Food and Nutrition Sciences
Vol.4 No.10A(2013), Article ID:36834,7 pages DOI:10.4236/fns.2013.410A004
Improvements of Nutrition Behavior Fitness and Body Fatness with a Short-Term after School Intervention Program
![]()
Center for Exercise Metabolism and Nutrition, Department of Public Health, School of Medicine, Sao Paulo State University (UNESP), Botucatu, Brazil.
Email: kmclellan@fmb.unesp.br
Copyright © 2013 Katia Cristina Portero McLellan et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received July 4th, 2013; revised August 4th, 2013; accepted August 11th, 2013
Keywords: Obesity; Lifestyle; School-Based Intervention
ABSTRACT
The prevalence of childhood obesity has been increasing worldwide and lifestyle changes are the most important strategies in managing this prevalence. This study aimed to describe the intervention effects of nutrition and physical activities offered as an after school short-term on outcomes of healthy nutrition practices, fitness and lowering fatness. This quasi-experimental study was conducted with a convenience sample of 59 caucasian children, aged 7.7 ± 1.4 years old (52.5% girls) registered on a private school of a middle-size town located in Sao Paulo State, Brazil. The school-based 12-week intervention consisted of 2 weekly 60 minutes section, during 3 months, including a nutritional education and a physical activity curriculum. Anthropometric data was measured for all children at baseline and after 12 weeks. All parents were contacted and requested to complete questionnaire about child’s eating behavior at baseline and after the 12-week program. After the intervention, children showed an increasing in the intake of fruits (64.3%), vegetables (61.9%), and water (52.0%). Overall, 83.3% of the children changed eating behavior according to the questionnaire responded by the parents. Waist circumference was significantly lower and abdominal strength improved after participating in the intervention program. Mean height and weight were significantly higher in boys and girls after a 12-week intervention. Although mean values of BMI remained the same after the intervention it was observed a decreasing in the prevalence of obesity among the children. Thus our study showed that a school-based intervention program focused on nutritional education and physical activity program promoted waist circumference reduction and decreased obesity without affecting the height growth along with improved fitness and healthy eating behavior. This intervention program would be feasible and replicable in others schools around the country.
1. Introduction
The prevalence of childhood obesity has been increasing in developed [1] and developing [2] countries. Data from the 2008-2009 Brazilian Household Survey indicated that approximately 33.5% of children (ages 5 - 9 years) and 20.5% of adolescents (ages 10 - 19 years) are above the weight considered healthy by the World Health Organization (WHO). Obesity prevalence increased from 2.3% to 14% (ages 5 to 9 years) and 0.5% to 5% (ages 10 to 19 years) between 1974-1975 and 2008-2009 [3,4]. Obese children are more likely to become obese adults [5,6] and are at a higher risk of developing adverse health conditions such type 2 diabetes mellitus, the early-onset metabolic syndrome, subclinical inflammation, dyslipidemia, coronary artery diseases [2], and psychosocial outcomes [7]. The metabolic syndrome rates in Brazilian childhood are available from regional studies and range from 4% to 42.4% [8-12].
The increasing prevalence of obesity is due to complex interactions between genetic and environmental factors such as dietary intake and physical activity. The most important factors underling the obesity epidemic are high caloric intake coupled with limited energy expenditure [13]. Both obesity and excessive abdominal adiposity predispose children to be unfit in abdominal strength/ resistance and aerobic resistance. Excess of body adiposity increase the likelihood of poor trunk flexibility [14]. Moreover, low physical fitness is associated with higher sedentary behavior illustrated by the TV time [15].
Because of the increasing public health importance of childhood obesity, many intervention studies have been conducted in developed and developing countries. These studies performed interventions during school time [16- 20], or after school hours [21-26], aiming various target outcomes such as nutrition education [18,20], physical activity [16,21-23] or a combination of these approaches [17,19,24-26].
A recent meta-analysis showed that school-based interventions that contain a physical activity component may be effective in helping to reduce BMI in children [27]. Therapeutic lifestyle changes and maintenance of regular physical activity are the most important strategies in managing childhood obesity [2,28]. The present study aimed to describe the intervention effects of nutrition and physical activities offered as an after school short-term outcomes of healthy nutrition practices, fitness and lowering fatness.
2. Methods
This quasi-experimental study was conducted with a convenience sample of 59 caucasian children (first to fifth grade students), aged 7.7 ± 1.4 years old (52.5% girls) from a private school of Sao Paulo State, Brazil. The study’s aims and methods were presented to children’s parents at the beginning of the academic year. Parents gave written consent for their children to participate in the study. Participating children were free of motor disorders that could impede participation in the physical activity education program. The study was approved by the Research Ethics Committee of School of Medicine of Sao Paulo State University—UNESP/Botucatu (protocol 579/2006).
