Journal of Cancer Therapy
Vol.5 No.9(2014), Article ID:49179,15 pages
DOI:10.4236/jct.2014.59093
Effect of Inhaled Tiotropium as the Perioperative Management of Patients Undergoing Pulmonary Resection for Primary Lung Cancer
Takanori Ayabe*, Masaki Tomita, Eiichi Chosa, Katsuya Kawagoe, Kunihide Nakamura
Department of Surgery II, Faculty of Medicine, University of Miyazaki, Miyazaki, Japan
Email: *tayabe@med.miyazaki-u.ac.jp
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 15 June 2014; revised 12 July 2014; accepted 8 August 2014
ABSTRACT
Background: The purpose of this study was to evaluate the effectiveness of perioperative tiotropium therapy for patients undergoing pulmonary resection for primary lung cancer. The shortterm tiotropium effect was investigated by perioperative pulmonary function and “lung age”. Methods: The fifty-five patients who underwent a lobectomy and had tiotropium treatment available from October 2007 through May 2009 were the subjects. The patients were divided into 3 groups according to their airway limitation such as Chronic Obstructive Pulmonary Disease (COPD) or a history of smoking; those with COPD (%FEV1 ≤ 70%, C-group, n = 22), smokers (%FEV1 > 70%, S-group, n = 10) and non-smokers (%FEV1 > 70%, N-group, n = 23). As the bronchodilator groups, the Cand S-groups received inhaled tiotropium bromide (18 μg once daily) for 1 week before surgery until at least 3 weeks after surgery without interruption, and as a control, the N-group had no treatment. The preoperative baselines, the predicted postoperative values, and the actual postoperative ones were measured by the pulmonary function test. The changed rates were calculated and denoted as ΔVC, ΔFEV1, ΔVC%, and ΔFEV1/FVC, from the baseline of the predicted postoperative values. The mean “real age” and “lung age” were calculated. Results: In the S-group, the parameters of ΔVC, ΔFEV1, ΔVC%, and ΔFEV1/FVC significantly increased compared to those of the N-group. In the C-group, the increased extents of ΔFEV1 and ΔFEV1/FVC were lower compared to those in the S-group (not significant). In the N-group, the parameters of ΔVC, ΔFEV1, and ΔVC% decreased. The postoperative “lung age” and “real age” were increased to 29.5 ± 18.0 year-old in the C-group, 25.8 ± 18.0 in the S-group, and 24.7 ± 17.0 in the N-group. Lung resection affected the “lung age”; the aging was a 28.9 ± 12.7 year-old increase in the N-group. In the Cand S-group, the “lung age” was a 14-year-old increase. The effect of tiotropium treatment affected the “lung age” as a 15-year-old increase. Conclusion: Perioperative interventional tiotropium contributed to the lobectomy patients with COPD and for smokers with a non-obstructive airway and played a role of preserving the postoperative lung function.
Keywords: Tiotropium, Pulmonary Function, Lung Age, Lobectomy, Lung Cancer

1. Introduction
The main focus of therapy for Chronic Obstructive Pulmonary Disease (COPD) is to relieve the symptoms, prevent disease progression, improve exercise tolerance and health status, prevent exacerbations and improve survival, preferably by interventions with a favorable safety profile [1] . The initial therapy involves preventive measures and often the use of a short-acting bronchodilator as needed. However, given the known progression of COPD, patients who become symptomatic will eventually require maintenance medication. The present guidelines provide several options for first-line maintenance pharmacotherapy, yet sparse data exist regarding the outcome that can be expected upon first prescription of the initial medication [1] .
Studies of patients who are not yet on maintenance respiratory therapy are needed to assist healthcare professionals in decision-making regarding their choice of the initial treatment. The Understanding Potential Longterm Impacts on Function with Tiotropium (UPLIFT®) trial [2] -[4] offers a unique opportunity to gain insight into using tiotropium as a first maintenance drug in COPD. In the 4-yr UPLIFT® trial, patients were randomized into a group receiving 18 μg tiotropium once daily or a placebo. The main results of the effect of tiotropium on the lung function, health-related quality of life, exacerbation rate and mortality are presented elsewhere [3] [4] .
On the pharmacology of tiotropium, there are 3 muscarinic receptors found in human airways. M1 receptors facilitate cholinergic neurotransmission and enhance cholinergic bronchoconstriction. M3 receptors mediate the bronchoconstriction and mucus secretion. M2 receptors serve as a feedback mechanism and inhibit the release of acetylcholine. Blocking the M1 and M3 receptors in the airways results in bronchodilation and decreased mucus secretion. When the M2 receptor is blocked, acetylcholine release is enhanced thereby potentially offsetting the bronchodilation achieved via inhibition of the M1 and M3 receptors. Tiotropium is a muscarinic antagonist and has a similar binding affinity for the M1, M2, and M3 receptors; however, it dissociates more slowly from the M1 and M3 receptors.
Lung cancer patients often have COPD, because both conditions are strongly associated with cigarette smoking. A high prevalence of COPD has been reported in patients with a new diagnosis of lung cancer [5] [6] . COPD is often underdiagnosed and undertreated [7] , so a new diagnosis of COPD is often made during the evaluation of patients requiring lung resection. Although pulmonary resection remains the only potentially curative treatment for lung cancer, lung cancer patients with COPD and/or smoking are at high risk for pulmonary resection [8] [9] . The perioperative management of COPD and smoking is therefore an important issue during the preparation for pulmonary resection. However, no prophylactic strategy has been established.
Lung cancer remains a significant cause of death for smokers, and smoking is often associated with COPD. A surgical resection offers the best chance for curing lung cancer. However, lung cancer patients with COPD are frequently deemed inoperable due to low pulmonary function, and such patients often suffer from pulmonary complications after surgery [10] . COPD and smoking in lung cancer patients are two of the causes leading to postoperative morbidity and mortality.
Recently, the Global Initiative for Obstructive Lung Disease (GOLD) guidelines and the American Thoracic Society (ATS)/European Respiratory Society (ERS) position paper [11] emphasized the role of long-acting bronchodilators, such as tiotropium and salmeterol, and recommended these as the first-line treatment for patients with COPD. To date, there have been no studies that evaluated the influence of these drugs on postoperative cancer patients with COPD. Suzuki H et al. [12] conducted a prospective randomized trial study and reported the efficacy of tiotropium and salmeterol on the postoperative pulmonary function and quality of life in lung cancer patients with COPD. The function of the remaining lungs after major lung resection may be a determination of the early postoperative outcomes, as well as the late postoperative quality of life of the patients.
The aim of the present study was to investigate the efficacy of bronchodilator therapy (perioperative tiotropium treatment) for the surgical patients, who underwent a lobectomy for lung cancer with COPD and with decreased pulmonary function by the influence of smoking. We divided the surgical patients into 3 groups, which are, the COPD, smoker, and non-smoker with healthy lungs. We conducted this study to investigate whether preoperative tiotropium intervention can preserve the postoperative pulmonary function of the surgical patients who underwent a lobectomy for lung cancer and improve the postoperative lung age.
2. Patients and Methods
2.1. Patients
Between October 2007 and May 2009, a total of 55 patients with primary Non-Small Cell Lung Cancer (NSCLC) underwent surgical resection at the University of Miyazaki Hospital. Preoperatively, the patients were enrolled to perform a lobectomy and lymph nodes dissection of resectable NSCLC. Figure 1 shows the concept of this study. After the diagnosis of lung cancer, the airway obstruction of these patients was preoperatively defined as the percentage of forced expiratory volume in 1 second (%FEV1). The extent of the airflow limitation was assessed by spirometry and was defined as a prebronchodilator percentage of %FEV1. Of them, 22 patients as an obstructive group with a preoperative %FEV1 of less than or equal to 70% (%FEV1 ≤ 70%), that is called the COPD group (C-group, n = 22), and the other 33 patients as the non-obstructive group with a preoperative %FEV1 more than 70% (%FEV1 > 70%) were divided in two groups. For the non-obstructive group (n = 33), the patients were also evaluated in two groups as a smoker group with the history of smoking more than 20 pack-year and/or temporally stopping the smoking before surgery (S-group, n = 10) and a non-smoker group without any smoking history (N-group, n = 23). After forming these three groups, a preoperative intervention of tiotropium was performed for the COPD group (n = 22) and the smoker group (n = 10), on the other hand, as the control, no preoperative intervention of tiotropium was done for the non-smoker group (n = 23).
