Surgical Science
Vol.06 No.06(2015), Article ID:57181,7 pages
10.4236/ss.2015.66038
Totally Laparoscopic Total Gastrectomy with D2 Lymphadenectomy for Advanced Gastric Cancer
Hironobu Takano*, Yuma Ebihara, Yo Kurashima, Soichi Murakami, Toshiaki Shichinohe, Satoshi Hirano
Department of Gastroenterological Surgery II, Hokkaido University Graduate School of Medicine, Sapporo, Japan
Email: *htakano1231@yahoo.co.jp
Copyright © 2015 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 19 May 2015; accepted 13 June 2015; published 16 June 2015
ABSTRACT
Introductions: Gastrectomy, which is the standard surgical procedure for gastric cancer, has gradually come to be performed laparoscopically. Laparoscopic distal gastrectomy (LDG) has been adopted gradually and performed for advanced gastric cancer. However, laparoscopic total gastrectomy (LTG) has not been as widely accepted as LDG due to technical difficulties, especially with reconstruction and proper D2 lymphadenectomy. The purpose of the current study was to determine the utility of TLTG with concomitant splenectomy and D2 lymphadenectomy (TLTGS) for advanced gastric cancer (AGC). Materials and Methods: Between January 2006 and May 2014, 10 consecutive patients who underwent TLTGS for AGC and 76 patients who underwent TLTG with D1 lymphadenectomy were included in this study. These two groups were compared in terms of perioperative results, with assessment of intraoperative and postoperative outcomes. Results: There were no significant differences in patients’ characteristics between the two groups. Operative time was longer in the TLTGS group than in the TLTG group. However, the rate of patients with postoperative complications including major complications was not different between the groups, and no patient in the TLTGS group had anastomotic leakage or pancreatic fistula. Conclusions: In the short-term, TLTGS had good postoperative outcomes and was useful and acceptable for AGC.
Keywords:
Advanced Gastric Cancer, Totally Laparoscopic Total Gastrectomy, D2 Lymphadenectomy

1. Introduction
Gastric cancer is one of the most common malignancies worldwide [1] , and surgery offers the greatest chance of cure. Recently, gastrectomy, which is the standard surgical procedure for gastric cancer, has gradually come to be performed laparoscopically.
In 1994, the first report of laparoscopy-assisted distal gastrectomy (LDG) for early gastric cancer was published [2] . After that, many studies reported that LDG is not inferior to open gastrectomy in patients with early gastric cancer [3] [4] . Furthermore, with development of devices and surgical techniques, LDG has gradually gained popularity and been performed for advanced gastric cancer (AGC).
Although laparoscopic total gastrectomy (LTG) for gastric cancer was first reported in 1999 [5] , LTG has not been as widely accepted as LDG. The reasons for this are technical difficulties, especially with reconstruction and proper D2 lymphadenectomy. Recently, some reports have described surgical procedures for reconstruction during LTG. Some procedures for intracorporeal esophagojejunostomy in totally laparoscopic total gastrectomy (TLTG) have also been reported, and the outcomes of these procedures were acceptable [6] [7] . For D2 lymphadenectomy, most reports have used a laparoscopy-assisted procedure. There have been few reports of D2 lymphadenectomy in TLTG. One report showed that, in TLTG, more advanced gastric cancer was associated with higher postoperative morbidity [8] . Evaluation of the safety and feasibility of D2 lymphadenectomy during TLTG would lead to wide acceptance of TLTG for advanced gastric cancer.
We have performed TLTG with concomitant splenectomy and D2 lymphadenectomy (TLTGS) for AGC in 10 patients since January 2006. To the best of our knowledge, there have been few reports about TLTGS. Therefore, in this study, the outcome of TLTGS for AGC was retrospectively investigated to clarify its utility.
2. Materials and Methods
2.1. Patients
Between January 2006 and May 2014, 10 consecutive patients underwent TLTGS for AGC and 76 patients underwent TLTG with D1 lymphadenectomy at Hokkaido University Hospital which is high volume center had about 10,000 admissions per year and were included in this study. The eligibility criterion for TLTG with D1 lymphadenectomy was clinical stage IA or IB gastric cancer that was preoperatively diagnosed by endoscopy, computed tomography, and endoscopic ultrasound according to the Japanese Classification of Gastric Carcinoma established by the Japanese Research Society for Gastric Cancer [9] . D2 lymphadenectomy was performed for patients with over clinical stage IIA gastric cancer. All patients were subjected to two groups according to these criteria. Two of the ten patients with TLTGS underwent neoadjuvant chemotherapy. All patients provided their written, informed consent prior to surgery. This study was approved by the institutional Ethics Committee of Hokkaido University Hospital. Specimens were also evaluated according to the Japanese Classification of Gastric Carcinoma established by the Japanese Research Society for Gastric Cancer.