The study was designed to be a school-based 12-week intervention, including a nutritional education and a physical activity program in which the children engaged in twice a week for 60 minutes. This program has been implemented in the school since 2005. It has been developed by the Nutritional and Exercise Metabolism Centre (CeMENutri) of the UNESP-Medical School which is a multi-professional teaching and research centre located in Botucatu city, a middle size city (in 2010, there were 127,328 inhabitants), in a middle western part of Sao Paulo, a Brazilian southeast state.
2.1. Measurements
Anthropometric measurements, including weight (kg), height (cm), waist circumference (WC) were obtained according to standard protocols (WHO 1995). All the measurements were assessed the week before and immediately after the intervention program. Body Mass index was calculated for all the children. The diagnosis of overweight was based on the BMI equal to or higher than the 85th percentile and lower than the 95th percentile, and obesity was considered a BMI equal to or higher than the 95th percentile [28]. Waist circumference values and percentiles were classified according to McCarthy et al. (2001) [29].
Fitness tests including flexibility and abdominal strength/ resistance were measured according to standards protocols [30].
2.2. Intervention
The nutrition education and physical activity program were conducted both by certified professionals. The program consisted of two 60-minutes section per week, during 3 months. The intervention aimed to improve knowledge, attitudes and eating habits of the children along with increasing daily exercise. The