volume corresponding to the initial alveolar defect of the cleft in this study was 7.53 ± 1.55 mm³, ranging from 4.77 to 10.20 mm³ (Table 1). Although no statistically significan t, the age presented a borderline significance (p = 0.097), and it could be an influent factor in the alveolar cleft volume. There was no statistically significant impact of the cleft side (right or left) on the cleft volume (p = 0.687). 4. DISCUSSION Secondary bone grafting is an essential step in alveolar deformity reconstruction in cleft lip and palate (CLP) patients [17]. In addition to the benefits recognized in creating bone suppo rt for tooth eruption [15,2 7], second- dary bone grafting allows the elimination of oronasal fistulae, improves oral hygiene by separating the dental and nasal cavities, rebuilds the hypoplastic pyriform ap- erture [17] and the soft tissue of the nasal base support [28], and stabilizes the maxillary arch [29], thus provid- ing a suitable volume of bone to allow dental movement and subsequent residual space closure in the cleft region [30]. The recognition of the initial size of the alveolar defect and the use of reproducible measurement methods are essential factors in studies that evaluate the stability of alveolar grafting [16]. The measurements in this study presented excellent examiner repeatability (Figure 1), and the mean volume corresponding to the preoperative alveolar defect was 7.53 ± 1.55 mm³ (Table 1). Other studies reported higher mean volumes of the alveolar defects (11.0 to 38.0 mm³) [10,26,30-32]. However, previous orthopedic procedures were not mentioned in those researches. In the present study, the sample consisted of patients with no previous orthodontic and orthopedic procedures when the CT scans were taken. Therefore, the difference among cleft volume values could be explained by the maxillary ex- pansion and orthopedic protraction performed to correct the sagittal and transverse deficiency [33,34], usually performed before the secondary bone graft [35]. In a study based on radiographs, Aurouze et al. [36] reported that there was no correlation between the alveo- lar cleft size and the success in secondary alveolar graft- ing. However, van der Meij et al. [37] evaluating this topic on CT scans, indicated that there could be a posi- tive correlation (i.e., bigger clefts would be more prone to have alveolar graft resorption due to insufficient vas- cularization of progenitor cells in the center of the bone graft) [38]. According to Shirota et al. [10] it is impor- tant to understand the architecture of the alveolar defect in the cleft area and to assess its volume using CT im- ages prior to the surgical procedure to obtain the correct volume necessary for bone grafting. Although CT is still used in situations when 3D information is required, do- simetry studies demonstrated that the absorbed and ef- fective doses of spiral and conventional CT were higher than that using cone beam CT (CBCT) [39-41]. Fur- thermore, the CBCT technology has other advantages over CT such as lower cost, shorter acquisition time, better resolution, greater detail, being more appropriate for dentistry [42-47]. However, spiral CT was used in this retrospective study because the access to CBCT scanners in the early 2000’s (when the cleft patients’ data were acquired) was difficult. For alveolar defect repair, autogenous bone can be harvested from intraoral sites (limited to the amount of bone available), such as the mandibular symphysis, retromolar pad, mandibular ramus, tuberosity and zygo- matic buttress, and from extraoral sites, such as the tibia, and iliac crest [48]. Although the iliac crest can provide an abundant bone amount for grafting [14], the preopera- tive computer simulation and assessment of the 3D