2.2. Surgical Procedure
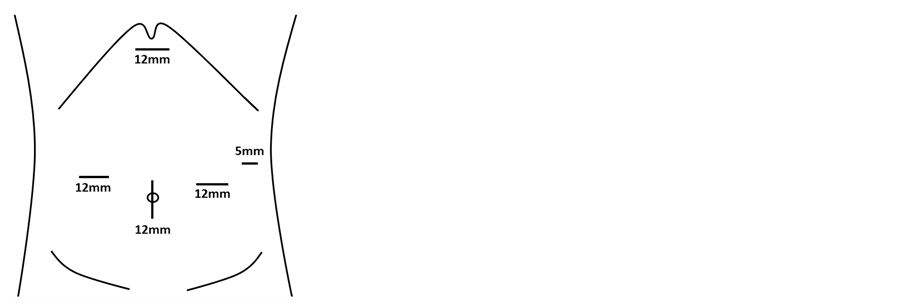
Each patient was placed in the supine reverse Trendelenburg position with legs apart, under general anesthesia. Five trocars (Exel; Echicon Endo-Surgery, Cincinnati, OH, USA) were used, and a 12-mm paraumbilical port was subsequently extended to 3.0 cm when pulling out the specimen. After carbon dioxide pneumoperitoneum was achieved at a pressure of 10 mmHg, an electrolaparoscope (WA50013, Olympus Medical Systems, Tokyo, Japan) was introduced through this port, and four other trocars (three 12-mm and one 5-mm ports) were placed as shown in Figure 1. Laparoscopic coagulation shears (SONOSURG-X; Olympus Medical Systems or Harmonic Ace; Echicon Endo-Surgery) were used for lymph node dissection and coagulating vessels. The basic extent of lymph node dissection was D1, but in patients with clinical N1, it was D2 with splenectomy, and both were performed with TLTG.
Intracorporeal reconstruction was done by a functional end-to-end esophagojejunostomy in all patients. The detailed procedure was reported previously [7] .
2.3. Clinicopathological Findings
Information about the patients, including sex, age, body mass index (BMI), and perioperative data, including
Figure 1. Positions of the surgical ports. Four 12-mm trocars are placed in the paraumbilical, bilateral abdominal, and epigastric regions. One 5-mm trocar is placed in the left hypochondrial area.
operation time, blood loss, number of lymph nodes dissected, pathological findings, and perioperative complications, was retrospectively collected from the medical and anesthesia records. Complications were classified according to the revised version of the Clavien-Dindo classification suggested by Dindo et al. [10] .
2.4. Statistical Analysis
Quantitative data are expressed as medians and ranges. The differences in the data between groups were compared using the χ2 test, Fisher’s exact probability test, or the Mann-Whitney U test. P < 0.05 was considered significant. All analyses were performed using JMP® 10 software.
3. Results
Table 1 shows the patients’ characteristic and pathologic features of the two groups (TLTGS (D2) group and TLTG (D1) group). There were 6 male and 4 female patients in the TLTGS group, and 53 male and 23 female patients in the TLTG group. The median age of these groups was 64 years (range, 40 - 74 years) and 66 years (range, 30 - 88 years), respectively. The median body mass index (BMI) was 21.0 kg/m2 (range, 16.0 - 34.2 kg/m2) in the TLTGS group and 23.0 kg/m2 (range, 15.2 - 34.6 kg/m2) in the TLTG group. There were no significant differences between the two groups in sex, age, and BMI. The ASA classification of the patients and the tumor locations of the patients were not significantly different between the two groups. The median number of dissected lymph nodes was 53 (range, 23 - 97) in the TLTGS group and 29 (range, 3-81) in the TLTG group; it was significantly larger in the TLTGS group than in the TLTG group (P = 0.019). The rate of patients with lymph node metastases was also significantly larger in the TLTGS group than in the TLTG group (P = 0.011). For the histological type of cancer, there was a tendency for a lower degree of differentiation in the TLTGS group. For pathological stage, more than half of the patients in the TLTG group were diagnosed with stage IA or IB, but few patients were diagnosed with stage IA or IB, and almost all patients were diagnosed with over stage IIA in the TLTGS group. The patients in the TLTGS group had significantly more advanced disease than those in the TLTG group.