program included lectures and information about human body, the importance of energy and nutrients, consequences of physical inactivity and high energy intake. It also included cooking classes, games and discussions about healthy/unhealthy food and drink, composition of food and drink, and the children’s nutritional pyramid (Figure 1). The nutritionist had presented the nutrition and activity material in an engaging, interactive manner to encourage the children’s participation. After each nutrition education session a healthy snack was provided for every child. Healthy cooking workshops were performed by a certified nutritionist where nutrition education focused on the increasing intake of fruits and vegetables and whole grain products, and the decreasing intake of foods rich in fat, salt and sugar. A healthy meals/recipes book was developed to achieve children’s needs and provided to the parents. The physical activity program combined games for outdoors and activity games, looking for coordination and flexibility improvements.
2.3. Qualitative Questionnaire
All parents were contacted and requested to complete questionnaire after the 12-week intervention program. Parents were queried about the project content and changes in children’s eating behavior (Figure 2).
2.4. Statistical Analysis
The analyses were performed by using SAS, version 9.1. The data were described as mean ± SD. Sample normality was tested by means of the Shapiro-Wilk test. Difference between baseline and after 12-week intervention of
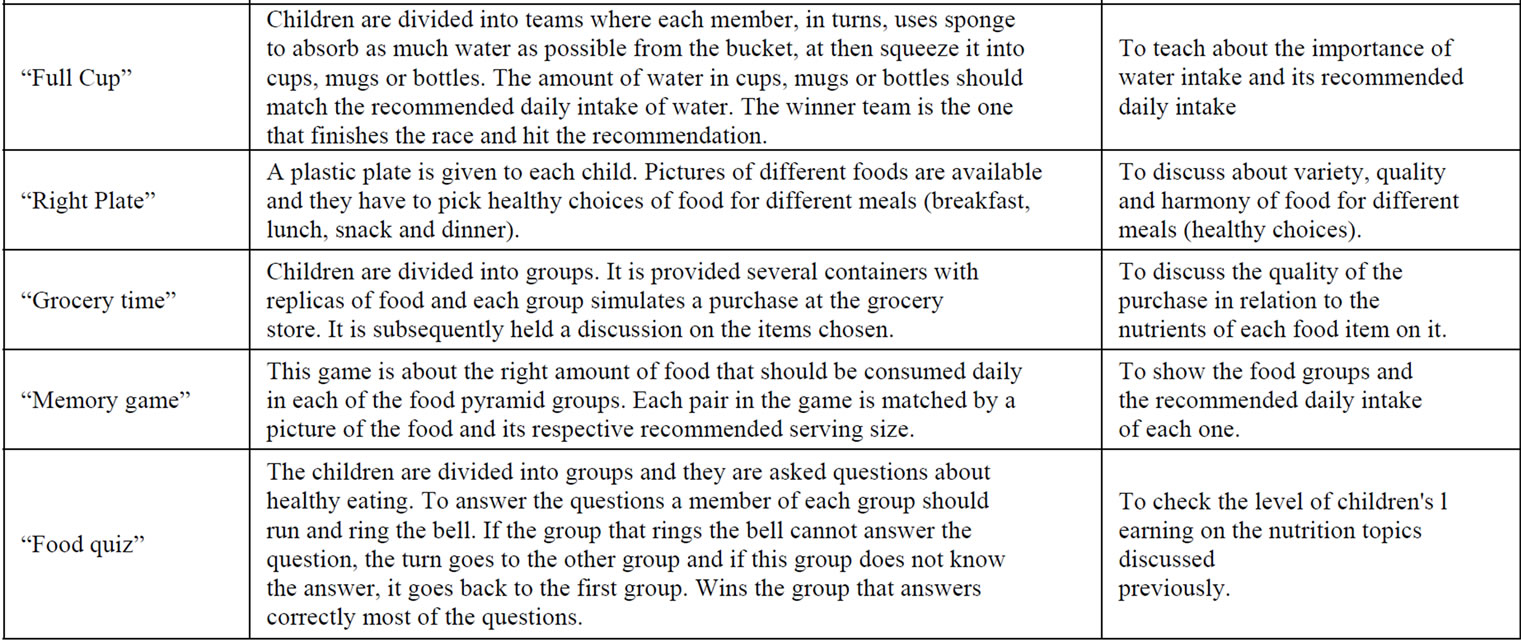
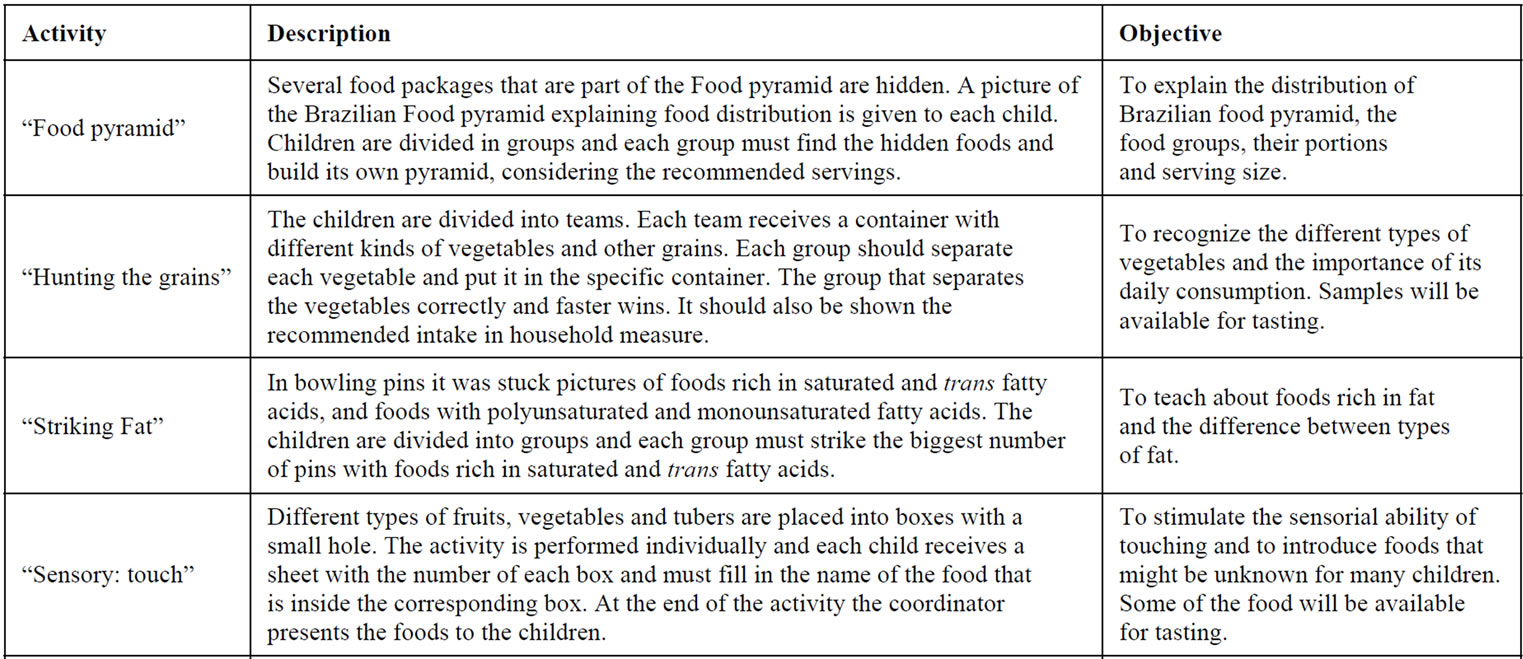
Figure 1. Activities performed during the program.