al- veolar cleft volume using CT images can avoid the in- adequate harvest of bone as well as reducing the postop- erative morbidity of the donor region [10]. This can pre- vent some of the possible surgical complications such as excessive blood loss, delayed wound healing, pain and hypoesthesia [49]. The mandibular symphysis, an in- traoral donor site with a reduced morbidity, is not a do- nor area that provides sufficient volume of cancellous bone [48] to fill in all kinds of alveolar cleft defects. Thus, it is essential to assess the cleft dimensions to se- lect the adequate donor site and harvest the needed amount of bone for the alveolar graft [50]. Copyright © 2013 SciRes. OPEN ACCESS  P. Picolli et al. / Open Journal of Stomatology 3 (2013) 31-36 Copyright © 2013 SciRes. 34 Figure 1. Linear scatter and Bland-Altman plots for the comparison among observers. Due to the popularizatio n of 3D imaging as a means to assist in dental diagnosis, this study assessed its clinical applicability using a public domain software program. It was possible to delimitate the alveolar bone defect in the cleft region, as well as to obtain its respective measure- ments in CT slices [51-53]. Considering the lack of spe- cific researches in the literature regarding the applicabil- ity of free software programs for the evaluation of bone deformity in cleft patients, this study showed a repro- ducible method to assess and measure the alveolar cleft volume. OPEN ACCESS 5. CONCLUSIONS In this study, the assessment as well as measurements in cleft patients using CT images and a free software pro- gram was a reproducible method. There was no significant relation between the alveolar defect volume with age or cleft location in UCLP. REFERENCES [1] Clavijo-Alvarez, J., Vecchione, L., De Cesare, G., Irwin, C., Smith, M., Grunwaldt, M. and Losee, J. (2010) Auto- logous bone grafting with adjunctive use of acellular der- mal matrix for alveolar cleft defects: early outcomes. The Cleft Palate-Craniofacial Journal, 47, 116-121. http://dx.doi.org/10.1597/09-029.1 [2] Rocha, R., Ritter, D.E., Locks, A., de Paula, L.K. and Santana, R.M. (2012) Ideal treatment protocol for cleft lip and palate patient from mixed to permanent dentition. American Journal of Orthodontics and Dentofacial Or- thopedics, 141, 1 40 -1 48 . http://dx.doi.org/10.1016/j.ajodo.2011.03.024 [3] Osawa, T., Omura, S., Fukuyama, E., Matsui, Y., Torikai, K. and Fujita, K. (2007) Factors influencing secondary alveolar bone grafting in cleft lip and palate patients: pro- spective analysis using CT image analyzer. The Cleft Palate-Craniofacial Journal, 44, 286-291. http://dx.doi.org/10.1597/06-054 [4] Oberoi, S., Chigurupati, R., Gill, P., Hoffman, W. and Vargervik, K. (2009) Volumetric assessment of second- dary alveolar bone grafting using cone beam computed tomography. The Cleft Palate-Craniofacial Journal, 46, 503-511. http://dx.doi.org/10.1597/08-153.1 [5] Rychlik, D. and Wojcicki, P. (2012) Bone graft healing in alveolar osteoplasty in patients with unilateral lip, alveo- lar process, and palate clefts. The Journal of Craniofacial Surgery, 23, 118-123. http://dx.doi.org/10.1097/SCS.0b013e318240faa0 [6] Silva Filho, O.G., Teles, S.G., Ozawa, T.O. and Cape-  P. Picolli et al. / Open Journal of Stomatology 3 (2013) 31-36 35 lozza Filho, L. (2000) Secondary bone graft and eruption of the permanent canine in patients with alveolar clefts: Literature review and case report. The Angle Orthodontist, 70, 174-178. [7] Russell, K.A. and McLeod, C.E. (2008) Canine eruption in patients with complete cleft lip and palate. The Cleft Palate-Craniofacial Journal, 45, 73-80. http://dx.doi.org/10.1597/07-049.1 [8] So, L.Y. and Lui, W.K. (1996) Alternative donor site for alveolar bone grafting in adults with cleft lip and palate. The Angle Orthodontist, 66, 9-16. [9] Offert, B., Janiszewska-Olszowska, J., Dudkiewicz, Z., Brudnicki, A., Katsaros, C. and Fudalej, P.S. (2013) Fa- cial esthetics in children with unilateral cleft lip and pal- ate 3 years after alveolar bone grafting combined with rhinoplasty between 2 and 4 years of age. Orthodontics and Craniofacial Research, 16, 36-43. h tt p: //d x. do i. org/ 10. 