Chinese Medicine
Vol.08 No.01(2017), Article ID:75063,9 pages
10.4236/cm.2017.81004
Acupuncture Point Injection of Vitamin K1 to Treat Severe Primary Dysmenorrhea: Case Series at a Women’s Health Service in Bologna
Grazia Lesi1*, Annagiulia Gramenzi2, Clarissa Frascà3, Francesco Cardini4, Clede Maria Garavini1
1Family Planning Clinic, Bologna Local Health Unit, Bologna, Italy
2Department of Medical and Surgical Science, University of Bologna, Bologna, Italy
3Gynecology and Pathophysiology of Human Reproduction Unit, S. Orsola-Malpighi Hospital, University of Bologna, Bologna, Italy
4Healthcare and Social Agency of Emilia-Romagna Region, Bologna, Italy

Copyright © 2017 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: February 19, 2017; Accepted: March 28, 2017; Published: March 31, 2017
ABSTRACT
Introduction and Aim: Vitamin K acupuncture point injection is an effective and safe menstrual pain treatment derived from Traditional Chinese Medicine, commonly used in some Chinese hospitals. This case series investigated the effectiveness and safety of vitamin K acupuncture point injection on menstrual pain in patients with severe primary dysmenorrhea at a regional public health clinic at Bologna, Italy. Methods: From September 2006 to July 2010, 24 women were enrolled and treated during their first day of menstrual pain with an injection of 1 ml of solution containing 5 mg of vitamin K1 in an acupuncture point San Yin Jiao/Spleen 6 (SP6) bilaterally on the inside of each lower leg above the ankle. Results: Treatment was well tolerated and no major adverse events were reported. Pain relief was observed starting from 2 minutes after treatment and within 30 minutes. All treated women but one (96%) reported a substantial pain reduction (p < 0.001). During the six post-treatment follow-up cycles, a trend toward a reduction of menstrual distress evaluated by the Cox Pain Intensity and Duration Scales was documented. Women reported fewer daily life restrictions and consumption of fewer analgesic tablets when compared to what they reported at the pre-treatment cycle. Conclusions: The results of this case series indicate that in primary dysmenorrhea a single vitamin K1 injection in the SP6 acupuncture point has an immediate pain-relieving effect and may ameliorate menstrual pain intensity and duration in post-treatment follow-up cycles.
Keywords:
Primary Dysmenorrhea, Acupuncture, Vitamin K

1. Introduction
Primary dysmenorrhoea is painful uterine cramping occurring just before or during menstruation in the absence of detectable pathologic conditions [1] . It is a common gynaecological complaint affecting more than 50% of menstruating women, especially those who are young [1] . In its severe form, primary dysmenorrhoea is a frequent cause of work or school absenteeism and affects personal as well as economic aspects of life [2] [3] . Conventional treatments include non- steroidal anti-inflammatory drugs (NSAIDs) and oral contraceptives. The efficacy of these treatments is high, but 20% - 25% of women have inadequate pain relief [4] - [11] . Moreover, both NSAIDs and oral contraceptives have side effects and their use is not without risk. Therefore, other approaches are needed. Clinical studies suggest that acupuncture may play a role in managing primary dysmenorrhoea, but the evidence is limited [12] [13] .
Injection of a drug, vitamin, saline solution, or plant extract into an acupuncture point is an innovation of traditional acupuncture aiming to enhance and prolong the effect of stimulation of acupuncture points. Vitamin K acupuncture point injection is a menstrual pain treatment derived from Traditional Chinese Medicine, commonly used in some Chinese hospitals since the 1980s. Researchers at the Obstetrics & Gynaecology Hospital in Shanghai, first reported that vitamin K3 injection into muscle could relieve primary dysmenorrhea within 30 minutes [14] . A subsequent study showed that vitamin K3 injection at the acupuncture point San Yin Jiao/Spleen 6 (SP6) could relieve menstrual pain more quickly than in muscle [15] . A pilot study conducted in China and Italy confirmed that injections of vitamin K (various types) alleviate acute menstrual pain and extended relief throughout the non-treatment follow-up cycles [16] . Indeed, vitamin K seems to relax uterine muscle spasms caused by noradrenaline or pro- staglandin F2-alpha [15] [16] . These favourable results have been further substantiate in Chinese women by a very recent double-blind randomised controlled trial using vitamin K3 acupuncture point injection [17] .