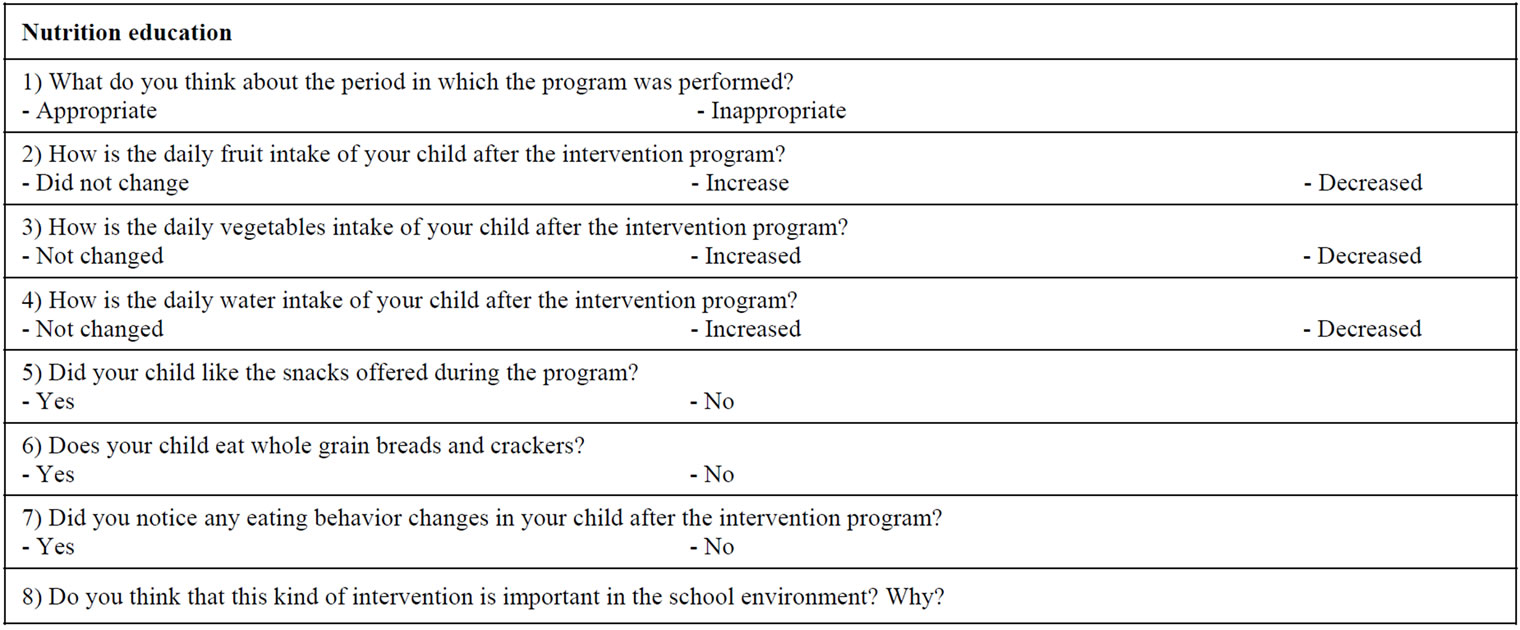
Figure 2. Questionnaire sent to parents after the intervention program.
variables was analyzed by paired student’s t test after. The effect between categories of BMI, WC, flexibility, strength/abdominal resistance and aerobic resistance was analyzed by means of chi-square test. The results were discussed based on the level of significance of p < 0.05.
3. Results
The characteristics of the study population at baseline and after the intervention are shown in Table 1. Mean height was significantly higher by 2.0 cm among boys and 1.0 cm among girls after a 12-week intervention. Body weight was also higher by 0.54 kg among boys and 0.57 kg among girls. Although mean values of BMI remained the same after the intervention it was noticed a decrease in the prevalence of obesity of among the children. Waist circumference was significantly lower and abdominal strength improved after participating in the intervention program. It was also noticed that flexibility improved among girls and aerobic resistance decreased among boys after 12 weeks of intervention.