1111/ oc r.1 200 2 [10] Shirota, T., Kurabayashi, H., Ogura, H., Seki, H., Maki, K. and Shintani, S. (2010) Analysis of bone volume using computer simulation system for secondary bone graft in alveolar cleft. International Journal of Oral and Maxil- lofacial Surgery, 39, 904-908. http://dx.doi.org/10.1016/j.ijom.2010.04.050 [11] Walia, A. (2011) Secondary alveolar bone grating in cleft lip and palate patients Contemporary Clinical Dentistry, 21, 146-154. [12] Missiuna, P.C., Gandhi, H.S., Farrokhyar, F., Dore, E.M.G. and Roberts, B. (2011) Anatomically safe and minimally invasive transcrestal technique for procurement of auto- genous cancellous bone graft from the mid-iliac crest. Journal Canadien de Chirurgie, 54, 327-332. http://dx.doi.org/10.1503/cjs.028010 [13] Boyne, P.J. and Sands, N.R. (1972) Secondary bone grafting of residual alveolar and palatal clefts. Journal of Oral Surgery, 30, 87-92. [14] McIntyre, G. and Devlin, M. (2010) Secondary alveolar bone grafting (CLEFTSiS) 2000-2004. The Cleft Pal- ate-Craniofacial Journal, 47, 66-72. http://dx.doi.org/10.1597/08-165.1 [15] Goudy, S., Lott, D., Burton, R., Wheeler, J. and Canady, J. (2009) Secondary alveolar bone grafting: Outcomes, revisions and new applications. The Cleft Palate-Cra- niofacial Journal, 46, 610-612. http://dx.doi.org/10.1597/08-126.1 [16] Van Hout, W., van der Molen, A., Breugem, C.C. and Koole, R. (2011) Reconstruction of the alveolar cleft: Can growth factor-aided tissue engineering replace auto- logous bone grafting? A literature review and systematic review of results obtained with bone morphogenetic pro- tein-2. Clinical Oral Investigations, 15, 297-303. http://dx.doi.org/10.1007/s00784-011-0547-6 [17] Eppley, B. and Sadove, A. (2000) Management of alveo- lar cleft bone grafting—State of the art. The Cleft Pal- ate-Craniofacial Journal, 37, 229-233. http://dx.doi.org/10.1597/1545-1569(2000)037<0229:MO ACBG>2.3.CO;2 [18] Wolfe, S.A. and Berkowitz, S. (1983) The use of cranial bone grafts in the closure of alveolar and palatal clefts. Plastic and Reconstructive Surgery, 72, 659-666. http://dx.doi.org/10.1097/00006534-198311000-00013 [19] Kim, K., Kim, S. and Baek, S. (2008) Change in grafted secondary alveolar bone in patients with UCLP and UCLA. A three-dimensional computed tomography study. The Angle Orthodontist, 78, 631-640. http://dx.doi.org/10.2319/0003-3219(2008)078[0631:CIG SAB]2.0.CO;2 [20] Cavalcanti, M., Rocha, S. and Vannier, W. (2004) Cra- niofacial measurements based on 3D-CT volume render- ing: Implications for clinical applications. Dentomaxillo- facial Radiology, 33, 170-176. http://dx.doi.org/10.1259/dmfr/13603271 [21] Moreira, C., Sales, M., Lopes, P. and Cavalcanti, M. (2009) Assessment of linear and angular measurements on three-dimensional cone-beam computed tomographic images. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 108, 430-436. http://dx.doi.org/10.1016/j.tripleo.2009.01.032 [22] Grauer, D., Cevidanes, L.S. and Proffit, W.R. (2009) Working with DICOM craniofacial images. American Journal of Orthodontics and Dentofacial Orthopedics, 136, 460-470. http://dx.doi.org/10.1016/j.ajodo.2009.04.016 [23] Gibaud, B. (2011) The quest for standards in medical imaging. European Journal of Radiology, 78, 190-198. http://dx.doi.org/10.1016/j.ejrad.2010.05.003 [24] Spin-Neto, R., Marcantonio Jr., E., Gotfredsen, E. and Wenzel, A. (2011) Exploring CBCT-based DICOM files: A systematic review on the properties of images used to evaluate maxillofacial bone grafts. Journal of Digital Imaging, 24, 959-966. http://dx.doi.org/10.1007/s10278-011-9377-y [25] De Vos, W., Cas selman, J. and Swennen, G. (2009) Co ne- beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. International Journal of Oral and Maxillofa- cial Surgery, 38, 609-625. http://dx.doi.org/10.1016/j.ijom.2009.02.028 [26] Feichtinger, M., Mossböck, R. and Kärcher, H. (2007) Assessment of bone resorption after secondary alveolar bone grafting using three-dimensional computed tomo- graphy: A three-year study. The Cleft Palate-Craniofacial Journal, 44, 142-148. http://dx.doi.org/10.1597/06-047.1 [27] Oberoi, S., Gill, P., Chigurupati, R., Hoffman, W., Hat ch er, D. and Vargervik, K. (2010) Three-dimensional assess- ment of the eruption path of the canine in individuals with bone-grafted alveolar clefts using cone beam com- puted tomography. The Cleft Palate-Craniofacial Journal, 47, 507-512. http://dx.doi.org/10.1597/08-171 [28] Nagasao, T., Ogata, H., Miya moto, J., Jiang, H., Kaneko, T. and Ishiki, Y. (2009) Alveolar bone grafting for pa- tients with unilateral complete alveolar and palatal clefts improves the bony structure of the nose. The Cleft Pal- ate-Craniofacial Journal, 46, 9-18. http://dx.doi.org/10.1597/07-169.1 [29] Bohman, P., Yamashita, D., Baek, S. and Yen, S. (2004) Stabilization of an edentulous premaxilla for an alveolar bone graft: Case report. The Cleft Palate-Craniofacial Copyright © 2013 SciRes. OPEN ACCESS  P. Picolli et al. / Open Journal of Stomatology 3 (2013) 31-36 Copyright © 2013 SciRes. 36 OPEN ACCESS Journal, 41, 214-217. http://dx.doi.org/10.1597/03-009 [30] Feichtinger, M., Mossböck, R. and Kärcher, H. (2006) Evaluation of bone volume following bone grafting in pa- tients with unilateral clefts of lip, alveolus and palate us- ing a CT-guided three-dimensional navigation system. Journal of Cranio-Maxillofacial Surgery, 34, 144-149. http://dx.doi.org/10.1016/j.jcms.2005.11.005 [31] Honma, K., Kobayashi, T., Nakajima, T. and Hayasi, T. (1999) Computed tomographic evaluation of bone forma- tion after secondary bone grafting of alveolar clefts. Journal of Oral and Maxillofacial Surgery, 57, 1209- 1213. http://dx.doi.org/10.1016/S0278-2391(99)90488-3 [32] Feichtinger, M., Zemann, W., Mossböck, R. and Kärcher, H. (2008) Three-dimensional evaluation of secondary al- veolar bone grafting using a 3D-navigation system based on computed tomography: A two-year follow-up. British Journal of Oral and Maxillofacial Surgery, 46, 278-282. http://dx.doi.org/10.1016/j.bjoms.2007.12.010 [33] Silva Filho, O.G., Boiani, E., Cavassan, A. and San- tamaria Jr., M. (2009) Rapid maxillary expansion after secondary alveolar bone grafting in patients with alveolar cleft. The Cleft Palate-Craniofacial Journal, 46, 331-338. http://dx.doi.org/10.1597/07-205.1 [34] Vieira, G., Menezes, L.M., Lima, E.M.S. and Rizzatto, S.M.D. (2009) Dentoskeletal effects of maxillary protrac- tion in cleft patients with repetitive weekly protocol of alternate rapid maxillary expansions and constrictions. The Cleft Palate-Craniofacial Journal, 46, 391-398. http://dx.doi.org/10.1597/07-144.1 [35] Menezes, L.M., Azeredo, F., Weissheimer, A., Rizzato, J.L. and Rizzatto, S.M.D. (2012) Cone-beam computed tomography evaluation of maxillary expansion in twins with cleft lip and palate. Dental Press Journal of Ortho- dontics, 17, 1-11. [36] Aurouze, C., Moller, K., Bevis, R., Rehm, K. and Rudney, J. (2000) The presurgical status of the alveolar cleft and success of secondary bone grafting. The Cleft Palate- Craniofacial Journal, 37, 179-184. http://dx.doi.org/10.1597/1545-1569(2000)036<0179:TP