This case series study investigated the effectiveness, safety and acceptability of vitamin K injection into the SP6 acupuncture point on menstrual pain in patients with severe primary dysmenorrhea in an Italian public health clinic.
2. Patients and Methods
The study was conducted at the outpatient Family Planning Clinic, Local Health Unit, Bologna, Italy. Nulliparous women aged 14 - 25 years were enrolled on the basis of the following inclusion criteria: no history or evidence of pelvic pathologyas confirmed by agynecological examination, regular menstrual cycles (28 day cycle ± 7 days) for the previous 6 months and severe primary dysmenorrhea for at least six months. According to the criteria of a Primary Dysmenorrhea Consensus Guideline [18] , severe dysmenorrhea was defined as “severe recurrent menstrual pain, with or without general accompanying symptoms, that interrupts normal activities for hours or days and that is not relieved, or not totally relieved, by any previous treatment”. The exclusion criteria were:use of hormonal contraceptives or intrauterine devices, pregnancy, dysmenorrheal due to any other suspected or established cause, history of abdominal surgery and concomitant therapy for acute or chronic pain due to any other cause, ongoing anti-coagulant therapy for any reason, previous treatment with needle-injection of Vitamin K for any reason, known hypersensitivity to vitamin K. All participating women were required to have a working phone. Patients with plans to move their residence beyond the catchment area of the clinic in the next 7 months or those without the ability to give consent did not participate.
The cases reported here were part of an integrated medicine network for teenagers and young women in Bologna. The study was approved by the Ethics Committee of the Local Health Unit of Bologna. All the studied patients provided informed consent for participation to the study. Minors only participated with parental consent.
Women were treated during the first day of menstrual pain at the cycle after enrollment. The subject’s skin around the SP6 acupuncture point was sterilized, a 22-gauge syringe needle was inserted at the point, and 1 ml of solution containing 5 mg of vitamin K1 was injected in the SP6 point bilaterally on each leg. After the injection, the injection site was pressed with a sterilized pad to prevent infection. The short-term effect of the treatment on menstrual pain intensity was evaluated by means of a 0- to 10-cm numeric rating scale (NRS) before and at 2, 5 and 30 minutes after the vitamin K acupuncture injection. Presence, type and intensity of side effects were also recorded.
Menstrual distress during the post-treatment follow-up cycles was measured with a Retrospective Symptom Scale of Menstrual Distress [19] for assessing average intensity (Cox1 score) and total duration (Cox2 score) of menstrual distress at baseline and for a total of 6 post-treatment cycles. At each follow-up cycle patients were also asked to record hours spent in bed, hours of absence from school/work and numbers of analgesic tablets taken to relieve pain.
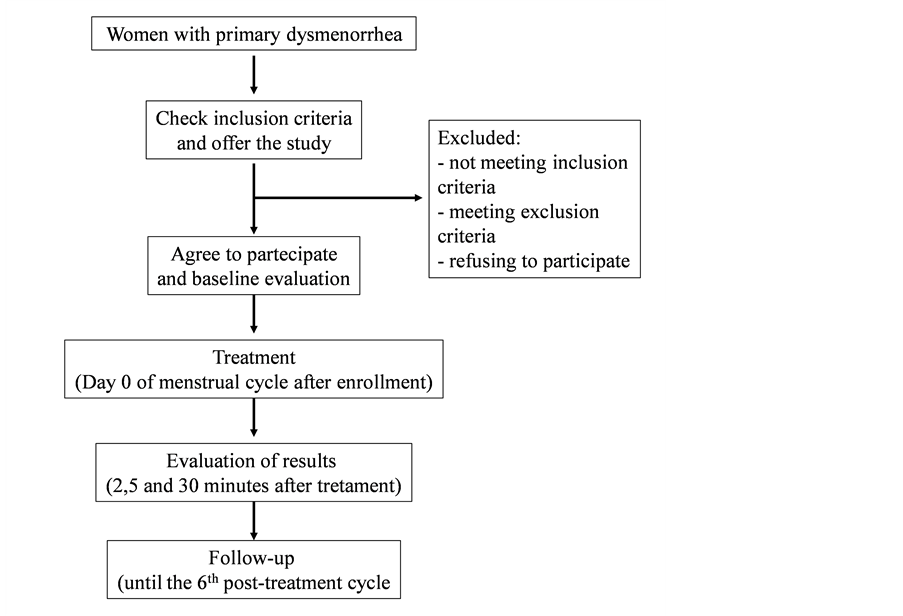
Figure 1 shows a flow diagram of the study design. The time points of the study were as follows:
1) Baseline (before treatment):
a) Retrospective symptom scale of menstrual distress (Cox1 and Cox2 scores)
b) Hours spent in bed, absence (hours) from school/work, numbers of analgesic tablet taken to relieve pain
2) Two, 5 and 30 minutes after treatment
a) Pain evaluation by means of NRS
b) Patient satisfaction questionnaire
3) Post-treatment follow-up cycles
a) Retrospective symptom scale of menstrual distress (Cox1 and Cox2 scores)
b) Hours spent in bed, absence (hours) from school/word, numbers of analgesic tablet of analgesic tablets taken to relieve pain
Data are expressed as mean ± standard deviation or median (range) as appropriated. Non-parametric tests were used to compare NRS scores, Cox 1 (pain
Figure 1. Flow diagram of study design.