Furthermore, for patients with a prebronchodilator forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) ≤ 0.70, the patients in each group were divided into two COPD grades: GOLD-I COPD (mild, FEV1 ≥ 80%, predicted) and GOLD-II COPD (moderate, 50% ≤ FEV1 < 80%). The severity of COPD was classified using the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria [13] . Spirometry was performed by a trained technician.
All patients with preoperative smoking had stopped smoking cigarettes for more than 1 month before surgery, even if they were current smokers. Patients diagnosed with respiratory disorders other than COPD, such as asthma, were excluded. The exclusion criteria for the present analysis were a history of treatment for COPD. The patient selection was at the discretion of the attending physicians. The tiotropium treatment in this study was performed in daily clinical practice and approved by the attending physicians in our department but not by the institutional ethics committees. All patients provided informed consent before the treatment.
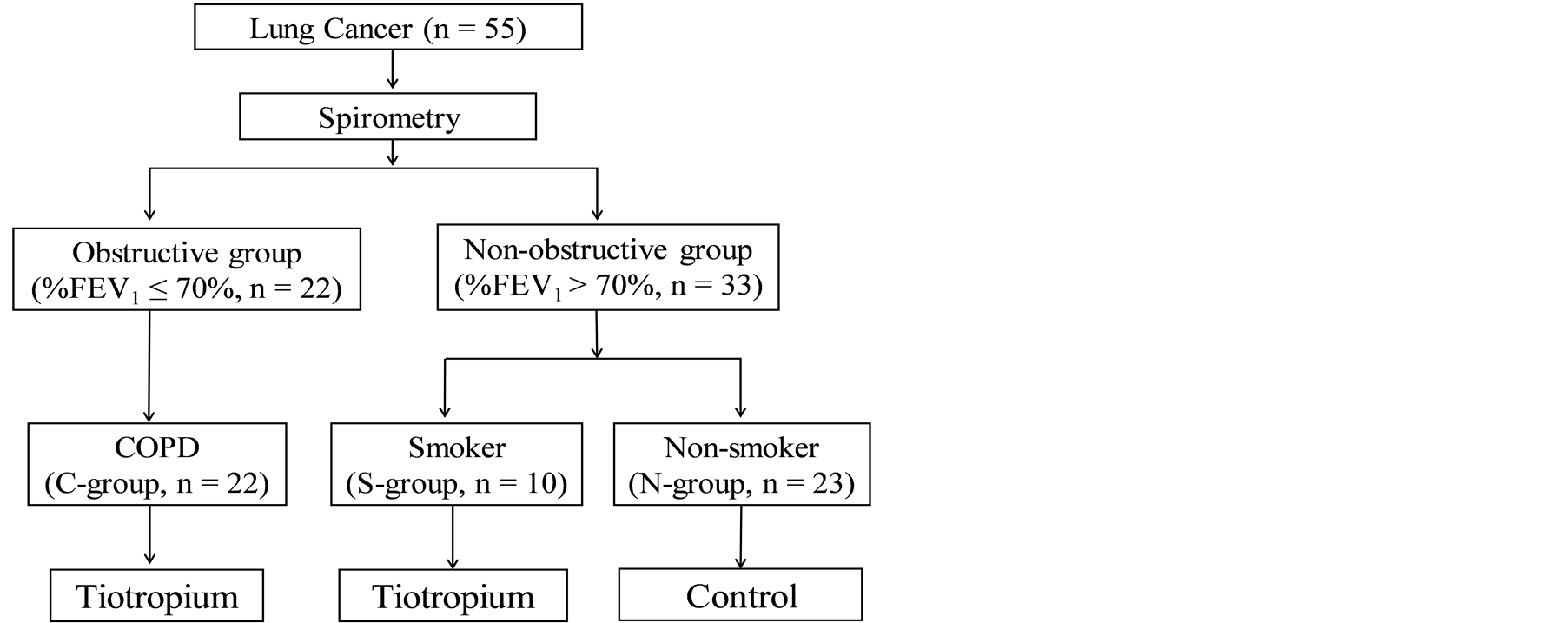
Figure 1. The concept of this study.
2.2. Treatment Design
Figure 2 shows the treatment design and schedule of this study. To examine the efficacy of bronchodilator therapy (preoperative interventional tiotropium treatment) for patients, we divided the patients who underwent a lobectomy for lung cancer in three groups. We evaluated the changed degree of the postoperatively-decreasing pulmonary function of the COPD, smoking, and the non-smoker healthy patients.
As an interventional bronchodilator treatment, two groups (the COPD and the Smoker groups, n = 32) received inhaled tiotropium bromide (18 μg once daily) (Spiriva®, Handi Haler; Boehringer Ingelheim, Berkshire, UK) for 1 week before surgery until at least 3 weeks after surgery without interruption in the current study.
The preoperative baseline data of the patients were evaluated using a pulmonary function test on a preoperative day of more than 1 week before surgery. The postoperative parameters of the pulmonary function test were measured as the actual postoperative value on postoperative day 3 weeks after surgery. All respiratory medications, with the exception of other inhaled anticholinergics, were permitted throughout the trial.
2.3. Surgery
All of the patients in this study had been diagnosed with preoperatively-resectable NSCLC and underwent lobectomy surgery. Surgery was performed under general and epidural anesthesia with a double-lumen endobronchial tube. After establishing a single-lung ventilation, the patient was flexed in the lateral decubitus position. After a posterolateral skin incision, a thoracotomy was performed through the fifth intercostals space using the dorsalpedis muscle-sparing technique. During anatomic resection, we used an endoscopic stapler (Ethicon, Tokyo, Japan, Covidien, Tokyo, Japan) to divide the lung parenchyma and incomplete fissures, and excise the bronchi. The pulmonary arteries and veins were also divided with an endoscopic stapler if the diameter of the vessels was greater than 5 mm. After anatomic resection and a mediastinal lymphadenectomy, we performed a water-seal test to ensure pneumostasis. Suture-lines were not buttressed, but evident pulmonary fistulae were closed with sutures and sealed with fibrin glue. A 24-F chest tube was placed in the hemithorax, and the wounds were closed. Patients were allowed to drink water 6 hours after extubation, and to eat and walk with assistance by the next morning after surgery. Patients continued to use inhaled tiotropium throughout the preoperative and postoperative periods. All patients received preoperative epidural anesthesia for pain management, which usually remained in place for 3 - 7 days and they were started on oral analgesia from the first postoperative day, and the chest drainage tubes were removed within the discharge volume of 200 ml per day. Postoperative spirometry was performed 3 weeks after surgery.
2.4. Pulmonary Function Testing
The pulmonary function test was performed using a hospital spirometer, in which the Vital Capacity (VC), the predicted percentage of VC (VC%, % predicted), the Forced Vital Capacity (FVC), the forced expiratory volume in one second (FEV1), the percentage of FEV1 (%FEV1), the percentage ratio of the forced expiratory volume in one second (FEV1)/the forced vital capacity (FVC) (FEV1%, FEV1/FVC × 100) were measured on the preoperative day before the administration of the first dose of tiotropium before surgery.