The patients’ perioperative data are shown in Table 2. The median operation time was 393 min (range, 294 - 762 min) in the TLTGS group and 258 min (range, 137 - 430 min) in the TLTG group (P < 0.001). However, there was no significant difference in blood loss between the two groups, which was 100 mL (range, 0 - 370 mL) in the TLTGS group and 50 mL (range, 0 - 909 mL) in the TLTG group. For the postoperative course, there was no significant difference in the time to first flatus between the two groups, but the time to first soft diet was significantly shorter in the TLTGS group than in the TLTG group (P = 0.008). There were 2 patients (20%) in the TLTGS group and 13 patients (17.1%) in the TLTG group with postoperative complications. There was no significant difference in the rate of complications between the two groups. Major complications (≥IIIa of the Clavien-Dindo classification) were seen in 1 patient (10%) in the TLTGS group and 7 patients (9.2%) in the TLTG group. The details of complications are listed in Table 2. There were no patients with anastomotic leakage and
Table 1. Patients’ characteristics and pathologic features (n = 86).
BMI body mass index. aNumbers show medians, and numbers in parentheses show the 95% confidence interval of each parameter.
pancreatic fistula in the TLTGS group. One patient in the TLTGS group needed reoperation for omental necrosis. Two patients in the TLTG group needed reoperation. One patient underwent reoperation for jejunojejunostomy leakage, and the other patient who underwent reoperation for afferent loop syndrome caused by internal hernia died of septic shock on postoperative day 90. One patient in the TLTG group was converted to open surgery due to low blood pressure of uncertain cause during the procedure. The median postoperative hospital stay in the TLTGS group was 17.5 days (range, 10 - 29 days) and that in the TLTG group was 16 days (range, 8 - 90 days). There was no significant difference in postoperative hospital stay between the two groups. In the TLTGS group, 8 of the 10 patients underwent adjuvant chemotherapy, and all patients were alive and have no recurrence at the
Table 2. Perioperative data (n = 86).
aNumbers show medians, and numbers in parentheses show the 95% confidence interval of each parameter.
time of writing. The median follow-up time from operation was 26.9 months.
4. Discussion
Gastrectomy is the standard therapy for gastric cancer, and laparoscopic surgery has seen rapid development recently. Laparoscopic surgery confers upon patients the advantages of faster recovery, less hemorrhage, and smaller incisions that reduce postoperative pain, the probability of intestinal obstruction, and the risk of wound infection. However, the safety and the results, including short-term and long-term outcomes, are the issues with the procedure. After its introduction in 1994, LDG for early gastric cancer has been widely accepted [11] [12] . Some reports have indicated the LDG for advanced gastric cancer is acceptable, with a favorable outcome for D2 lymphadenectomy during LDG [13] [14] . Totally laparoscopic distal gastrectomy (TLDG) has also been accepted with the development of the new technique of intracorporeal anastomosis [15] and various devices. We adopted the policy of totally laparoscopic gastrectomy (TLG) from the initial period at our hospital, and we have not experienced conversion to open surgery as a result of intracorporeal anastomosis. There may be several advantages associated with TLG. In laparoscopy-assisted gastrectomy, extracorporeal anastomosis via a mini-la- parotomy incision may cause strong tension and injuries to the structures around the anastomosis because of limited vision, particularly in obese patients. In TLG, the whole anastomotic procedure can be clearly viewed, thereby eliminating such tension and injuries.