There were no statistically significant differences in the nutritional status and fitness of children after the intervention. However, the prevalence of obesity decreased in 3.4%, abnormal waist circumference decreased in 6.8%, and abnormal strength/abdominal resistance decreased in 17% (Table 2).
Analysis of children’s food behavior after the intervention program showed an increase in the intake of fruits (64.3%), vegetables (61.9%), and water (52.0%). Overall, 83.3% of the children changed eating behavior according to the questionnaire responded by the parents (Table 3).
Table 1. Characteristics of the study population at baseline and after a 12-week intervention.
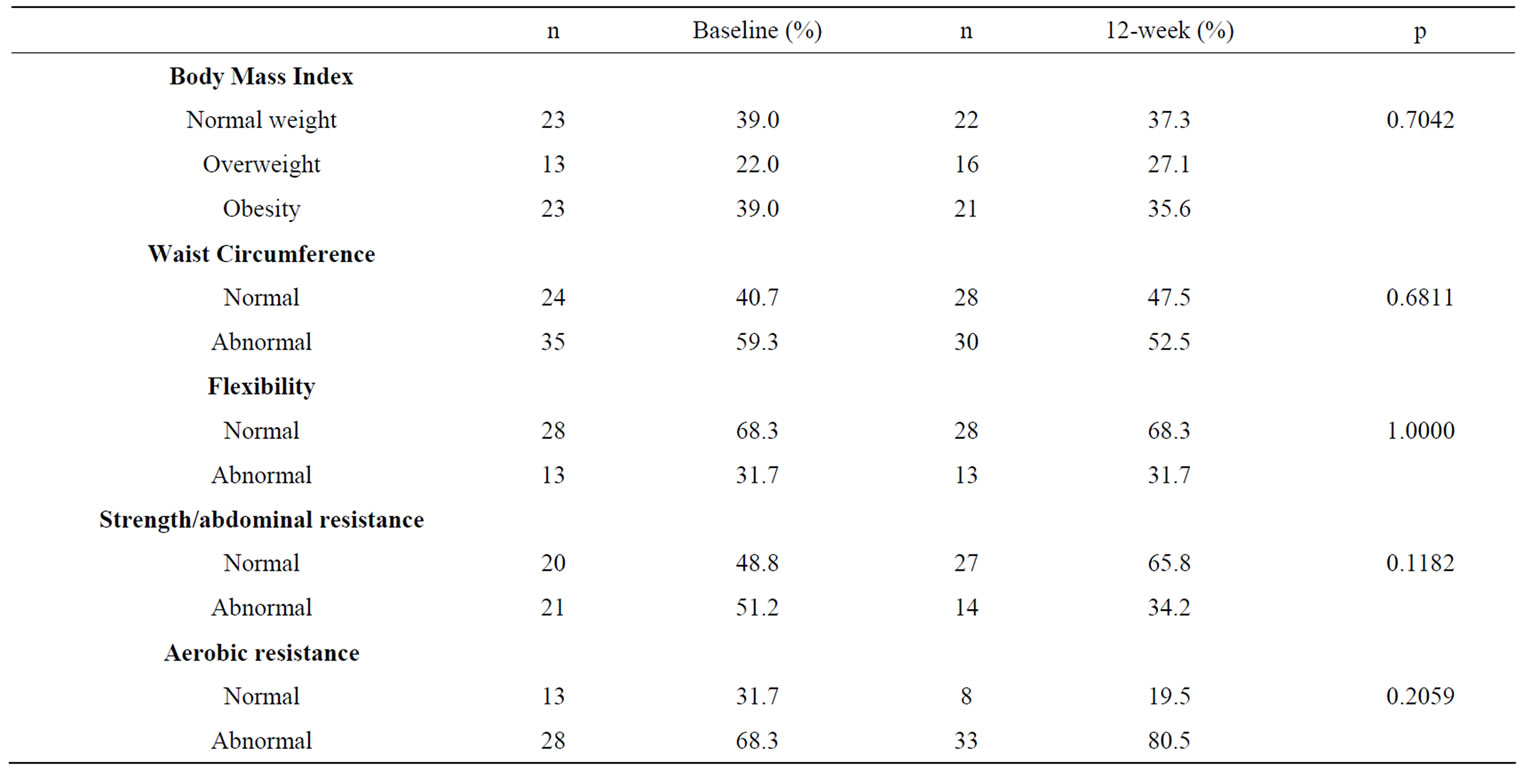
Table 2. Nutritional status and fitness of the study population at baseline and after a 12-week intervention.
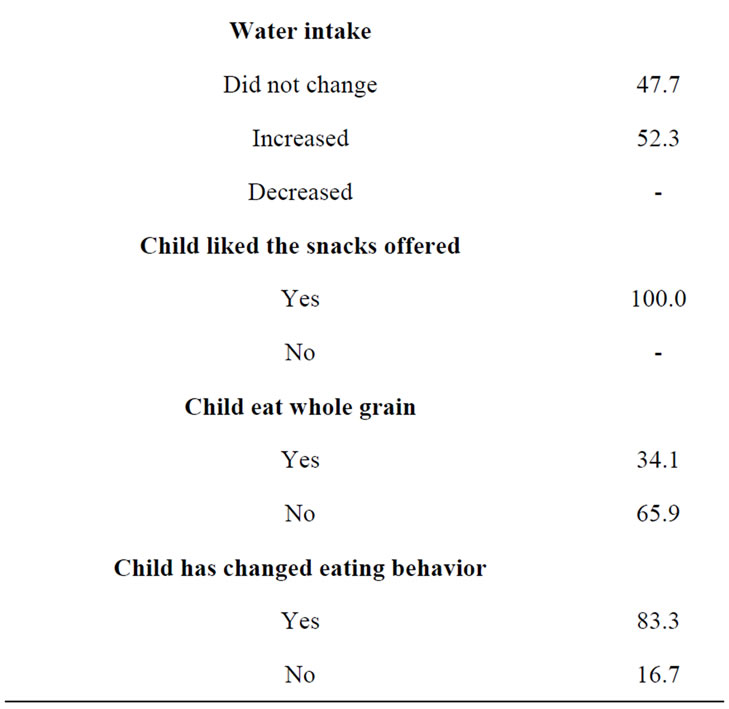
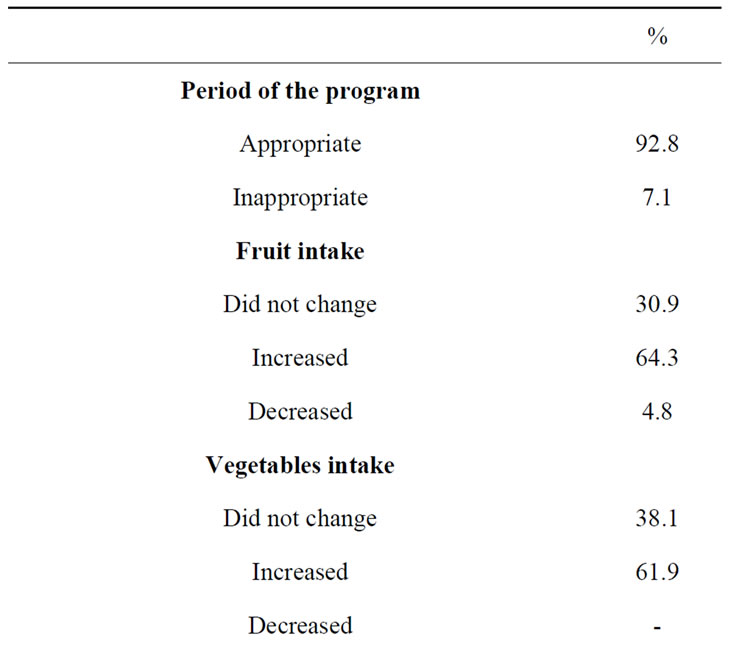
Table 3. Qualitative questionnaire about child’s eating behavior after the intervention program.