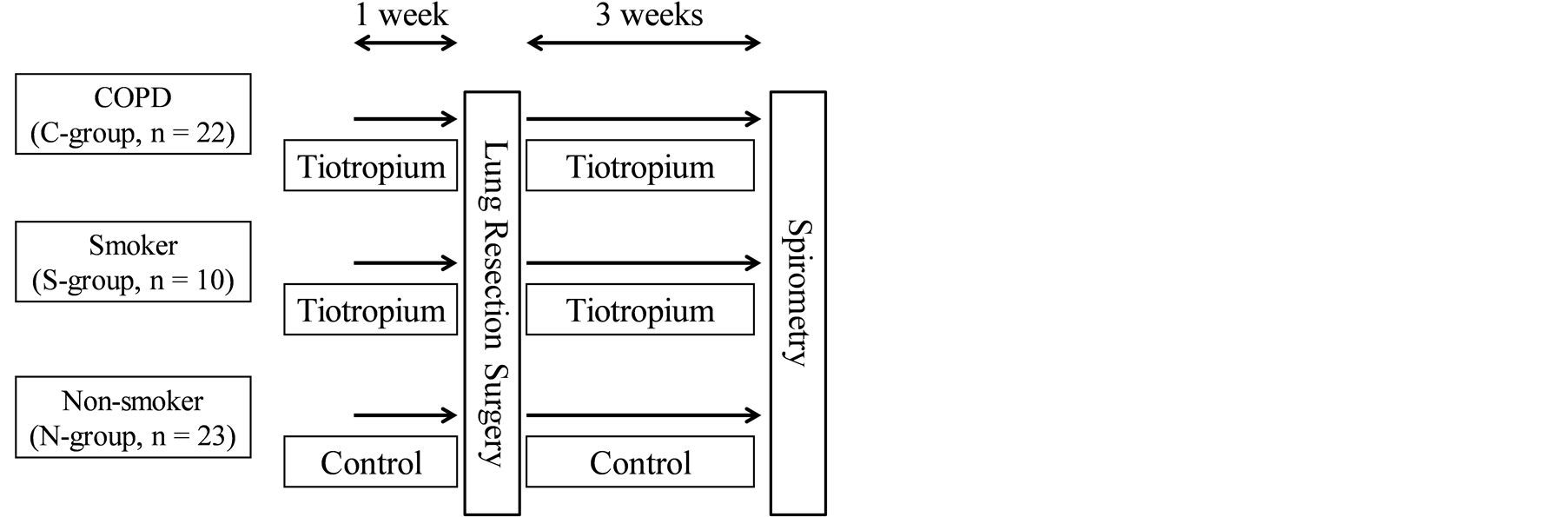
Figure 2. The treatment design and schedule of this study.
The values of the obtained pulmonary function tests were defined as the preoperative baseline values (base-VC, base-FEV1, base-VC%, and base-FEV1/FVC). For the predicted postoperative values (ppo-values) of VC, FEV1, VC%, and FEV1/FVC, for example, in the case of FEV1, we estimated the predicted postoperative FEV1 (ppo-FEV1) using the following equation: ppo-FEV1 = preoperative FEV1 × (1 − S × 0.0526), where S = number of resected bronchopulmonary segments [14] . For the actual postoperative values 3 weeks day after surgery, the pulmonary function test was performed and defined as the actual postoperative values (apo-VC, apo-FEV1, apo-VC%, and apo-FEV1/FVC).
To compare the difference between the preoperative and the postoperative lung functions, the percentage (%) changed from the baseline of the predicted postoperative values (VC, %VC, FEV1, and FEV1%) was calculated. After the predicted postoperative values (ppo-values) and the actual postoperative values (apo-values) were obtained, we determined the changed rates between the ppo-values and the apo-values as the ΔVC, ΔFEV1, ΔVC, and ΔFEV1/FVC (%). For example, in case of the calculated ΔFEV1 (%), the following equation was used. ΔFEV1 (%) = 100 × [(The apo-FEV1) − (The ppo-FEV1)]/(The ppo-FEV1).
2.5. The Concept of “Lung Age”
The Japanese Respiratory Society (JRS) defined the standard regression equation of FEV1 for Japanese people in 2001, as follows:
Male: FEV1 (L) = 0.036 × body height (cm) − 0.028 × real age (years) − 1.178 Female: FEV1 (L) = 0.022 × body height (cm) − 0.022 × real age (years) − 0.005 These calculations lead to the standard predicted values of FEV1 based on the body height and real age of Japanese people. In 2007, the JRS proposed the conception of “lung age”. The calculated “lung age” is derived from the inverse calculation of the standard regression equation of FEV1, as noted above. The following are the expressions.
Male: Lung age (years) = (0.036 × body height (cm) − 1.178 − FEV1 (L))/0.028 Female: Lung age (years) = (0.022 × body height (cm) − 1.005 − FEV1 (L))/0.022
2.6. The Calculation of “Lung Age”
Based on the results of the measured value from the preoperative pulmonary function test, we derived a preoperative “lung age” in accordance with the calculation described above. The mean “real age” and preoperative “lung age” of all patients in the three groups were calculated. In addition, we calculated the postoperative “lung age” after the lobectomy surgery using the actual postoperative values of the pulmonary function test. We determined a difference in the postoperative “lung age” and preoperative “lung age”, and the postoperative “lung age” and “real age” in each group.
2.7. Statistical Analysis
Means and standard deviations are used for the description of the continuous measures. The differences in the preoperative and postoperative values from the pulmonary function test and the difference in the changed ratio of the predicted and actual postoperative values after surgery were tested by Student’s paired t-test among each group. A p-value less than 0.05 was considered to be statistically significant.
3. Results
3.1. Patient Characteristics
The characteristics of the 55 patients involved in this study are summarized in Table1 All patients had an Eastern Cooperative Oncology Group performance status of 1. There were no patients who received new medication without tiotropium during the study period. None of the subjects had the inhaled tiotropium discontinued due to any side effects, and none had any cardiopulmonary events and postoperative complications during the study protocol. There was no death within 30 days following surgery.
The average age of the C-group (74.2 ± 4.9) was significantly higher than the N-group (64.4 ± 7.9, p = 0.0062) and the S-group (68.8 ± 6.3, p = 0.0174), however, it was not significantly higher than the N-group (68.8 ± 6.3, p = 0.0673). There were more men in the C-group (68.2%, 15/22), however, more women in the N-group (26.1%
GOLD: Global Initiative for Chronic Obstructive Lung Disease.
6/23). Regarding preoperative smoking, there were 16 smokers (6 patients in the C-group and 10 patients in the S-group) and 39 non-smokers (16 patients in the C-group and 23 patients in the N-group).
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) severity stage, stage 0 was 21; stage I was 21; stage II was 13 cases.
In the C-group, 13 patients were stage II (59.1%, 13/22). In the S-group, 4 patients (40%, 4/10) were stage I, while 8 patients (34.8%, 8/23) were stage I in the N-group. Histology showed 42 adenocarcinoma, 12 squamous cell carcinoma, and 1 large cell carcinoma. The operation procedures involved 53 lobectomies and 2 bilobectomies. The operation side was 33 right lobectomies (13 upper lobes, 1 upper-middle one, 3 middle ones, 1 middle-lower one, and 15 lower ones) and 22 left lobectomies (14 upper lobes and 8 lower ones). The postoperative pathological examination was defined as stage IA, 32; IB, 9; IIB, 4; IIIA, 8; IIIB, 1; IV, 1. Although 1 patient was diagnosed with preoperatively c-staged IA (cT1N0M0), this patient was postoperatively diagnosed with p-T4N2M0 due to an intraoperatively-suspected dissemination. One patient was postoperatively-diagnosed with p-staged IIIB from preoperatively c-staged IA (cT1N0M0). After one patient had been clinically diagnosed with a brain tumor and had undergone neurosurgery, however, the brain tumor had been finally diagnosed with brain metastasis from lung cancer, even though p-staged IV NSCLC, a lobectomy for primary NSCLC was performed.
