Open Journal of Respiratory Diseases
Vol.3 No.4(2013), Article ID:39880,10 pages DOI:10.4236/ojrd.2013.34024
Developments in Simulation Bronchoscopy Training*
Department of Respiratory Medicine, Castle Hill Hospital, Hull and East Yorkshire Hospitals NHS Trust, Hull York Medical School, University of Hull, Hull, UK
Email: #jack.kastelik@hey.nhs.uk
Copyright © 2013 Jack A. Kastelik et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received August 6, 2013; revised September 6, 2013; accepted October 8, 2013
Keywords: Bronchoscopy; Simulation; Training
ABSTRACT
Flexible bronchoscopy is a common procedure. Training in bronchoscopy is a complex process involving learning technical skills, understanding indications and contraindications, risks and benefits of the procedure, working within the team and communicating with patients. It is expected that a competent bronchoscopist is able to maneuver the scope through the anatomically complex bronchial tree, take samples, manage the sedated patient and communicate with nursing staff. Learning the complex procedural skills in the clinical setting can be stressful, therefore current bronchoscopic training methodology should blend a number of learning methods including didactic lectures, web-based material, high and low fidelity simulators as well as supervised apprenticeship training. Simulation-based bronchoscopy training therefore has been explored as a mode of training bronchoscopy skills. In this article, the role of simulation-based bronchoscopy training is reviewed. The low fidelity and high fidelity virtual reality bronchoscopy models are described together with the evidence available to support the use of simulation for bronchoscopy training.
1. Introduction
The first minimally invasive visualization using flexible bronchoscopy was performed in 1965 and since then has gained wide use with over 500,000 procedures being performed in the USA annually [1,2]. It is performed under awake sedation and permits not only examination but also sampling of the upper airways and bronchial tree [3]. Flexible fibreoptic bronchoscopy has a multitude of glass fibres transporting light from the light source to the end of the scope positioned in the bronchus and then bringing the image back to the high definition screen. Additionally, it has suctioning and instrumentation channels for obtaining samples. The bronchoscopist is supported by endoscopy nursing staff trained in the preparation and working of the equipment, handling samples obtained during the procedure and managing sedated patients. It is expected that a competent bronchoscopist is able to manoeuvre the scope through the anatomically complex bronchial tree, take samples, manage the sedated patient and communicate with nursing staff [4]. Training in bronchoscopy is a complex process involving learning technical skills, understanding indications and contraindications, risks and benefits of the procedure, working within the team and communicating with patients [2]. Traditionally, acquiring the ability of conducting this procedure is based on the apprenticeship model that requires the trainee to have the acumen to acquire the skill and the trainer to effectively teach it [3]. Learning the complex procedural skills in the clinical setting can be stressful [5]. Therefore, current bronchoscopic training methodology should blend a number of learning methods including didactic lectures, web-based material, high and low fidelity simulators as well as supervised apprenticeship training. More recently, educational technology including simulation-based bronchoscopy training has become available and is gradually being integrated into respiratory medicine curriculum.
2. Training in Bronchoscopy Skills
Core curriculum training in many institutions includes a series of lectures and modular approach including a variety of technological media describing the procedure, its indications, complications and consenting [6-9]. For example, trainees may watch a video of a procedure or use a web-based e-learning module such as that available at British Thoracic Society (www.brit-thoracic.org.uk) or Essential Bronchoscopist (www.bronchoscopy.org) web sites [10-12]. Evidence suggests that instructional videotaped, web-based educational material or even simple question and answer exercises can improve visual perception and discrimination skills of the learner, and provide cognitive skills essential for performing the procedure most likely through acquisition of anatomical knowledge, recognition of pathological abnormalities, technical information such as consenting, or knowledge of sedation and use of local anesthesia [4,11,13]. Although there is some evidence contrary to this [12]. These conflicting results may be explained by variations in e-learning programs, use of inappropriate assessment tools, or trainees’ lack of time and motivation of receiving the educational material due to clinical work pressure [12]. Despite the shortfalls there is suggestion that in order to achieve these challenges training e-learning modules, didactic lectures or video material are essential tools that may be combined with other modes of learning using educational technological developments such as simulation [14-16].
3. Simulation-Based Education
The concept of simulation was initially introduced in the airline industry as a cost-effective measure and reduces potential errors that may have catastrophic consequences [9]. Simulation permits trainees to acquire theoretical and technical skills through an interactive occasionally immersive educational activity through recreation of clinical experience without exposing patients to the associated risks [17-19]. However, in order to provide most effective simulation training learners require to interact with the simulator and simulation environment as if they were real [20]. It can help trainees develop muscle memory and hand-eye co-ordination [12]. A proportion of higher medical trainers may have chosen a career in respiratory medicine in the hope of performing bronchoscopies [5]. Traditional bronchoscopic training is based on a master-apprentice model utilizing Halstedt’s approach based on “see one, do one, teach one” principle, with trainees initially performing procedures on low-risk patients under close supervision and gradually progressing to more complex cases and independence [21,22]. However, this training model has its limitations. For example, from an educational perspective there is recognized variation in bronchoscopy training with reports suggesting that a fifth of the trainees not achieving the required number of procedures and skill [23-25]. Moreover, the clinical setting may not be the ideal learning environment for novices to acquire bronchoscopic skills, and may be associated with anxiety, variable experience and patient safety issues [5,26]. Hence, simulation has increasingly been used as an alternative mechanism of attaining bronchoscopy skills.