However, LTG for the treatment of advanced gastric cancer has remained controversial. The reasons for this are technical difficulties with reconstruction and proper lymphadenectomy, including D2 lymphadenectomy. Intracorporeal reconstruction was performed mainly by the functional end-to-end method or the overlap method. These methods during LTG were reported previously and showed a good outcome [16] . We adopted functional end-to-end anastomosis with a linear stapler for intracorporeal esophagojejunostomy for all patients with TLTG including D1 and D2 lymphadenectomy. One patient (1%) developed esophagojejunostomy leakage. The patient did not need drainage or re-operation and was cured by conservative therapy alone. Esophagojejunostomy stenosis developed in 3 patients (3%). These patients resolved with endoscopic dilation. There was one case of internal hernia with TLTG, and the mesenteric defects were closed using an intracorporeal suture for all patients after that. We consider that functional end-to-end anastomosis for esophagojejunostomy is a safe and feasible technique during TLTG.
LTG with D1 lymphadenectomy for early gastric cancer has been reported to be an acceptable procedure [17] . In these reports, postoperative morbidity after LTG was 18.1% - 26.9%. However, Jeong et al. noted that D2 lymphadenectomy was an independent risk factor for postoperative complications after LTG [18] . The rate of morbidity after LTG with D2 was 52.6%, and that of LTG with D1 was 18.2% in their study. Tsunoda et al. mentioned that more advanced disease was associated with higher postoperative morbidity [8] . The morbidity of LTG with D2 was 34.5%, and that of LTG with D1 was 18.1% in their report. In the present study, the rate of postoperative complications for TLTG with D2 was 20%, compared with 17.1% for TLTG with D1. There were no significant differences in morbidity between the two groups. The patient morbidity of TLTG with D2 was considered acceptable compared with previous reports.
Combined splenectomy for advanced gastric cancer has been controversial. Some reports stated that the survival of patients who underwent gastrectomy with splenectomy and extended lymph node dissection was longer than that of patients with gastrectomy alone [19] . There were also cases with metastatic nodes in the dissected area including the splenic hilus by extended lymph node dissection including splenectomy [20] [21] . However, other reports indicated that gastrectomy combined with splenectomy tended to be associated with higher morbidity and mortality and had no impact on survival [22] [23] . The common technical difficulty encountered during LTG with D2 lymphadenectomy was dissection of the suprapancreatic and splenic hilus lymph nodes. Shinohara et al. and Hur et al. reported that taping of the splenic artery was helpful in dissecting lymph nodes, including Nos. 10 and 11d [24] [25] . We performed TLTG combined with splenectomy for all patients with D2 lymphadenectomy, and we standardized the operative procedure. We performed the operation in a co-axial setting; the surgeon stood between the patient’s legs and used bilateral abdominal ports, and the scopist used the paraumbilical port. Initial mobilization of the cranial end of the pancreatic body/tail and spleen and taping of the splenic artery for dissecting lymph nodes 11 d and 10 were performed. As a result, the rate of complications of patients with D2 lymphadenectomy was similar with that of D1 lymphadenectomy in the present study. The rate of major complications (≥IIIa of the Clavien-Dindo classification) in the TLTGS group was also similar to that in the TLTG group. TLTG combined with splenectomy and D2 lymphadenectomy did not have a higher morbidity rate.
The limitation of the present study is the retrospective study and that the long-term outcomes, overall survival and disease-free survival, are still unknown. More cases and longer follow-up for long-term survival are needed.
5. Conclusion
In conclusion, the short-term results of TLTGS with D2 lymphadenectomy for advanced gastric cancer were evaluated by comparing them with those of D1 lymphadenectomy for early gastric cancer. Although cases with higher stage were included in the TLTGS group, the safety of the procedure during TLTGS with D2 lymphadenectomy was not inferior to that of TLTG with D1 lymphadenectomy. TLTGS with D2 lymphadenectomy is a useful and acceptable procedure for advanced gastric cancer.
Acknowledgements
The authors have no conflicts of interest to disclose and receive no financial support for this study.
References
- Parkin, D.M., Bray, F., Ferlay, J. and Pisani, P. (2005) Global Cancer Statistics, 2002. CA: A Cancer Journal for Clinicians, 55, 74-108. http://dx.doi.org/10.3322/canjclin.55.2.74
- Kitano, S., Iso, Y., Moriyama, M. and Sugimachi, K. (1994) Laparoscopy-Assisted Billroth I Gastrectomy. Surgical Laparoscopy & Endoscopy, 4, 146-148.