4. Discussion
The purpose of our study was to document the results of a short-term school-based intervention program on lifestyle (nutrition and physical activity) of Brazilian children. The improvement of fitness and eating behavior led to a decrease in the prevalence of obesity, suggesting that it may be possible to control/reduce this problem in schools. The program not only decreased the prevalence of obesity but also improve children’s fitness by increasing abdominal strength and physical resistance. Moreover, our intervention program improved children dietary quality by increasing the intake of fruits, vegetables and water. We believe that the parental involvement in this program played an important role in child’s eating behavior changes as they were informed of the purpose of the study and were informed about their child’s nutrition status over time. Besides, parental involvement increases participation of children in the program and help children makes the right choices and planning a balanced meal. The implementation of this short-term after-school intervention was successful and well accepted by parents and children.
Many intervention programs promoting physical activity and healthy diet have been demonstrated to be effective in several countries [24,26,31-33]. Most interventions showed improvement in health knowledge and health-related behaviors, including consumption of lowfat diet, increase in fruits and vegetables intake, and more physical activity [31,34]. Our short term intervention program (12 weeks) was successful in reducing body fatness and improving fitness and eating behavior of school children. Some of studies we reviewed had a length of intervention ranging from four weeks to three years [21,23,26,32], yet evidences suggest that a short intervention period might be associated with better outcomes [21,23,35].
The prevalence of overweight and obesity in our study were higher in boys than in girls. After the intervention the prevalence of obesity decreased 3.8% in boys and 3.0% in girls. Small shifts in BMI may be more effective at a population level than simply reducing the prevalence of obesity [36].
Inadequate eating behavior and sedentary lifestyle predispose to childhood obesity. There are interactions of many factors that contribute to the obesogenic environments and affect children’s weight, such as individual factors, home influences, and school factors. Afterschool intervention programs that promote an open-air physical activity along with healthy cooking class replaces a time that would be probably spent by children in front of the television or playing with computer and video games.
This study had several potential limitations: the children’s group was not separately to meet their age-appropriated developmental and gender issue; the intervenetion were applied to a small number of children and thus may not be representative; lack of control group.
Despite of these limitations, out data shows successfully the efficacy of a multidisciplinary school intervenetion to reduce body fat and improve fitness and healthy eating behavior in children. The increased prevalence of childhood obesity is an indicator of public health problem. High-risk screening and effective health educational should be priority especially in developing countries.
5. Conclusion
Our study showed that a school-based intervention program focused on nutritional education and physical activity program promote waist circumference reduction, improve fitness and healthy eating behavior. This intervention program would be feasible and replicable in others schools around the country.
6. Acknowledgements
Pró Reitoria de Pesquisa da UNESP and FUNDUNESP, for providing funds for the publication fee.
REFERENCES
- C. L. Ogden, M. D. Carroll, L. R. Curtin, et al., “Prevalence of High Body Mass Index in US Children and Adolescents, 2007-2008,” The Journal of the American Medical Association, Vol. 303, No. 3, 2010, pp. 242-249. http://dx.doi.org/10.1001/jama.2009.2012
- N. Gupta, K. Goel, P. Shah, et al., “Childhood Obesity in Developing Countries: Epidemiology, Determinants, and Prevention,” Endocrine Reviews, Vol. 33, No. 1, 2012, pp. 48-70. http://dx.doi.org/10.1210/er.2010-0028
- IBGE, “Fundação Instituto Brasileiro de Geografia e Estatística. Estudo Nacional das Despesas Familiares; Dados Preliminares. Consumo; Antropometria,” IBGE, Região V. Rio de Janeiro, 1977.
- IBGE, “Fundação Instituto Brasileiro de Geografia e Estatística. Pesquisas de Orçamentos Familiares 2008-2009. Antropometria e Estado Nutricional de Crianças, Adolescentes e Adultos no Brasil,” Rio de Janeiro, 2010.