3.2. Changes of Pulmonary Function
As shown in Tables 2-5, the variables (VC, FEV1, VC%, and FEV1/FVC) at the preoperative baseline, postoperative predicted one, actual postoperative one, and the changed rates between the postoperative and preoperative values are listed for the three groups (C-, S-, and N-group). The comparison between two groups from the three (between Cand S-group, between Cand N-group, and between Sand N-groups) was performed using the paired t test.
Table 2. The variables for the preoperative baselines.
Table 4. The variables for the actual postoperative values.
Table 5. The variables for the changed rates between the postoperative and preoperative values.
In Table 2, before the preoperative intervention of tiotropium, on the baseline values (base-values), the mean VC values were not significantly different between each of the two groups. On the other hand, the mean FEV1 value (1.86 ± 0.46 L) in the C-group was significantly lower than 2.22 ± 0.46 L in the S-group (p = 0.0133), and was significantly lower than 2.31 ± 0.61 L in the N-group (p = 0.0254). For the non-obstructive group, that is, between the S-group and the N-group, there was no significant difference in the mean baseline FEV1 values (p = 0.3399). Before the preoperative intervention of tiotropium, on the baseline FEV1/FVC values in Table 2, the mean base-FEV1/FVC value (60.4% ± 7.4%) in the C-group was significantly lower than 80.4% ± 1.9% in the S-group (p < 0.0001) and 76.6% ± 4.5% in the N-group (p < 0.0001). For the non-obstructive group, that is, between the S-group and the N-group, there was no significant difference in the mean base-FEV1/FVC value (p = 0.3565).
In Table 4, for the actual postoperative values (apo-values) with the intervention of tiotropium, the mean apo-VC, apo-VC%, and FEV1 values were not significantly different between each of the two groups, while the mean apo-FEV1/FVC values were significantly different between each of the two groups. For comparison of the baseline values before the preoperative intervention of tiotropium in Table 2 and the actual postoperative values with the intervention of tiotropium in Table 4, the C-group decreased postoperatively from 3.13 ± 0.59 L preoperatively to 2.26 ± 0.50 L, even with the intervention of tiotropium. However, in the S-group, the mean VC value did not decrease postoperatively from 3.01 ± 0.50 L preoperatively to 2.91 ± 0.40 L by the tiotropium intervention. On the other hand, in the N-group without intervention of the tiotropium, the mean VC value decreased postoperatively from 3.01 ± 0.71 L preoperatively to 2.12 ± 0.55 L. On the other hand, on the apo-FEV1/FVC value, the C-group increased postoperatively from 60.4% ± 7.4% preoperatively to 67.7% ± 9.2%, by the effect of intervention of tiotropium. However, in the S-group, the mean apo-FEV1/FVC value did not increase but decrease postoperatively from 80.4% ± 1.9% preoperatively to 75.8% ± 7.1%, even with tiotropium intervention. In addition, in the N-group without the intervention of tiotropium, the mean apo-FEV1/FVC value slightly increased postoperatively from 76.6% ± 4.5% preoperatively to 77.7% ± 5.2%.
In Table 5, the changes, such as, the increase and decrease as a difference between the mean apo-values and the mean ppo-values were defined as the changed rates (Δ), that is, ΔVC, ΔFEV1, ΔVC%, and ΔFEV1/FVC. For the mean parameters of ΔVC, ΔFEV1, ΔVC%, and ΔFEV1/FVC values, there were significant differences between the S-group and the N-group, that is, these values in the S-group positively increased, on the other hand, the ones in the N-group were significantly decreased in the negative direction.
For the mean parameter of ΔVC, there were decreases in the C-group (−6.0% ± 15.0%) and in the N-group (−11.0% ± 12.0%), however, an increase in the S-group (21.9% ± 4.2%). In the non-obstructive group, there was a significant increase in ΔVC due to the tiotropium treatment for the S-group compared to a decrease in the non-tiotropium treatment for the N-group (p = 0.0102). Tiotropium intervention affected the increase in ΔVC of the non-obstructive smoking group, however, it did not affect the increase but the decrease in ΔVC of the obstructive COPD group.
For the mean parameter of ΔFEV1, there was an increase in the C-group (5.0% ± 19.0%) and in the S-group (16.8% ± 4.0%), however, a decrease in the N-group (−10.0% ± 14.0%). In the tiotropium treated group (Cand S-group), there was an increase in ΔFEV1, on the other hand, in with treatment of tiotropium for the N-group, there was a decrease in ΔFEV1. In the non-obstructive group, there was a significant increase due to the tiotropium treatment compared to a decrease in ΔFEV1 due to the non-tiotropium treatment for the N-group (p = 0.0004). Tiotropium intervention affected the increase in FEV1 of both the obstructive COPD group and non-obstructive smoking group, however, the extent of the increase in the N-group was higher than in the C-group.
For the mean parameter of ΔVC%, there was a decrease in the C-group (−5.0% ± 14.0%) and in the N-group (−11.0% ± 12.0%), however, an increase in the S-group (77.5% ± 18.1%). In the tiotropium treatment group, there was a decrease in ΔVC% in the C-group, on the other hand, in the N-group, there was an increase in ΔVC%. For ΔVC% in the non-obstructive group, there was a significant increase in the S-group due to the tiotropium treatment compared to a decrease in the non-tiotropium treatment for the N-group (p = 0.0101). Tiotropium intervention affected the increase in ΔVC% of the non-obstructive smoking group, however, the extent of the decrease in the N-group was lower than in the C-group.
For the mean parameter of ΔFEV1/FVC, there were increases in the three groups; i.e., in the C-group (45.0% ± 16.0%), in the S-group (56.8% ± 8.4%), and in the N-group (29.0% ± 12.0%). In the tiotropium treated group (Cand S-group), there was an increase in ΔFEV1/FVC, and also for the no treatment of tiotropium in the N-group, there was an increase in ΔFEV1/FVC. In the non-obstructive group, there was a significant increase due to the tiotropium treatment compared to an increase in ΔFEV1/FVC for the non-tiotropium treatment for the N-group (p = 0.0004). Tiotropium intervention affected the increase in ΔFEV1/FVC of both the obstructive COPD group and non-obstructive smoking group, however, the extent of the increase in the N-group was lower than those in the C-group due to the no treatment of tiotropium.
Based on the results of the changed rates by the intervention of tiotropium for the non-obstructive group in the S-group, the parameters of ΔVC, ΔFEV1, ΔVC%, and ΔFEV1/FVC were positively increased, which were significantly improved compared to those of the N-group. In the C-group, the parameters of ΔFEV1 and ΔFEV1/FVC positively increased, however, the extents of the increase were small compared to those in the S-group, and the parameters of ΔFEV1 and ΔFEV1/FVC in the C-group were not significantly improved compared to those of the N-group. For the no intervention of tiotropium to the non-obstructive group, in the N-group, the parameters of ΔVC, ΔFEV1 and ΔVC% were decreased. The increased extent of ΔVC, ΔFEV1, ΔVC%, and ΔFEV1/FVC values in the C-group were smaller compared to those in the S-group, and there was no significant difference between the Cand S-groups. Comparison of the parameters of ΔVC, ΔFEV1, ΔVC%, and ΔFEV1/FVC in the C-group of the obstructive group and of those in the S-group in non-obstructive group, the changed rates of them in the S-group had more significantly increased than those in the C-group (not significant).