duration) and Cox 2 (pain intensity) scores, hours spent in bed, hours of absence from school/work, numbers of analgesic tablets. The statistical analysis was performed using SPSS 13.0 for Windows.
Statistical significance was set at p-value less than 0.05.
3. Results
From September 2006 to July 2010, 24 women gave their informed consent and were enrolled. Baseline data on participant demographics and on menstrual cycle characteristics were collected and summarized in Table 1. Among the 24 enrolled women, 16 (66.7%) usually had dysmenorrhea during bleeding, 2 (8.3%) only before bleeding began, 5 (20.8%) before and during bleeding and 1 (4.2%) before, during and after bleeding. Table 2 shows the menstrual pain and distress characteristics at baseline
Treatment was well tolerated with no major adverse events reported. Reported side effects were transient, of short duration and fully reversible without any additional treatment. In particular 17 patients experienced pain and/or tenderness in the injection site, two felt light-headed (faint) and one complained of foot paresthesia.
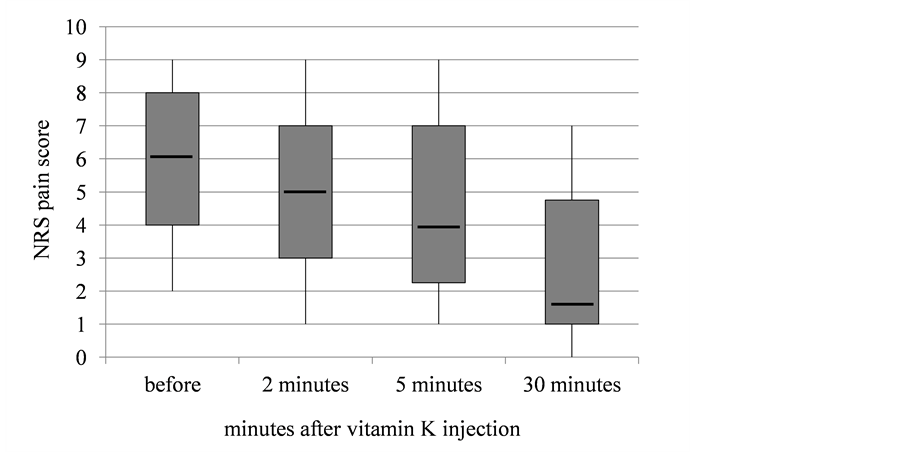
After the injection of vitamin K1 in the SP6 point the decrease of pain as measured by the NRS over time (Figure 2) was statistically significant (Friedman test, p < 0.001), with a 4.5 point decrease in pain from baseline (median NRS = 6) to 30 minutes following acu-injection (median NRS = 1.5). Indeed, the highest pain reduction occurred 30 minutes after the treatment, when all women but one (96%) reported a substantial reduction of pain. Four patients (16.7%) had no pain (NRS = 0) 30 minutes after the treatment.
Table 1. Baseline characteristics of enrolled patients (n = 24).
Table 2. Menstrual pain and distress characteristics at baseline.
Figure 2. NRS pain scores (median and interquartile intervals) before and after treatment (Friedman test, p < 0.001).
