S. R. JAHROMI ET AL.
Open Access 3
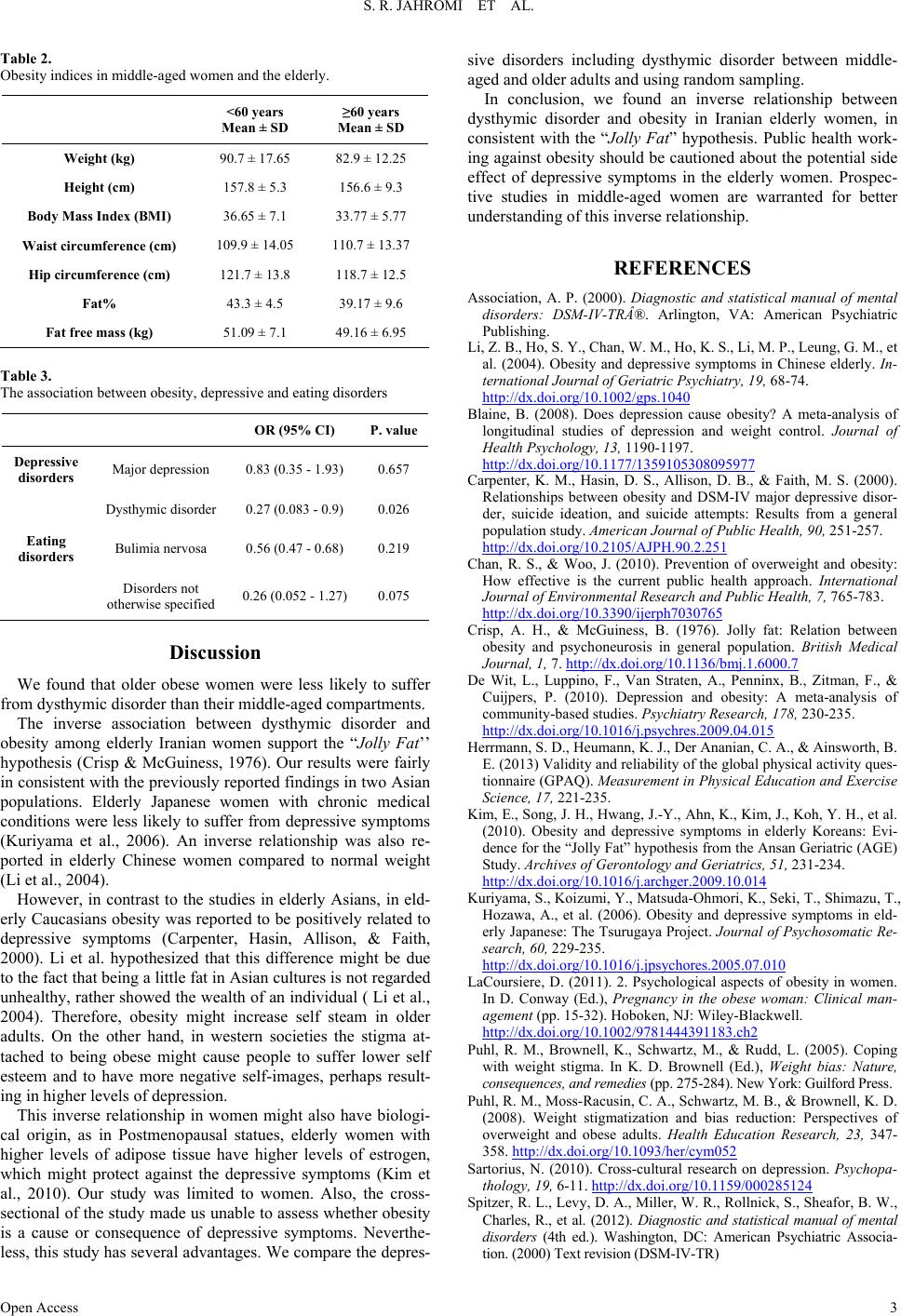
Table 2.
Obesity indices in middle-aged women and the elderly.
<60 years
Mean ± SD
≥60 years
Mean ± SD
Weight (kg) 90.7 ± 17.65 82.9 ± 12.25
Height (cm) 157.8 ± 5.3 156.6 ± 9.3
Body Mass Index (BMI) 36.65 ± 7.1 33.77 ± 5.77
Waist circumference (cm) 109.9 ± 14.05 110.7 ± 13.37
Hip circumference (cm) 121.7 ± 13.8 118.7 ± 12.5
Fat% 43.3 ± 4.5 39.17 ± 9.6
Fat free mass (kg) 51.09 ± 7.1 49.16 ± 6.95
Table 3.
The association between obesity, depressive and eating disorders
OR (95% CI) P. value
Depressive
disorders Major depression 0.83 (0.35 - 1.93) 0.657
Dysthymic disorder 0.27 (0.083 - 0.9) 0.026
Eating
disorders Bulimia nervosa 0.56 (0.47 - 0.68) 0.219
Disorders not
otherwise specified 0.26 (0.052 - 1.27) 0.075
Discussion
We found that older obese women were less likely to suffer
from dysthymic disorder than their middle-aged compartments.
The inverse association between dysthymic disorder and
obesity among elderly Iranian women support the “Jolly Fat’’
hypothesis (Crisp & McGuiness, 1976). Our results were fairly
in consistent with the previously reported findings in two Asian
populations. Elderly Japanese women with chronic medical
conditions were less likely to suffer from depressive symptoms
(Kuriyama et al., 2006). An inverse relationship was also re-
ported in elderly Chinese women compared to normal weight
(Li et al., 2004).