3.3. Real Age, Preoperative “Lung Age”, and Postoperative “Lung Age”
As shown in Table 6, the real age was 74.2 ± 4.9 years in the C-group, 68.8 ± 6.3 years in the S-group, and 64.4 ± 7.9 years in the N-group. The real age in the C-group was the highest, and that in the N-group was the youngest of the three groups. Based on calculation of the preoperative “lung age” based on the lung age concept described in method, the preoperative “lung age” was 89.2 ± 17.9 years in the C-group, 84.0 ± 19.0 years in the S-group, and 60.2 ± 20.8 years in the N-group. Considering the pulmonary aging effect, the influence of COPD and smoking on the “lung age” was estimated to be 15.0-years in the C-group, 15.2-years in the S-group, however, in the case of the N-group, due to no COPD and no exposed smoking, the preoperative “lung age” was estimated to be
4.2-year-old younger compared to the “real age”. COPD and smoking affected the pulmonary function, and the effect was an aging of 15-years to the “lung age”.
After the lobectomy, the postoperative “lung age” was 103.7 ± 17.4 years in the C-group, 98.4 ± 18.2 years in the S-group, and 89.1 ± 16.8 years in the N-group. The difference in the postoperative “lung age” and preoperative “lung age” was 14.5 ± 13.1 years in the C-group, 14.4 ± 12.2 years in the S-group, and 28.9 ± 12.7 years in the N-group. Invasive surgical influence, that is, the open lobectomy affect on the pulmonary function, the effect was adding of aging of 29-years to the “lung age” in the N-group without tiotropium intervention. On the other hand, as the effect on the Cand S-groups was adding of aging of 14-years to the “lung age”; the effect of intervention of tiotropium decreased about 15-years the degree to the “lung age”.
The difference in the postoperative “lung age” and “real age” was 29.5 ± 18.0 years in the C-group, 25.8 ± 18.0 years in the S-group, and 24.7 ± 17.0 years in the N-group. Surgical invasive influence, open lobectomy to COPD, smoking, and non-smoking patients, added aging of 24- to 29-years to the “lung age”.
4. Discussion
Lung cancer is the leading cause of cancer death in Japan and around the world. The number of lung cancer patients with a poor respiratory function has been increasing due to long-term smoking, an aging population and environmental factors. COPD is a disorder of decreased respiratory function. According to a Nippon COPD Epidemiology study, COPD was prevalent in males (16.4%) and females (5%) aged ≥40 years in Japan [15] . COPD was complicated in 10% of the lung cancer patients (48/521 Pts.) [16] . In patients with a new diagnosis of lung cancer, the prevalence of COPD varied between 40% and 70% [5] [17] . Patients with lung cancer have a six-fold greater risk of having COPD than matched smokers [6] . COPD is largely underdiagnosed and undertreated [7] [18] . The frequent coexistence of COPD increases the risk of operation because of an impaired postoperative ventilatory function [8] . In the study of potential patient-related risk factors with postoperative pulmonary complications in COPD that provided an adjusted estimate of risk, the odds ratio was 1.79 (CI, 1.44 to 2.22) [19] . Furthermore, COPD is an important patient-related risk factor for postoperative pulmonary complications [20] . Up to 50% of patients with COPD develop postoperative COPD exacerbations after lung resection [21] . General guidelines for the perioperative pulmonary management exist and focus on smoking cessation, pulmonary toilet, and physical therapy [22] . There are few data on the short-term effects of pharmacologic treatment in patients with newly diagnosed COPD requiring surgery for lung cancer. In a study of 20 patients with lung cancer and untreated COPD, preoperative treatment with tiotropium for at least 7 days improved the lung function prior to thoracic surgery; however, no effect was seen regarding postoperative complications [23] .
Recently, the addition of inhaled corticosteroids for the treatment of patients with moderate-to-severe COPD leads to significant improvements in their lung function. Furthermore, inhaled corticosteroids reduced the risk of COPD exacerbations in these patients [24] . Bölükbas S et al. [25] hypothesized that the addition of an inhaled corticosteroid to preoperative treatment with long-acting bronchodilators could optimize the preoperative lung function and reduce the risk for postoperative pulmonary complications. They reported the benefit from adding inhalative budenoside to tiotropium and formoterol in terms of an improvement in FEV1 and the severity of COPD, which beneficial results might lead to less pulmonary complications in the postoperative period.
Tiotropium is a once-daily, inhaled anticholinergic that provides at least 24 hours of improvement in airflow and hyperinflation in patients with COPD [3] . The results of the UPLIFT (Understanding Potential Long-Term Impacts on Function with Tiotropium) trial, which tested whether tiotropium could reduce the rate of decline in FEV1 in patients with COPD who were permitted treatment including use of shortand long-acting respiratory medication other than inhaled anticholinergics, have been published [3] . Although there was no difference in the rate of FEV1 decline over the placebo, at all time points, patients receiving tiotropium had significant improvements in their lung function and health-related quality of life and had a reduced risk for exacerbations, episodes of respiratory failure, and hospitalizations due to COPD exacerbations compared with patients receiving a placebo.
COPD is characterized by airflow limitation which is not fully reversible [1] . There has been much interest in whether acute bronchodilator responsiveness based on a predefined threshold of a change in forced expiratory volume in the first second (FEV1) is a prognostic factors in COPD [26] [27] . A 1-yr trial with tiotropium showed that acute responsiveness was not predictive of whether patients clinically improved [28] . However, whether such a responsiveness can predict disease progression or health outcomes beyond 1 year has not been established. Further, more the reliability of the currently recommended criteria for assessing responsiveness (also referred to as reversibility) differs according to various guidelines. The American Thoracic Society considers a 200 ml and 12% increase from the pre-bronchodilator baseline FEV1 as a positive bronchodilator responsiveness [29] , while a 15% increase from the baseline [30] or 10% increase in normalized FEV1 is considered a positive bronchodilator responsiveness by the other group [26] [31] [32] .
The function of the remaining lungs after major lung resection may be a determination of the early postoperative outcome, as well as the late postoperative quality of life of the patients [33] . Therefore, an assessment of the pulmonary ventilator capacity is mandatory in patients undergoing major lung resection [34] . Because the adult lung generally does not have the ability to generate new alveolar septal tissue [35] , the postoperative pulmonary function can be theoretically determined by the amount of parenchymal resection. However, the postoperative pulmonary function can also be influenced by various other factors, such as the site of resection (upper lobectomy or lower lobectomy), the severity of pulmonary emphysema, and the surgical approach (open or port access). The ventilatory capacity is impaired during the early postoperative period in accordance with the level of chest wall trauma (posterolateral thoracotomy > anterior thoracotomy > video-assisted thoracic surgery) due to the reduction in the chest wall motility [36] . Many reports suggest that the pulmonary ventilation capacity is better preserved after a lobectomy via video-assisted thoracic surgery than after posterolateral thoracotomy within 3 months after the operation [36] . However, the differences may decrease or disappear 1 year after a lobectomy [37] .
It has been well recognized that the postoperative pulmonary function can be unexpectedly improved after a lobectomy due to a volume reduction effect in patients with moderate to severe pulmonary emphysema [33] . Relief of the airflow obstruction, improved respiratory muscle function, elimination of dead space ventilation in ventilated but unperfused areas, and improved cardiovascular hemodynamics may all contribute to this unexpected improvement [38] -[40] . Many reports emphasize that the remaining lung function is higher than the predicted values in patients with COPD [16] [41] [42] . However, the extent of the differences between the predicted and measured postoperative pulmonary function significantly differs in individual patients with COPD.
The function of the remaining lung after lobectomy time-dependently improves during the first postoperative year. Zeiher et al. [43] reported that the late postoperative forced expiratory volume in 1 s (FEV1) was 250 ml higher than the values predicted by the standard segment counting techniques.