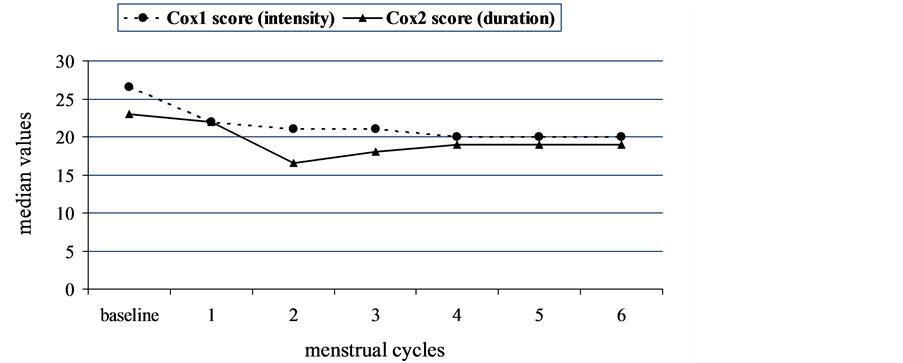
The median Cox1and Cox2 scores (intensity and duration of menstrual distress, respectively) both decreased in the cycles following the treatment cycle, then tended to go up progressively (Figure 3). Indeed, early improvements reported by women were no longer sustained: a statistically significant reduction compared to baseline was observed only until the 5th post-treatment cycle for Cox1 score and until the 3rd for Cox2. Similarly, during follow-up there was a significant improvement in relation to restriction of daily living activities evaluated by the number of hours in bed and the number of hours of absence from school/works (Table 3). This improvement was evident in the early cycles after treatment and then the symptoms tend to return to the initial intensity, even though the consumption of analgesic drugs was reduced for five cycles (Table 3).
At the end of the study period a questionnaire on satisfaction was administered to all the treated women. Sixteen participants (67%) were very satisfied and another 6 (25%) were satisfied. Only 2 participants were dissatisfied or very dissatisfied. Twenty-two women (92%) would have liked to repeat the treatment and 21 of them (88%) affirmed that they would seek the treatment every month, if available. In addition, 23 (96%) would recommend this kind of treatment to a friend. Indeed, 4 patients (16.6%) asked for a second treatment at the end of the study (after about six months).
Figure 3. Median intensity (Cox1) and duration (Cox2) scores of menstrual distress during the study period.
Table 3. Secondary endpoints during the non-treatment follow-up cycles.
*Friedman test.
4. Discussion
The results of this case series show that vitamin K1 injection into the SP6 acupuncture point in young Italian patients with severe primary dysmenorrhea is safe and has a rapid pain-relieving effect. A significant reduction in pain intensity evaluated by an NRS was observed from baseline to 30 minutes post-treat- ment. Relief lasted through several non-treatment follow-up cycles as shown by the Cox scores for pain duration and intensity and by the reports of both daily life restriction and numbers of analgesic tablets consumed. These findings are consistent with those obtained in a previous uncontrolled observational study conducted among young Chinese and Italian women [16] . A pilot study with a crossover design from the USA showed that in young women with primary dysmenhorrea acupuncture injection into the SP6 point decreased pain and that the pain relief was greater for vitamin K1 than for saline acupuncture point injection [20] , suggesting a possible synergistic action between vitamin K1 and SP6 acupuncture point injection. Increased plasma concentration of vitamin K1 after injection at the acupuncture point SP6 was also observed [21] . Recently, in a three-arm randomized controlled trial it has been shown that acupuncture point injection with vitamin K3 in SP6 is able to induce a rapid and long-term pain relief in Chinese women with primary dysmenhorroea [17] . It should be pointed out that the results of this study support the acupuncture point injection site as a crucial aspect of optimal pain relief. The SP6 point is the crossing point of the liver, spleen, and kidney meridians and, according to Traditional Chinese Medicine, its stimulation is proposed to strengthen the spleen, resolve and expel dampness, restore balance of Yin and blood, liver and kidney, and consequently invigorate blood supply and relieve menstrual pain [22] [23] . Thus, the acupuncture point SP6 is commonly selected for treatment of menstrual disorders since it is a crossing point of the liver, spleen and kidney channels. Acupuncture at SP6 may affect the pelvic nerve plexus formed by T5-L1 sympathetic nerve fibers and mediate contractions of uterine myometrium [14] . Recently, a randomized study demonstrated that SP6 acupressure immediately relieves dysmenorrhea and, if applied for three consecutive months, it can relieve both pain and menstrual distress [24] . On the other hand, a potential role of vitamin K in reducing pro-inflammatory cytokines [15] [16] [25] could contribute to the beneficial effect on menstrual pain. However, the mechanisms of action of acupuncture point injection of vitamin K in primary dysmenorrhea are largely unknown. In particular little is known about the difference of the various form of vitamin K.