There is an ever increasing evidence base for the role of high fidelity virtual reality simulation bronchoscopy as a useful tool for novice trainees to acquire skills prior to performing the procedure on patients [6]. Moreover simulation may standardize assessing bronchoscopy competence, which currently is based on the record of number of procedures performed, subjective educational supervisors report and the outcomes of work-based assessments; the direct observation of procedural skills (DOPS), which grade competency based on multiple stages varying from performing the procedure under close supervision to being independent [11]. Simulation training within the confines of a controlled environment of the skills laboratory provides a safe training environment of practical procedures, enhances professional and learning experience, protects patients’ safety by reducing exposure to trainees’ deficiencies as well as protecting trainees from deficient training environment. Simulation bronchoscopy training may be delivered either as low fidelity and high fidelity simulation depending on the types of technology used. Low fidelity simulation relies on the use of inanimate models of upper airways and bronchial tree whereas high fidelity simulation uses specifically designed equipment based on computerized modules [27].
4. Low Fidelity Bronchoscopy Simulation
Initial reports described the use of animal models to acquire basic instrument handling to develop psychomotor bronchoscopic skills including lavage, biopsy and the removal of various foreign bodies [16,28]. However, it is well recognized that the use of animal models has its limitations due to ethical considerations as well as potential anatomical differences. As a result workshops using inanimate models have been introduced and have subsequently reported improved aspects of certain bronchoscopic psychomotor skills such as nasotracheal intubation; however only 35% of participants had an improvement in their performance [14]. This may be attributed to differences in the speed of skill acquisition and styles of learning. Interestingly, trainees who practiced using low fidelity inanimate models were more successful initially with bronchoscopy intubation skills compared with those learning using traditional approach [29]. This is most likely related to the improvement of the initial learning curve for bronchoscopy skills that may occur in the early stages of leaning this procedure as a result of simulation training [12]. Occasionally, hybrid low fidelity models combining inanimate airway models have been used though the data on this hybrid training is limited [30]. The use of inanimate models for simulated bronchoscopy training has its limitations such as the artificial appearances and the lack of adaptation and application for specific pathology [10,28]. A major pitfall of low fidelity bronchoscopy simulation is its lack of realism compared to the actual procedure. The reality aspect in the learning environment can be improved through incorporation of low fidelity inanimate models with a real bronchoscope [31]. Despite these limitations perceptions from learners and trainers however suggest that both low and high fidelity bronchoscopy simulation provide equally enjoyable learning experiences [31]. Interestingly, learners report that some aspects of low fidelity bronchoscopy compared to high fidelity models provide a more realistic experience as the former involves the use of a real bronchoscope rather than a proxy instrument that is incorporated within the high fidelity model. However, the perception of trainers was that high fidelity simulators provide a more enjoyable learning experience due to the “halo” effect related to the pre-conception of the novelty of a higher degree of technological sophistication [31]. Moreover, high fidelity virtual reality models can make the educational experience more realistic through their ability to simulate aspects of bronchoscopy procedures such as such as cough, breathing, display of vital signs or bleeding. Importantly, low fidelity simulators are less costly, reusable and can incorporate a real bronchoscope. Considering the pros and cons of low and high fidelity simulators it may suggest that the former may be more suited to task-based teaching with and the latter virtual reality models providing high degree of realism with modular functions that may better suit more complex tasks [9].