However, in contrast to the studies in elderly Asians, in eld-
erly Caucasians obesity was reported to be positively related to
depressive symptoms (Carpenter, Hasin, Allison, & Faith,
2000). Li et al. hypothesized that this difference might be due
to the fact that being a little fat in Asian cultures is not regarded
unhealthy, rather showed the wealth of an individual ( Li et al.,
2004). Therefore, obesity might increase self steam in older
adults. On the other hand, in western societies the stigma at-
tached to being obese might cause people to suffer lower self
esteem and to have more negative self-images, perhaps result-
ing in higher levels of depression.
This inverse relationship in women might also have biologi-
cal origin, as in Postmenopausal statues, elderly women with
higher levels of adipose tissue have higher levels of estrogen,
which might protect against the depressive symptoms (Kim et
al., 2010). Our study was limited to women. Also, the cross-
sectional of the study made us unable to assess whether obesity
is a cause or consequence of depressive symptoms. Neverthe-
less, this study has several advantages. We compare the depres-
sive disorders including dysthymic disorder between middle-
aged and older adults and using random sampling.
In conclusion, we found an inverse relationship between
dysthymic disorder and obesity in Iranian elderly women, in
consistent with the “Jolly Fat” hypothesis. Public health work-
ing against obesity should be cautioned about the potential side
effect of depressive symptoms in the elderly women. Prospec-
tive studies in middle-aged women are warranted for better
understanding of this inverse relationship.
REFERENCES
Association, A. P. (2000). Diagnostic and statistical manual of mental
disorders: DSM-IV-TR®. Arlington, VA: American Psychiatric
Publishing.
Li, Z. B., Ho, S. Y., Chan, W. M., Ho, K. S., Li, M. P., Leung, G. M., et
al. (2004). Obesity and depressive symptoms in Chinese elderly. In-
ternational Journal of Ge r i at r ic Psychiatry, 19, 68-74.
http://dx.doi.org/10.1002/gps.1040
Blaine, B. (2008). Does depression cause obesity? A meta-analysis of
longitudinal studies of depression and weight control. Journal of
Health Psychology, 13, 1190-1197.
http://dx.doi.org/10.1177/1359105308095977
Carpenter, K. M., Hasin, D. S., Allison, D. B., & Faith, M. S. (2000).
Relationships between obesity and DSM-IV major depressive disor-
der, suicide ideation, and suicide attempts: Results from a general
population study. American Journal of Public Health, 90, 251-257.
http://dx.doi.org/10.2105/AJPH.90.2.251
Chan, R. S., & Woo, J. (2010). Prevention of overweight and obesity:
How effective is the current public health approach. International
Journal of Environmental R esearch and Public Health, 7, 765-783.
http://dx.doi.org/10.3390/ijerph7030765
Crisp, A. H., & McGuiness, B. (1976). Jolly fat: Relation between
obesity and psychoneurosis in general population. British Medical
Journal, 1, 7. http://dx.doi.org/10.1136/bmj.1.6000.7
De Wit, L., Luppino, F., Van Straten, A., Penninx, B., Zitman, F., &
Cuijpers, P. (2010). Depression and obesity: A meta-analysis of
community-based studies. Psychiatry Research, 178, 230-235.
http://dx.doi.org/10.1016/j.psychres.2009.04.015
Herrmann, S. D., Heumann, K. J., Der Ananian, C. A., & Ainsworth, B.
E. (2013) Validity and reliability of the global physical activity ques-
tionnaire (GPAQ). Measurement in Physical Education and Exercise
Science, 17, 221-235.
Kim, E., Song, J. H., Hwang, J.-Y., Ahn, K., Kim, J., Koh, Y. H., et al.
(2010). Obesity and depressive symptoms in elderly Koreans: Evi-
dence for the “Jolly Fat” hypothesis from the Ansan Geriatric (AGE)
Study. Archives of Gerontology and Geriatrics, 51, 231-234.
http://dx.doi.org/10.1016/j.archger.2009.10.014
Kuriyama, S., Koizumi, Y., Matsuda-Ohmori, K., Seki, T., Shimazu, T.,
Hozawa, A., et al. (2006). Obesity and depressive symptoms in eld-
erly Japanese: The Tsurugaya Project. Journal of Psychosomatic Re-
search, 60, 229-235.
http://dx.doi.org/10.1016/j.jpsychores.2005.07.010
LaCoursiere, D. (2011). 2. Psychological aspects of obesity in women.
In D. Conway (Ed.), Pregnancy in the obese woman: Clinical man-
agement (pp. 15-32). Hoboken, NJ: Wiley-Blackwell.
http://dx.doi.org/10.1002/9781444391183.ch2
Puhl, R. M., Brownell, K., Schwartz, M., & Rudd, L. (2005). Coping
with weight stigma. In K. D. Brownell (Ed.), Weight bias: Nature,
consequences, and remedies (pp. 275-284). New York: Guilford Press.
Puhl, R. M., Moss-Racusin, C. A., Schwartz, M. B., & Brownell, K. D.
(2008). Weight stigmatization and bias reduction: Perspectives of
overweight and obese adults. Health Education Research, 23, 347-
358. http://dx.doi.org/10.1093/her/cym052
Sartorius, N. (2010). Cross-cultural research on depression. Psychopa-
thology, 19, 6-11. http://dx.doi.org/10.1159/000285124
Spitzer, R. L., Levy, D. A., Miller, W. R., Rollnick, S., Sheafor, B. W.,
Charles, R., et al. (2012). Diagnostic and statistical manual of mental
disorders (4th ed.). Washington, DC: American Psychiatric Associa-
tion. (2000) Text revision (DSM-IV-TR)