The main limitations of this work include the small sample size and the lack of a control group. Consequently, a non-specific effect of acupuncture in reducing the menstrual cycle pain cannot be ruled out [12] .
5. Conclusion
In conclusion, vitamin K injection into the SP6 acupuncture point may relieve or attenuate pain in young women with primary dysmenorrhea. Therefore, it could represent an optimal treatment in emergency settings, because it could be administered during the course of pain interrupting it. If the results of this study will be confirmed in further well-designed, randomized clinical studies, vitamin K injection into the SP6 acupuncture point could became part of complementary care pathway devoted to women disease.
Cite this paper
Lesi, G., Gramenzi, A., Frascà, C., Cardini, F. and Garavini, C.M. (2017) Acupuncture Point Injection of Vitamin K1 to Treat Severe Primary Dysmenorrhea: Case Series at a Women’s Health Service in Bologna. Chinese Medicine, 8, 33-41. https://doi.org/10.4236/cm.2017.81004
References
- 1. Ju, H., Jones, M. and Mishra, G. (2014) The Prevalence and Risk Factors of Dysmenorrheal. Epidemiologic Reviews, 36, 104-113.
https://doi.org/10.1093/epirev/mxt009 - 2. Latthe, P., Latthe, M., Say, L., Gülmezoglu, M. and Khan, K.S. (2006) WHO Systematic Review of Prevalence of Chronic Pelvic Pain: A Neglected Reproductive Health Morbidity. BMC Public Health, 6, 177.
https://doi.org/10.1186/1471-2458-6-177 - 3. Iacovides, S., Avidon, I. and Baker, F.C. (2015) What We Know about Primary Dysmenorrhoea Today: A Critical Review. Human Reproduction Update, 21, 762-778.
https://doi.org/10.1093/humupd/dmv039 - 4. Marjoribanks, J., Proctor, M., Farquhar, C. and Ayeleke, R.O. (2015) Nonsteroidal anti-Inflammatory Drugs for Dysmenorrhoea. The Cochrane Database of Systematic Reviews, 7, CD001751.
https://doi.org/10.1002/14651858.CD001751.pub3 - 5. Nor Azlin, M.I., Maryasalwati, I., Norzilawati, M.N., Mahdy, Z.A., Jamil, M.A. and Zainul Rashid, M.R. (2008) The Efficacy of Etoricoxib vs Mefenamic Acid in the Treatment of Primary Dysmenorrhoea: A Randomised Comparative Trial. Journal of Obstetrics and Gynaecology, 28, 424-426.
https://doi.org/10.1080/01443610802150051 - 6. Iacovides, S., Baker, F.C. and Avidon, I. (2014) The 24-H Progression of Menstrual Pain in Women with Primary Dysmenorrhea When Given Diclofenac Potassium: A Randomized, Double-Blinded, Placebo-Controlled Crossover Study. Archives of Gynecology and Obstetrics, 289, 993-1002.
https://doi.org/10.1007/s00404-013-3073-8 - 7. Daniels, S., Gitton, X., Zhou, W., Stricker, K. and Barton, S. (2008) Efficacy and Tolerability of Lumiracoxib 200 mg once Daily for Treatment of Primary Dysmenorrhoea: Results from Two Randomized Controlled Trials. Journal of Women’s Health, 17, 423-437.
https://doi.org/10.1089/jwh.2007.0416 - 8. Daniels, S., Robbins, J., West, C.R. and Nemeth, M.A. (2009) Celecoxib in the Treatment of Primary Dysmenorrhoea: Results from Two Randomized, Double-Blind, Active- and Placebo-Controlled, Crossover Studies. Clinical Therapeutics, 31, 1192-1208.