SOTA>2.3.CO;2 [37] Van der Meij, A., Baart, J., Prahl-Andersen, B., Valk, J. and Kontense, P. (2001) Bone volume after secondary bone grafting in unilateral and bilateral clefts determined by computed tomography scans. Oral Surgery, Oral Me- dicine, Oral Pathology, Oral Radiology, and Endodon- tology, 92, 136-141. http://dx.doi.org/10.1067/moe.2001.115274 [38] Long Jr., R., Spangler, B. and Yow, M. (1995) Cleft width and secondary alveolar bone success. The Cleft Palate-Craniofacial Journal, 32, 420-427. http://dx.doi.org/10.1597/1545-1569(1995)032<0420:CW ASAB>2.3.CO;2 [39] Kim, S.Y., Han, J.W. and Park, I.W. (2008) Comparison of cone beam CT and conventional CT in absorned and effective dose. Korean Journal of Oral and Maxillofacial Radiology, 38, 7-15. [40] Hirsch, E., Wolf, U., Heinicke, F. and Silva, M.A. (2008) Dosimetry of the cone beam computed tomography ve- raviewepocs 3D compared with the 3D accuitomo in dif- ferent fields of view. Dentomaxillofacial Radiology, 37, 268-273. http://dx.doi.org/10.1259/dmfr/23424132 [41] Chau, A.C. and Fung, K. (2009) Comparison of radiation dose for implant imaging using conventional spiral to- mography, computed tomography, and cone-beam com- puted tomography. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 107, 559- 565. http://dx.doi.org/10.1016/j.tripleo.2008.11.009 [42] Mah, J.K. and Hatcher, D. (2004) Three-dimensional craniofacial imaging. American Journal of Orthodontics and Dentofacial Orthopedics, 126, 308-309. http://dx.doi.org/10.1016/j.ajodo.2004.06.024 [43] Almog, D.M. and Romano, P.R. (2007) CT-based dental imaging for implant planning and surgical guidance. The New York State Dental Journal, 73, 51-53. [44] Silva, M.A.G., Wolf, U., Heinicke, F., Bumann, A., Vis- ser, H. and Hirsch, E. (2008) Cone-beam computed to- mography for routine orthodontic treatment planning: A radiation dose evaluation. American Journal of Ortho- dontics and Dentofacial Orthopedics, 133, e1-e5. [45] Ludlow, J.B. and Ivanovic, M. (2008) Comparative do- simetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 106, 106-114. http://dx.doi.org/10.1016/j.tripleo.2008.03.018 [46] Quereshy, F.A., Savell, T.A. and Palomo, J.M. (2008) Applications of cone beam computed tomography in the practice of oral and maxillofacial surgery. Journal of Oral and Maxillofacial Surgery, 66, 791-796. http://dx.doi.org/10.1016/j.joms.2007.11.018 [47] Katsumata, A., Hirukawa, A., Okumura, S., Naitoh, M., Fujishita, M., Ariji, E. and Langlais, R.P. (2009) Rela- tionship between density variability and imaging volume size in cone-beam computerized tomographic scanning of the maxillofacial region: an in vitro study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and En- dodontology, 107, 420-425. http://dx.doi.org/10.1016/j.tripleo.2008.05.049 [48] Mikoya, T., Inoue, N., Matsuzawa, Y., Totsuka, Y. and Kajii, T. (2010) Monocortical mandibular bone grafting for reconstruction of alveolar cleft. The Cleft Palate- Craniofacial Journal, 47, 454-468. http://dx.doi.org/10.1597/09-172 [49] Lilja, J. (2003) Cleft lip and palate surgery. Scandinavian Journal of Surgery, 92, 269-273. [50] Zouhary, A. (2010) Bone graft harvesting from distant sites: concepts and techniques. Oral and Maxillofacial Surgery Clinics of North America, 22, 301-316. http://dx.doi.org/10.1016/j.coms.2010.04.007 [51] Abramoff, M., Magalhaes, P. and Ram, S. (2004) Image processing with image J. Biophotonics International, 11, 36-42. [52] Barboriak, D.P., Padua, A.O., York, G.E. and Macfall, J.R. (2005) Creation of DICOM-aware applications using image J. Journal of Digital Imaging, 18, 91-99. http://dx.doi.org/10.1007/s10278-004-1879-4 [53] Rasband, W. (2008) Image J. US National Institutes of Health, Bethesda. http://rsb.info.nih.gov/ij
|