- Huscher, C.G., Mingoli, A., Sgarzini, G., Sansonetti, A., Di Paola, M., Recher, A. and Ponzano, C. (2005) Laparoscopic versus Open Subtotal Gastrectomy for Distal Gastric Cancer: Five-Year Results of a Randomized Prospective Trial. Annals of Surgery, 241, 232-237. http://dx.doi.org/10.1097/01.sla.0000151892.35922.f2
- Lee, S.W., Nomura, E., Bouras, G., Tokuhara, T., Tsunemi, S. and Tanigawa, N. (2010) Long-Term Oncologic Outcomes from Laparoscopic Gastrectomy for Gastric Cancer: A Single-Center Experience of 601 Consecutive Resections. Journal of the American College of Surgeons, 211, 33-40. http://dx.doi.org/10.1016/j.jamcollsurg.2010.03.018
- Azagra, J.S., Goergen, M., De Simone, P. and Ibanez-Aguirre, J. (1999) Minimally Invasive Surgery for Gastric Cancer. Surgical Endoscopy, 13, 351-357. http://dx.doi.org/10.1007/s004649900988
- Okabe, H., Obama, K., Tanaka, E., Nomura, A., Kawamura, J., Nagayama, S., Itami, A., Watanabe, G., Kanaya, S. and Sakai, Y. (2009) Intracorporeal Esophagojejunal Anastomosis after Laparoscopic Total Gastrectomy for Patients with Gastric Cancer. Surgical Endoscopy, 23, 2167-2171. http://dx.doi.org/10.1007/s00464-008-9987-8
- Ebihara, Y., Okushiba, S., Kawarada, Y., Kitashiro, S. and Katoh, H. (2013) Outcome of Functional End-to-End Esophagojejunostomy in Totally Laparoscopic Total Gastrectomy. Langenbeck’s Archives of Surgery, 398, 475-479. http://dx.doi.org/10.1007/s00423-013-1051-z
- Tsunoda, S., Okabe, H., Obama, K., Tanaka, E., Hisamori, S., Kinjo, Y. and Sakai, Y. (2014) Short-Term Outcomes of Totally Laparoscopic Total Gastrectomy: Experience with the First Consecutive 112 Cases. World Journal of Surgery, 38, 2662-2667. http://dx.doi.org/10.1007/s00268-014-2611-2
- Japanese Gastric Cancer Association (1998) Japanese Classification of Gastric Carcinoma―2nd English Edition. Gastric Cancer, 1, 10-24. http://dx.doi.org/10.1007/PL00011681
- Dindo, D., Demartines, N. and Clavien, P.A. (2004) Classification of Surgical Complications: A New Proposal with Evaluation in a Cohort of 6336 Patients and Results of a Survey. Annals of Surgery, 240, 205-213. http://dx.doi.org/10.1097/01.sla.0000133083.54934.ae
- Adachi, Y., Shiraishi, N., Shiromizu, A., Bandoh, T., Aramaki, M. and Kitano, S. (2000) Laparoscopy-Assisted Billroth I Gastrectomy Compared with Conventional Open Gastrectomy. Archives of Surgery, 135, 806-810. http://dx.doi.org/10.1001/archsurg.135.7.806
- Kim, M.C., Kim, K.H., Kim, H.H. and Jung, G.J. (2005) Comparison of Laparoscopy-Assisted by Conventional Open Distal Gastrectomy and Extraperigastric Lymph Node Dissection in Early Gastric Cancer. Journal of Surgical Oncology, 91, 90-94. http://dx.doi.org/10.1002/jso.20271
- Zhao, X.F., Jeong, O., Jung, M.R., Ryu, S.Y. and Park, Y.K. (2013) A Propensity Score-Matched Case-Control Com- parative Study of Laparoscopic and Open Extended (D2) Lymph Node Dissection for Distal Gastric Carcinoma. Surgical Endoscopy, 27, 2792-2800. http://dx.doi.org/10.1007/s00464-013-2809-7
- Chen, K., Mou, Y.P., Xu, X.W., Cai, J.Q., Wu, D., Pan, Y. and Zhang, R.C. (2014) Short-Term Surgical and Long- Term Survival Outcomes after Laparoscopic Distal Gastrectomy with D2 Lymphadenectomy for Gastric Cancer. BMC Gastroenterology, 14, 41. http://dx.doi.org/10.1186/1471-230X-14-41