- 9. Wong, C.L., Farquhar, C., Roberts, H. and Proctor, M. (2009) Oral Contraceptive Pill for Primary Dysmenorrhoea. The Cochrane Database of Systematic Reviews, 4, CD002120.
https://doi.org/10.1002/14651858.CD002120.pub3 - 10. Daniels, J.P. and Khan, K.S. (2010) Chronic Pelvic Pain in Women. BMJ, 341, c4834.
https://doi.org/10.1136/bmj.c4834 - 11. Vercellini, P., Vigano, P. and Somigliana, E. (2005) The Role of the Levonorgestrel-Releasing Intrauterine Device in the Management of Symptomatic Endometriosis. Current Opinion in Obstetrics and Gynecology, 17, 359-365.
https://doi.org/10.1097/01.gco.0000175353.03061.7f - 12. Smith, C.A., Zhu, X., He, L. and Song, J. (2011) Acupuncture for Primary Dysmenorrhoea. The Cochrane Database of Systematic Reviews, 1, CD007854.
https://doi.org/10.1002/14651858.CD007854.pub2 - 13. Chung, Y.C., Chen, H.H. and Yeh, M.L. (2012) Acupoint Stimulation Intervention for People with Primary Dysmenorrhea: Systematic Review and Meta-Analysis of Randomized Trials. Complementary Therapies in Medicine, 20, 353-363.
- 14. Yu, J. and Chao, J.A. (1985) Clinical and Experimental Study of Dysfunctional Dysmenorrhea Treated by Vitamin K. Chinese Journal of New Drugs and Clinical Remedies, 5, 14-16.
- 15. Zhao, W.J., Weng, J.E. and Yu, J. (2000) Clinical Study of Vitamin K3 Acupuncture Point Injection in Treating Pelvic Pain. Chinese Acupuncture & Moxibustion, 20, 393-394.
- 16. Wang, L., Cardini, F., Zhao, W., Regalia, A.L., Wade, C., Forcella, E. and Yu, J. (2004) Vitamin K Acupuncture Pint Injection for Severe Primary Dysmenorrhea: An International Pilot Study. Medscape General Medicine, 6, 45.
- 17. Wade, C., Wang, L., Zhao, W.J., Cardini, F., Kronenberg, F., Gui, S.Q., Ying, Z., Zhao, N.Q., Chao, M.T. and Yu, J. (2016) Acupuncture Point Injection Treatment of Primary Dysmenorrhoea: A Randomised, Double Blind, Controlled Study. BMJ Open, 6, e008166.
https://doi.org/10.1136/bmjopen-2015-008166 - 18. Lefebvre, G., Pinsonneault, O., Antao, V., Black, A., Burnett, M., Feldman, K., Lea, R. and Robert M. (2005) SOGC, Primary Dysmenorrhea Consensus Guideline. Journal of Obstetrics and Gynaecology Canada, 27, 1117-1146.
- 19. Cox, D.J. and Meyer, R.G. (1978) Behavioral Treatment Parameters with Primary Dysmenorrhea. Journal of Behavioral Medicine, 3, 297-310.
https://doi.org/10.1007/BF00846681 - 20. Chao, M.T., Wade, C.M., Abercrombie, P.D. and Gomolak, D. (2014) An Innovative Acupuncture Treatment for Primary Dysmenorrhea: A Randomized, Crossover Pilot Study. Alternative Therapies in Health and Medicine, 20, 49-56.
- 21. Chao, M.T., Wade, C.M. and Booth, S.L. (2014) Increase in Plasma Phylloquinone Concentrations Following Acupoint Injection for the Treatment of Primary Dysmenorrheal. Journal of Acupuncture and Meridian Studies, 7, 151-154.
- 22. Maciocia, G. (2004) Obstetrics and Gynecology in Chinese Medicine. Churchill Livingstone, London.
- 23. Chen, M.N., Chien, L.W. and Liu, C.F. (2013) Acupuncture or Acupressure at the Sanyinjiao (SP6) Acupoint for the Treatment of Primary Dysmenorrhea: A Meta-Analysis. Evidence-Based Complementary and Alternative Medicine, 2013, Article ID: 493038.
https://doi.org/10.1155/2013/493038 - 24. Wong, C.L., Lai, K.Y. and Tse, H.M. (2010) Effects of SP6 Acupressure on Pain and Menstrual Distress in Young Women with Dysmenorrheal. Complementary Therapies in Clinical Practice, 16, 64-69.
- 25. Booth, S.L. (2009) Roles for Vitamin K beyond Coagulation. Annual Review of Nutrition, 29, 89-110.
https://doi.org/10.1146/annurev-nutr-080508-141217
Abbreviations
numeric rating scale (NRS);
non-steroidal anti-inflammatory drugs (NSAIDs);
acupuncture point San Yin Jiao/Spleen 6 (SP6).