Based on the percent change in the value after a lobectomy [44] -[48] , although the lobectomy corresponded to resection of, on average, 20% of the total lung parenchyma. Regardless of the significant reduction in the FEV1, the diffusing capacity of the lung for carbon monoxide (DLCO) and the maximum oxygen consumption (VO2max) did not decrease or only slightly decreased after the lobectomy [33] . Regardless of some conflicting reports [47] [49] , the assessment of the postoperative pulmonary function by the FEV1 can likely lead to an overestimation of the loss of the postoperative pulmonary function. To evaluate the functional respectability for lung cancer, the preoperative pulmonary function test is still the gold standard, and ppoFEV1 is the most reliable predictor for mortality and morbidity [20] [50] . However, several approaches, such as inhalation perfusion (single-photon emission computed tomography) imaging [51] , perfusion lung scintigraphy [52] , and quantitative computed tomography [53] have been proposed for predicting precise postoperative FEV1. None of these methods has been proven to be more accurate than the simple calculation based on the number of removed bronchopulmonary segments [16] . However, recent studies have shown that underestimation of the actual postoperative FEV1 may occur due to heterogeneous distribution of the ventilation and perfusion [54] .
Regarding the “lung age”, the Japanese Respiratory Society (JRS) recently proposed that the concept of “lung age” be easily understood by both clinicians and patients. Pulmonary function testing is essential for the diagnosis of the “lung age”. Additionally, pulmonary function testing is routinely preoperatively performed on lung cancer patients to assess surgical risk and to predict and prevent postoperative complications. However, the interpretation of the results of pulmonary function testing is sometimes difficult for both patients and clinicians. “Lung age” could be useful for the prediction of post-operative respiratory complications and survival in patients with surgically treated lung cancer [55] . This study investigated a change in the “lung age” before and after surgery. The study evaluated whether “lung age”, a simple indicator of pulmonary obstructive impairment as typified by COPD, could be a useful parameter for lung cancer patients with pulmonary resection [55] . There has been extensive research on pulmonary resection for lung cancer patients with a poor respiratory function, although no study has evaluated patient outcome using a simple parameter obtained from the pulmonary function test [55] . “Lung age” could be just a parameter to use in daily clinical practice. Assessment of the difference between “real age” and “lung age” is useful and convenient for predicting complications and prognosis. “Lung age” should be used widely for lung cancer patients because it helps patients to understand their own respiratory function, especially obstruction impairment. In this study, the “lung age” was preoperatively calculated in the COPD and the Smoker group, compared to the “real age”, and there was an increase in aging of a 14-year degree to the “lung age” before surgery. The difference in the “postoperative lung age” and “real age” was 29.5 ± 18.0 in the C-group, 25.8 ± 18.0 in the S-group, and 24.7 ± 17.0 in the N-group. Open thoracotomy is an invasive surgery, which influences to the postoperative pulmonary function. For COPD, smoking and non-smoking patients, the influenced degrees was an increase in aging from 24- to 29-years to the “lung age”. The effect of tiotropium treatment was preserving of the 15-years to the “lung age”.
Regarding the limitations of this study, this is a small number of patients in a single university hospital. A larger prospective and double-blind randomized study will be needed. In the current study, there was a lack of a completely placebo group for the tiotropium treatment for the COPD group. That is, there was no set up with patients of no triotropium treatment in the COPD group. Therefore, it remains unclear whether the perioperative tiotropium intervention was effective or not for the COPD surgical patients. In addition, whether or not it possible to expand the indication of COPD patients, it should be evaluated whether or not preoperative tiotropium intervention would reduce the postoperative complication.
5. Conclusion
A preoperative tiotropium intervention for surgical patients, such as either COPD or smoker with %FEV1 > 70%, would inhibit the extent of postoperatively-decreasing pulmonary function, and would improve the postoperative pulmonary function. The mechanism of the postoperatively preserved FEV1, but not the decreased FEV1 should be based on the benefit of the lung volume reduction surgery, the efficacy of tiotropium as a bronchodilator, and the cessation of smoking. Tiotropium treatment affected the increase of FEV1 and FEV1/FVC compared to the non-treated group with the non-obstructive group. Therapy with tiotropium for smoking patients with a normal lung function resulted in a much better efficacy compared to that for COPD ones with a worse pulmonary function. Preoperative intervention with tiotropium for the lobectomy cases of lung cancer patients with COPD and smoking, which suggested a benefit of improving the postoperatively decreased pulmonary function. However, further study would be needed if the above benefit should contribute to improving the surgical outcome and extend the surgical indication.
References
- Rabe, K.F., Hurd, S., Anzueto, A., Barnes, P.J., Buist, S.A., Calverley, P., Fukuchi, Y., Jenkins, C., Rodriguez-Roisin, R., Van Weel, C. and Zielinski J. (2007) Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: GOLD Executive Summary. American Journal of Respiratory and Critical Care Medicine, 176, 532-555. http://dx.doi.org/10.1164/rccm.200703-456SO
- Decramer, M., Celli, B., Tashkin, D.P., Pauwels, R.A., Burkhart, D., Cassino, C. and Kesten, S. (2004) Clinical Trial Design Considerations in Assessing Long-Term Functional Impacts of Tiotropium in COPD: The UPLIFT Trial. COPD, 1, 303-312. http://dx.doi.org/10.1081/COPD-200026934
- Tashkin, D.P., Celli, B., Senn, S., Burkhart, D., Kesten, S., Menjoge, S. and Decramer, M. (2008) UPLIFT Study Investigators. A 4-Year Trial of Tiotropium in Chronic Obstructive Pulmonary Disease. New England Journal of Medicine, 359, 1543-1554. http://dx.doi.org/10.1056/NEJMoa0805800
- Celli, B., Decramer, M., Kesten, S., Liu, D., Mehra, S. and Tashkin, D.P. (2009) UPLIFT Study Investigators. Mortality in the 4-Year Trial of Tiotropium (UPLIFT) in Patients with Chronic Obstructive Pulmonary Disease. American Journal of Respiratory and Critical Care Medicine, 180, 948-955. http://dx.doi.org/10.1164/rccm.200906-0876OC
- Loganathan, R.S., Stover, D.E., Shi, W. and Venkatraman, E. (2006) Prevalence of COPD in Women Compared to Men around the Time of Diagnosis of Primary Lung Cancer. Chest, 129, 1305-1312. http://dx.doi.org/10.1378/chest.129.5.1305
- Young, R.P., Hopkins, R.J., Christmas, T., Black, P.N., Metcalf, P. and Gamble, G.D. (2009) COPD Prevalence Is Increased in Lung Cancer, Independent of Age, Sex and Smoking History. European Respiratory Journal, 34, 380-386. http://dx.doi.org/10.1378/chest.129.5.1305
- Bednarek, M., Maciejewski, J., Wozniak, M., Kuca, P. and Zielinski, J. (2008) Prevalence, Severity and Underdiagnosis of COPD in the Primary Care Setting. Thorax, 63, 402-407. http://dx.doi.org/10.1136/thx.2007.085456