- M. K. Serdula, D. Ivery, R. J. Coates, et al., “Do Obese Children Become Obese Adults? A Review of the Literature,” Preventive Medicine, Vol. 22, No. 2, 1993, pp. 167- 177. http://dx.doi.org/10.1006/pmed.1993.1014
- R. C. Whitaker, J. A. Wright, M. S. Pepe, et al., “Predicting Obesity in Young Adulthood from Childhood and Parental Obesity,” The New England Journal of Medicine, Vol. 337, No. 13, 1997, pp. 869-873. http://dx.doi.org/10.1056/NEJM199709253371301
- D. S. Freedman, Z. Mei, S. R. Srinivasan, et al., “Cardiovascular Risk Factors and Excess Adiposity among Overweight Children and Adolescents: The Bogalusa Heart Study,” The Journal of Pediatrics, Vol. 150, No. 1, 2007, pp. 12-17.e2.
- A. E. Rinaldi, G. D. Pimentel, A. F. Pereira, et al., “Metabolic Syndrome in Overweight Children from the City of Botucatu—Sao Paulo State—Brazil: Agreement among Six Diagnostic Criteria,” Diabetology & Metabolic Syndrome, Vol. 2, No. 1, 2010, p. 39. http://dx.doi.org/10.1186/1758-5996-2-39
- A. P. Ferreira, C. E. Oliveira and N. M. Franca, “Metabolic Syndrome and Risk Factors for Cardiovascular Disease in Obese Children: The Relationship with Insulin Resistance (HOMA-IR),” Journal de Pediatria, Vol. 83, No. 1, 2007, pp. 21-26. http://dx.doi.org/10.2223/JPED.1562
- R. C. da Silva, W. L. Miranda, A. R. Chacra, et al., “Metabolic Syndrome and Insulin Resistance in Normal Glucose Tolerant Brazilian Adolescents with Family History of Type 2 Diabetes,” Diabetes Care, Vol. 28, No. 3, 2005, pp. 716-718. http://dx.doi.org/10.2337/diacare.28.3.716
- C. G. Buff, E. Ramos, F. I. S. Souza, et al., “Frequency of Metabolic Syndrome in Overweight and Obese Children and Adolescents,” The Revista Paulista de Pediatria, Vol. 25, No. 3, 2007, pp. 221-226. http://dx.doi.org/10.1590/S0103-05822007000300005
- M. S. F. Souza, R. B. Leme, R. R. Franco, et al., “Metabolic Syndrome and Obese and Overweight Adolescents,” The Revista Paulista de Pediatria, Vol. 25, No. 3, 2007, pp. 214-220. http://dx.doi.org/10.1590/S0103-05822007000300004
- F. M. Biro and M. Wien, “Childhood Obesity and Adult Morbidities,” The American Journal of Clinical Nutrition, Vol. 91, No. 5, 2010, pp. 1499S-1505S. http://dx.doi.org/10.3945/ajcn.2010.28701B
- V. Andreasi, E. Michelin, A. E. Rinaldi, et al., “Physical Fitness and Associations with Anthropometric Measurements in 7 to 15-Year-Old School Children,” Journal de Pediatria, Vol. 86, No. 6, 2010, pp. 497-502.
- J. C. Angelo, “Associação da Aptidão Física com Indicadores Socioeconômicos, Tempo de TV e Prática de Atividades Físicas de Escolares com Excesso de Peso,” Monografia de Conclusão de Curso de Aperfeiçoamento/ Especialização em Exercício Físico Nutrição e Medicina na Saúde e no Esporte, Universidade Estadual Paulista Júlio de Mesquita Filho, 2009.
- J. E. Donnelly, J. L. Greene, C. A. Gibson, et al., “Physical Activity across the Curriculum (PAAC): A Randomized Controlled Trial to Promote Physical Activity and Diminish Overweight and Obesity in Elementary School Children,” Preventive Medicine, Vol. 49, No. 4, 2009, pp. 336-341. http://dx.doi.org/10.1016/j.ypmed.2009.07.022
- B. Caballero, T. Clay, S. M. Davis, et al., “Pathways: A School-Based, Randomized Controlled Trial for the Prevention of Obesity in American Indian Schoolchildren,” The American Journal of Clinical Nutrition, Vol. 78, No. 5, 2003, pp. 1030-1038.