- Kanaya, S., Gomi, T., Momoi, H., Tamaki, N., Isobe, H., Katayama, T., Wada, Y. and Ohtoshi, M. (2002) Delta-Shaped Anastomosis in Totally Laparoscopic Billroth I Gastrectomy: New Technique of Intraabdominal Gastroduodenostomy. Journal of the American College of Surgeons, 195, 284-287. http://dx.doi.org/10.1016/S1072-7515(02)01239-5
- Tsujimoto, H., Uyama, I., Yaguchi, Y., Kumano, I., Takahata, R., Matsumoto, Y., Yoshida, K., Horiguchi, H., Aosasa, S., Ono, S., Yamamoto, J. and Hase, K. (2012) Outcome of Overlap Anastomosis Using a Linear Stapler after Laparoscopic Total and Proximal Gastrectomy. Langenbeck’s Archives of Surgery, 397, 833-840. http://dx.doi.org/10.1007/s00423-012-0939-3
- Jeong, G.A., Cho, G.S., Kim, H.H., Lee, H.J., Ryu, S.W. and Song, K.Y. (2009) Laparoscopy-Assisted Total Gastrectomy for Gastric Cancer: A Multicenter Retrospective Analysis. Surgery, 146, 469-474. http://dx.doi.org/10.1016/j.surg.2009.03.023
- Jeong, O., Ryu, S.Y., Zhao, X.F., Jung, M.R., Kim, K.Y. and Park, Y.K. (2012) Short-Term Surgical Outcomes and Operative Risks of Laparoscopic Total Gastrectomy (LTG) for Gastric Carcinoma: Experience at a Large-Volume Center. Surgical Endoscopy, 26, 3418-3425. http://dx.doi.org/10.1007/s00464-012-2356-7
- Sano, T., Yamamoto, S. and Sasako, M. (2002) Randomized Controlled Trial to Evaluate Splenectomy in Total Gastrectomy for Proximal Gastric Carcinoma: Japan Clinical Oncology Group Study JCOG 0110-MF. Japanese Journal of Clinical Oncology, 32, 363-364. http://dx.doi.org/10.1093/jjco/hyf085
- Monig, S.P., Collet, P.H., Baldus, S.E., Schmackpfeffer, K., Schroder, W., Thiele, J., Dienes, H.P. and Holscher, A.H. (2001) Splenectomy in Proximal Gastric Cancer: Frequency of Lymph Node Metastasis to the Splenic Hilus. Journal of Surgical Oncology, 76, 89-92. http://dx.doi.org/10.1002/1096-9098(200102)76:2<89::AID-JSO1016>3.0.CO;2-I
- Hulscher, J.B., Van Sandick, J.W., Offerhaus, G.J., Tilanus, H.W., Obertop, H. and Van Lanschot, J.J. (2001) Prospective Analysis of the Diagnostic Yield of Extended en Bloc Resection for Adenocarcinoma of the Oesophagus or Gastric Cardia. British Journal of Surgery, 88, 715-719. http://dx.doi.org/10.1046/j.1365-2168.2001.01746.x
- Csendes, A., Burdiles, P., Rojas, J., Braghetto, I., Diaz, J.C. and Maluenda, F. (2002) A Prospective Randomized Study Comparing D2 Total Gastrectomy versus D2 Total Gastrectomy plus Splenectomy in 187 Patients with Gastric Carcinoma. Surgery, 131, 401-407. http://dx.doi.org/10.1067/msy.2002.121891
- Yu, W., Choi, G.S. and Chung, H.Y. (2006) Randomized Clinical Trial of Splenectomy versus Splenic Preservation in Patients with Proximal Gastric Cancer. British Journal of Surgery, 93, 559-563. http://dx.doi.org/10.1002/bjs.5353
- Hur, H., Jeon, H.M. and Kim, W. (2008) Laparoscopic Pancreas- and Spleen-Preserving D2 Lymph Node Dissection in Advanced (cT2) Upper-Third Gastric Cancer. Journal of Surgical Oncology, 97, 169-172. http://dx.doi.org/10.1002/jso.20927
- Shinohara, T., Kanaya, S., Taniguchi, K., Fujita, T., Yanaga, K. and Uyama, I. (2009) Laparoscopic Total Gastrectomy with D2 Lymph Node Dissection for Gastric Cancer. Archives of Surgery, 144, 1138-1142. http://dx.doi.org/10.1001/archsurg.2009.223
NOTES
*Corresponding author.