- Sekine, Y., Kesler, K.A., Behnia, M., Brooks-Brunn, J., Sekine, E. and Brown, J.W. (2001) COPD May Increase the Incidence of Refractory Supraventricular Arrhythmias Following Pulmonary Resection for Non-Small Cell Lung Cancer. Chest, 120, 1783-1790. http://dx.doi.org/10.1378/chest.120.6.1783
- Win, T., Jackson, A., Sharples, L., Groves, A.M., Wells, F.C., Ritchie, A.J. and Laroche, C.M. (2005) Relationship between Pulmonary Function and Lung Cancer Surgical Outcome. European Respiratory Journal, 25, 594-599. http://dx.doi.org/10.1183/09031936.05.00077504
- Nakamura, H., Haruki, T., Adachi, Y., Fujioka, S., Miwa, K. and Taniguchi, Y. (2008) Smoking Affects Prognosis after Lung Cancer Surgery. Surgery Today, 38, 227-231. http://dx.doi.org/10.1007/s00595-007-3599-0
- Celli, B.R., MacNee, W., Agusti, A., Anzueto, A., Berg, B., Buist, A.S., et al. and ATS/ERS Task Force (2004) Standards for the Diagnosis and Treatment of Patients with COPD: A Summary of the ATS/ERS Position Paper. European Respiratory Journal, 23, 932-946. http://dx.doi.org/10.1183/09031936.04.00014304
- Suzuki, H., Sekine, Y., Yoshida, S., Suzuki, M., Shibuya, K., Takiguchi, Y., Tatsumi, K. and Yoshino, I. (2010) Efficacy of Perioperative Administration of Long-Acting Bronchodilator on Postoperative Pulmonary Function and Quality of Life in Lung Cancer Patients with Chronic Obstructive Pulmonary Disease. Preliminary Results of a Randomized Control Study. Surgery Today, 40, 923-930. http://dx.doi.org/10.1007/s00595-009-4196-1
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) Criteria (2014). http://www.goldcopd.org/
- Juhl, B. and Frost, N. (1975) A Comparison between Measured and Calculated Changes in the Lung Function after Operation for Pulmonary Cancer. Acta Anaesthesiologica Scandinavica, 19, 39-45. http://dx.doi.org/10.1111/j.1399-6576.1975.tb05411.x
- Fukuchi, Y., Nishimura, M., Ichinose, M., Adachi, M., Nagai, A., Kuriyama, T., Takahashi, K., Nishimura, K., Ishioka, S., Aizawa, H. and Zaher, C. (2004) COPD in Japan: The Nippon COPD Epidemiology Study. Respirology, 9, 458-465. http://dx.doi.org/10.1111/j.1440-1843.2004.00637.x
- Sekine, Y., Iwata, T., Chiyo, M., Yasufuku, K., Motohashi, S., Yoshida, S., Suzuki, M., Iizasa, T., Saitoh, Y. and Fujisawa, T. (2003) Minimal Alteration of Pulmonary Function after Lobectomy in Lung Cancer Patients with Chronic Obstructive Pulmonary Disease. Annals of Thoracic Surgery, 76, 356-361; Discussion 362. http://dx.doi.org/10.1016/S0003-4975(03)00489-2
- Congleton, J. and Muers, M.F. (1995) The Incidence of Airflow Obstruction in Bronchial Carcinoma, Its Relation to Breathlessness, and Response to Bronchodilator Therapy. Respiratory Medicine, 89, 291-296. http://dx.doi.org/10.1016/0954-6111(95)90090-X
- Hill, K., Goldstein, R.S., Guyatt, G.H., Blouin, M., Tan, W.C., Davis, L.L., Heels-Ansdell, D.M., Erak, M., Bragaglia, P.J., Tamari, I.E., Hodder, R. and Stanbrook, M.B. (2010) Prevalence and Underdiagnosis of Chronic Obstructive Pulmonary Disease among Patients at Risk in Primary Care. Canadian Medical Association Journal, 182, 673-678. http://dx.doi.org/10.1503/cmaj.091784
- Smetana, G.W., Lawrence, V.A., Cornell, J.E. and American College of Physicians (2006) Preoperative Pulmonary risk Stratification for Noncardiothoracic Surgery: Systematic Review for the American College of Physicians. Annals of Internal Medicine, 144, 581-595. http://dx.doi.org/10.7326/0003-4819-144-8-200604180-00009
- Markos, J., Mullan, B.P., Hillman, D.R., Musk, A.W., Antico, V.F., Lovegrove, F.T., Carter, M.J. and Finucane, K.E. (1989) Preoperative Assessment as a Predictor of Mortality and Morbidity after Lung Resection. American Review of Respiratory Disease, 139, 902-910. http://dx.doi.org/10.1164/ajrccm/139.4.902
- Leo, F., Venissac, N., Pop, D., Solli, P., Filosso, P., Minniti, A., Radice, D. and Mouroux, J. (2008) Postoperative Exacerbation of Chronic Obstructive Pulmonary Disease. Does It Exist? European Journal Cardio-Thoracic Surgery, 33, 424-429. http://dx.doi.org/10.1016/j.ejcts.2007.11.024
- Lawrence, V.A., Cornell, J.E., Smetana, G.W. and American College of Physicians (2006) Strategies to Reduce Postoperative Pulmonary Complications after Noncardiothoracic Surgery: Systematic Review for the American College of Physicians. Annals of Internal Medicine, 144, 596-608. http://dx.doi.org/10.7326/0003-4819-144-8-200604180-00011
- Kobayashi, S., Suzuki, S., Niikawa, H., Sugawara, T. and Yanai, M. (2009) Preoperative Use of Inhaled Tiotropium in Lung Cancer Patients with Untreated COPD. Respirology, 14, 675-679. http://dx.doi.org/10.1111/j.1440-1843.2009.01543.x
- Calverley, P.M., Anderson, J.A., Celli, B., Ferguson, G.T., Jenkins, C., Jones, P.W., Yates, J.C., Vestbo, J. and TORCH Investigators (2007) Salmeterol and Fluticasone Propionate and Survival in Chronic Obstructive Pulmonary Disease. New England Journal of Medicine, 356, 775-789. http://dx.doi.org/10.1056/NEJMoa063070
- Bolükbas, S., Eberlein, M., Eckhoff, J. and Schirren, J. (2011) Short-Term Effects of Inhalative Tiotropium/Formoterol/Budenoside versus Tiotropium/Formoterol in Patients with Newly Diagnosed Chronic Obstructive Pulmonary Disease Requiring Surgery for Lung Cancer: A Prospective Randomized Trial. European Journal Cardio-Thoracic Surgery, 39, 995-1000. http://dx.doi.org/10.1016/j.ejcts.2010.09.025
- Anthonisen, N.R. and Wright, E.C. (1986) Bronchodilator Response in Chronic Obstructive Pulmonary Disease. American Review of Respiratory Disease, 133, 814-819.
- Anthonisen, N.R., Lindgren, P.G., Tashkin, D.P., Kanner, R.E., Scanlon, P.D., Connett, J.E. and Lung Health Study Research Group (2005) Bronchodilator Response in the Lung Health Study over 11 Yrs. European Respiratory Journal, 26, 45-51. http://dx.doi.org/10.1183/09031936.05.00102604
- Tashkin, D. and Kesten, S. (2003) Long-Term Treatment Benefits with Tiotropium in COPD Patients with and without Short-Term Bronchodilator Responses. Chest, 123, 1441-1449. http://dx.doi.org/10.1378/chest.123.5.1441
- American Thoracic Society (1995) Standardization of Spirometory, 1994 Update. American Journal of Respiratory and Critical Care Medicine, 152, 1107-1136. http://dx.doi.org/10.1164/ajrccm.152.3.7663792
- (1974) Criteria for the Assessment of Reversibility in Airways Obstruction. Report of the Committee on Emphysema American College of Chest Physicians. Chest, 65, 552-553.
- Brand, P.L., Quanjer, P.H., Postma, D.S., Kerstjens, H.A., Ko?ter, G.H., Dekhuijzen, P.N. and Sluiter, H.J. (1992) Interpretation of Bronchodilator Response in Patients with Obstructive Airways Disease. The Dutch Chronic Non-Specific Lung Disease (CNSLD) Study Group. Thorax, 47, 429-436. http://dx.doi.org/10.1136/thx.47.6.429�
- Eliasson, O. and Degraff Jr., A.C. (1985) The Use of Criteria for Reversibility and Obstruction to Define Patient Groups for Bronchodilator Trials. Influence of Clinical Diagnosis, Spirometric, and Anthropometric Variables. American Review of Respiratory Disease, 132, 858-864.
- Ueda, K., Hayashi, M., Tanaka, N., Tanaka, T. and Hamano, K. (2014) Long-Term Pulmonary Function after Major Lung Resection. General Thoracic and Cardiovascular Surgery, 62, 24-30. http://dx.doi.org/10.1007/s11748-013-0346-x
- Colice, G.L., Shafazand, S., Griffin, J.P., Keenan, R., Bolliger, C.T. and American College of Chest Physicians (2007) Physiologic Evaluation of the Patient with Lung Cancer Being Considered for Resectional Surgery: ACCP Evidenced-Based Clinical Practice Guidelines (2nd Edition). Chest, 132, 161S-177S.