- R. Sichieri, A. Paula Trotte, R. A. de Souza, et al., “School Randomised Trial on Prevention of Excessive Weight Gain by Discouraging Students from Drinking Sodas,” Public Health Nutrition, Vol. 12, No. 2, 2009, pp. 197-202. http://dx.doi.org/10.1017/S1368980008002644
- P. D. Angelopoulos, H. J. Milionis, E. Grammatikaki, et al., “Changes in BMI and Blood Pressure after a School Based Intervention: The CHILDREN Study,” European Journal of Public Health, Vol. 19, No. 3, 2009, pp. 319- 325. http://dx.doi.org/10.1093/eurpub/ckp004
- G. D. Foster, S. Sherman, K. E. Borradaile, et al., “A Policy-Based School Intervention to Prevent Overweight and Obesity,” Pediatrics, Vol. 121, No. 4, 2008, pp. e794- e802. http://dx.doi.org/10.1542/peds.2007-1365
- O. Matvienko and I. Ahrabi-Fard, “The Effects of a 4- Week After-School Program on Motor Skills and Fitness of Kindergarten and First-Grade Students,” American Journal of Health Promotion, Vol. 24, No. 5, 2010, pp. 299- 303. http://dx.doi.org/10.4278/ajhp.08050146
- Z. Yin, B. Gutin, M. H. Johnson, et al., “An Environmental Approach to Obesity Prevention in Children: Medical College of Georgia FitKid Project Year 1 Results,” Obesity Research, Vol. 13, No. 12, 2005, pp. 2153-2161. http://dx.doi.org/10.1038/oby.2005.267
- M. J. Duncan, Y. Al-Nakeeb and A. M. Nevill, “Effects of a 6-Week Circuit Training Intervention on Body Esteem and Body Mass Index in British Primary School Children,” Body Image, Vol. 6, No. 3, 2009, pp. 216-220. http://dx.doi.org/10.1016/j.bodyim.2009.04.003
- C. Graf, B. Koch, B. Bjarnason-Wehrens, et al., “Who Benefits from Intervention in, as Opposed to Screening of, Overweight and Obese Children?” Cardiology in the Young, Vol. 16, No. 5, 2006, pp. 474-480. http://dx.doi.org/10.1017/S1047951106000667
- B. M. Melnyk, L. Small, D. Morrison-Beedy, et al., “The COPE Healthy Lifestyles TEEN Program: Feasibility, Preliminary Efficacy, & Lessons Learned from an after School Group Intervention with Overweight Adolescents,” Journal of Pediatric Health Care, Vol. 21, No. 5, 2007, pp. 315-322. http://dx.doi.org/10.1016/j.pedhc.2007.02.009
- R. Vandongen, D. A. Jenner, C. Thompson, et al., “A Controlled Evaluation of a Fitness and Nutrition Intervention Program on Cardiovascular Health in 10- to 12- Year-Old Children,” Preventive Medicine, Vol. 24, No. 1, 1995, pp. 9-22. http://dx.doi.org/10.1006/pmed.1995.1003
- H. V. Lavelle, D. F. Mackay and J. P. Pell, “Systematic Review and Meta-Analysis of School-Based Interventions to Reduce Body Mass Index,” Journal of Public Health, Vol. 34, No. 3, 2012, pp. 360-369. http://dx.doi.org/10.1093/pubmed/fdr116
- M. de Onis, A. W. Onyango, E. Borghi, et al., “Development of a WHO Growth Reference for School-Aged Children and Adolescents,” Bulletin of the World Health Organization, Vol. 85, No. 9, 2007, pp. 660-667. http://dx.doi.org/10.2471/BLT.07.043497
- H. D. McCarthy, K. V. Jarrett and H. F. Crawley, “The Development of Waist Circumference Percentiles in British Children Aged 5.0-16.9 y,” European Journal of Clinical Nutrition, Vol. 55, No. 10, 2001, pp. 902-907. http://dx.doi.org/10.1038/sj.ejcn.1601240
- A. Gaya, A. Lemos, A. Gaya, et al., “Projeto Esporte Brasil (Proesp-Br). Manual de Testes e Avaliação,” 2012.
- M. Frenn, S. Malin and N. K. Bansal, “Stage-Based Interventions for Low-Fat Diet with Middle School Students,” Journal of Pediatric Nursing, Vol. 18, No. 1, 2003, pp. 36-45. http://dx.doi.org/10.1053/jpdn.2003.6
- J. Jiang, X. Xia, T. Greiner, et al., “The Effects of a 3-Year Obesity Intervention in Schoolchildren in Beijing,” Child: Care, Health and Development, Vol. 33, No. 5, 2007, pp. 641-646. http://dx.doi.org/10.1111/j.1365-2214.2007.00738.x
- F. Salcedo Aguilar, V. Martinez-Vizcaino, M. Sanchez Lopez, et al., “Impact of an After-School Physical Activity Program on Obesity in Children,” Journal of Pediatrics, Vol. 157, No. 1, 2010, pp. 36-42.e3.
- T. K. Harrell, B. M. Davy, J. L. Stewart, et al., “Effectiveness of a School-Based Intervention to Increase Health Knowledge of Cardiovascular Disease Risk Factors among Rural Mississippi Middle School Children,” Southern Medical Journal, Vol. 98, No. 12, 2005, pp. 1173-1180. http://dx.doi.org/10.1097/01.smj.0000182499.59715.07
- C. K. Haddock, W. R. Shadish, R. C. Klesges, et al., “Treatments for Childhood and Adolescent Obesity,” Annals of Behavioral Medicine, Vol. 16, No. 3, 1994, pp. 235-244.
- G. Rose, “Sick Individuals and Sick Populations,” International Journal of Epidemiology, Vol. 14, No. 1, 1985, pp. 32-38. http://dx.doi.org/10.1093/ije/14.1.32