- Bremer, J.L. (1936) The Fate of the Remaining Lung Tissue after Lobectomy or Pneumonectomy. The Journal of Thoracic Surgery, 6, 336-343.
- Endoh, H., Tanaka, S., Yajima, T., Ito, T., Tajima, K., Mogi, A., Shitara, Y. and Kuwano, H. (2010) Pulmonary Function after Pulmonary Resection by Posterior Thoracotomy, Anterior Thoracotomy or Video-Assisted Surgery. European Journal Cardio-Thoracic Surgery, 37, 1209-1214. http://dx.doi.org/10.1016/j.ejcts.2009.11.016
- Nakata, M., Saeki, H., Yokoyama, N., Kurita, A., Takiyama, W. and Takashima, S. (2000) Pulmonary Function after Lobectomy: Video-Assisted Thoracic Surgery versus Thoracotomy. Annals of Thoracic Surgery, 70, 938-941. http://dx.doi.org/10.1016/S0003-4975(00)01513-7
- Sciurba, F.C., Rogers, R.M., Keenan, R.J., Slivka, W.A., Gorcsan III, J., Ferson, P.F., Holbert, J.M., Brown, M.L. and Landreneau, R.J. (1996) Improvement in Pulmonary Function and Elastic Recoil after Lung-Reduction Surgery for Diffuse Emphysema. New England Journal of Medicine, 334, 1095-1099. http://dx.doi.org/10.1056/NEJM199604253341704
- Jubran, A., Laghi, F., Mazur, M., Parthasarathy, S., Garrity Jr., E.R., Fahey, P.J. and Tobin, M.J. (1998) Partitioning of Lung and Chest-Wall Mechanics before and after Lung-Volume-Reduction Surgery. American Journal of Respiratory and Critical Care Medicine, 158, 306-310. http://dx.doi.org/10.1164/ajrccm.158.1.9706082
- Laghi, F., Jubran, A., Topeli, A., Fahey, P.J., Garrity Jr., E.R., De Pinto, D.J., Tobin, M.J. and Loyola/Hines Lung Volume Reduction Surgery Research Group (2004) Effect of Lung Volume Reduction Surgery on Diaphragmatic Neuromechanical Coupling at 2 Years. Chest, 125, 2188-2195. http://dx.doi.org/10.1378/chest.125.6.2188
- Rapicetta, C., Tenconi, S., Voltolini, L., Luzzi, L., Scala, V. and Gotti, G. (2011) Impact of Lobectomy for Non-Small-Cell Lung Cancer on Respiratory Function in Octogenarian Patients with Mild to Moderate Chronic Obstructive Pulmonary Disease. European Journal Cardio-Thoracic Surgery, 39, 555-559. http://dx.doi.org/10.1016/j.ejcts.2010.07.043
- Korst, R.J., Ginsberg, R.J., Ailawadi, M., Bains, M.S., Downey Jr., R.J., Rusch, V.W. and Stover, D. (1998) Lobectomy Improves Ventilatory Function in Selected Patients with Severe COPD. Annals of Thoracic Surgery, 66, 898-902. http://dx.doi.org/10.1016/S0003-4975(98)00697-3
- Zeiher, B.G., Gross, T.J., Kern, J.A., Lanza, L.A. and Peterson, M.W. (1995) Predicting Postoperative Pulmonary Function in Patients Undergoing Lung Resection. Chest, 108, 68-72. http://dx.doi.org/10.1378/chest.108.1.68
- Ginsberg, R.J. and Rubinstein, L.V. (1995) Randomized Trial of Lobectomy versus Limited Resection for T1 No Non-Small Cell Lung Cancer. Lung Cancer Study Group. Annals of Thoracic Surgery, 60, 615-622; Discussion 622-623. http://dx.doi.org/10.1016/0003-4975(95)00537-U
- Bolliger, C.T., Jordan, P., Solèr, M., Stulz, P., Tamm, M., Wyser, C., Gonon, M. and Perruchoud, A.P. (1996) Pulmonary Function and Exercise Capacity after Lung Resection. European Respiratory Journal, 9, 415-421. http://erj.ersjournals.com/content/9/3/415.long
- Funakoshi, Y., Takeda, S., Sawabata, N., Okumura, Y. and Maeda, H. (2005) Long-Term Pulmonary Function after Lobectomy for Primary Lung Cancer. Asian Cardiovascular and Thoracic Annals, 13, 311-315. http://dx.doi.org/10.1177/021849230501300404
- Wang, J.S., Abboud, R.T. and Wang, L.M. (2006) Effect of Lung Resection on Exercise Capacity and on Carbon Monoxide Diffusing Capacity during Exercise. Chest, 129, 863-872. http://dx.doi.org/10.1378/chest.129.4.863
- Brunelli, A., Xiumé, F., Refai, M., Salati, M., Marasco, R., Sciarra, V. and Sabbatini, A. (2007) Evaluation of Expiratory Volume, Diffusion Capacity, and Exercise Tolerance Following Major Lung Resection: A Prospective Follow-Up Analysis. Chest, 131, 141-147. http://dx.doi.org/10.1378/chest.06-1345
- Win, T., Groves, A.M., Ritchie, A.J., Wells, F.C., Cafferty, F. and Laroche, C.M. (2007) The Effect of Lung Resection on Pulmonary Function and Exercise Capacity in Lung Cancer Patients. Respiratory Care, 52, 720-726. http://rc.rcjournal.com/content/52/6/720.full.pdf+html
- Kearney, D.J., Lee, T.H., Reilly, J.J., DeCamp, M.M. and Sugarbaker, D.J. (1994) Assessment of Operative Risk in Patients Undergoing Lung Resection—Importance of Predicted Pulmonary Function. Chest, 105, 753-759. http://dx.doi.org/10.1378/chest.105.3.753
- Imaeda, T., Kanematsu, M., Asada, S., Seki, M., Matsui, E., Doi, H., Sakai, S., Kokubo, M. and Hirose, H. (1995) Prediction of Pulmonary Function after Resection of Primary Lung Cancer. Utility of Inhalation-Perfusion SPECT Imaging. Clinical Nuclear Medicine, 20, 792. http://dx.doi.org/10.1097/00003072-199509000-00007
- Giordano, A., Calcagni, M.L., Meduri, G., Valente, S. and Galli, G. (1997) Perfusion Lung Scintigraphy for the Prediction of Postlobectomy Residual Pulmonary Function. Chest, 111, 1542-1547. http://dx.doi.org/10.1378/chest.111.6.1542
- Wu, M.T., Chang, J.M., Chiang, A.A., Lu, J.Y., Hsu, H.K., Hsu, W.H. and Yang, C.F. (1994) Use of Quantitative CT to Predict Postoperative Lung Function in Patients with Lung Cancer. Radiology, 191, 257-262. http://dx.doi.org/10.1148/radiology.191.1.8134584
- Sangalli, M., Spiliopoulos, A. and Mrgevand, R. (1992) Predictability of FEV1 after Pulmonary Resection for Bronchogenic Carcinoma. European Journal Cardio-Thoracic Surgery, 6, 242-245. http://dx.doi.org/10.1016/1010-7940(92)90105-7
- Haruki, T., Nakamura, H., Taniguchi, Y., Miwa, K., Adachi, Y. and Fujioka, S. (2010) “Lung Age” Predicts Post-Opeartive Complications and Survival in Lung Cancer Patients. Respirology, 15, 495-500. http://dx.doi.org/10.1111/j.1440-1843.2010.01708.x
NOTES

*Corresponding author.