5. Virtual Reality Bronchoscopy Simulators
Virtual reality incorporates a combination of human and computer interfaces, which may include the use of graphics, sensor technology, computing, or networking to allow the trainee to become immersed in and interact with the artificial environment [32,33]. Virtual reality simulation (VRS) can be used as a didactic means of delivering different training requirements incorporating a range of fidelity, teaching and assessment modes. Technological advances in computer technology, graphics, processor speed have permitted the development of bronchoscopy VRS [34]. Other specialties such as surgery and gastroenterology have been using VRS for training in procedures such as sigmoidoscopy, colonoscopy, gastroscopy and laparoscopic surgery [9,35,36]. In comparison there is limited evidence on the use of high fidelity simulation for bronchoscopy training. Due to the costs of the development and their production, only a small number of commercial bronchoscopy VRS are available (Table 1). An example of a complex training system is the Dexter™ (Replicant, Wellington, New Zealand), which is a modular, non-anatomical endoscopic dexterity training system, composed of a series of channels and images [37,38]. Although not a true VRS model, this system has been shown to improve dexterity-related psychomotor skills essential for bronchoscopy. True VRS models include AccuTouch® (HT Medical and Immersion Corporation, Gaithersburg, USA), the BRONCH Mentor™ (Simbionix, Cleveland, Ohio, USA) and EndoVR CAE Healthcare, Sarasota, FL, USA) with average cost of over $100,000 each, and a more cheaper (around $25,000) computer-based bronchoscopy simulator developed by Chen and colleagues [39] (Table 1). These high fidelity VRS are composed of a proxy bronchoscope modeled on a conventional scope, which may be inserted to the manikin nasal passages robotic interface that tracks the motion of proxy scope and simulation software within a personal computer and screen that generates the VRS images of the airways and bronchial tree [33,40]. Once the scope is inserted the computerized program allows for realistic vocal cords, trachea and bronchial tree imaging as the trainee navigates the scope, records actions of the user including duration of the procedure, number of bronchial segments entered, collisions with the bronchial wall and amount of medication used [33,39]. Furthermore, these simulators incorporate a realistic simulation environment of virtual patients modeled on real cases with realistic responses including vital signs and potential complications such as hypoxia and hypotension, as well as simulation of awake sedation, topical anaesthesia, anatomy atlas, 3-D orientation, performance metrics, retrospective evaluation of performance and tutorials. Within this complex data set and experience trainees gain new skills, knowledge in the safe environment of clinical skills laboratory including experience of maneuvering of the bronchoscope, learning bronchial anatomy using up-to-date graphic technology and physiological responses, and the psychomotor skills necessary to become competent in performing fiberoptic bronchoscopy which optimizes the learning curve of the trainee [33,40]. Hence, VRS bronchoscopy allows for bronchoscopic skill acquisition maintenance and assessment, subsequent skill development, potential cost reduction, increased competency with potential improvement in patient safety. VRS bronchoscopy can be programmed for a number of additional features such as variations in anatomy, degree of difficulty and physiological responses thus allowing the trainee to assess response to their actions. Moreover, VRS provides, built in feedback permitting independent learning, realistic graphics for enhanced learning as well as independent learning together with quantitative assessment using objective data for skills monitoring.
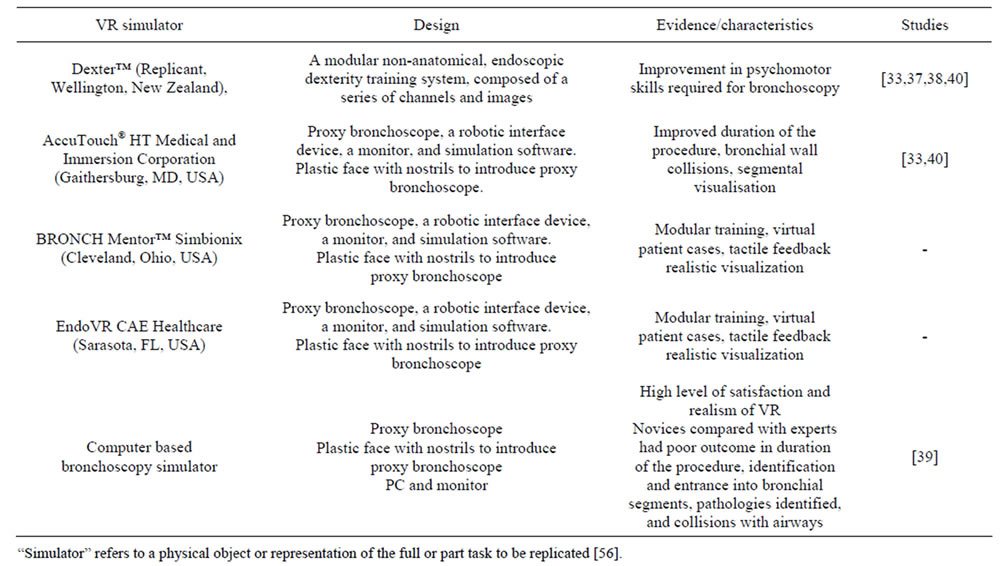
Table 1. Examples of virtual reality bronchoscopy simulators.
6. VRS Bronchoscopy Studies
Bronchoscopy training is an area of respiratory medicine where an argument for VRS may be compelling. Whilst technical aspects of performing bronchoscopy are important, the application of skills in the clinical context, and learner-centered and patient-focused training are of equal relevance. Currently, in the literature there are 12 studies that have used VRS bronchoscopy (Table 2). Five of these were randomized clinical trials [10,38-41] and of those only two assessed intubation using simulation bronchoscopy [38,40]. Of the three studies that assessed the full bronchoscopy procedure, two included one session on a simulator [39,41] and the third 20 bronchoscopies on a simulator in three to four sessions [10]. A recent systematic review and meta-analysis of simulation based bronchoscopy training incorporated additional studies [42]. These studies included animal models, manikins, designed artificial models or VRS bronchoscopy and endobronchial ultrasound training [26,43-49]. These studies used various differing models and demonstrated benefits from using simulation for purpose of bronchoscopy training. Moreover the systematic review and metaanalysis concluded that simulation based bronchoscopy as based on the limited available studies was effective when compared with no intervention [42].
The outcomes measured in the studies on simulation bronchoscopy training depended on the design, duration and the subjects participating in the study as well as the technology used. The studies using VRS bronchoscopy assessed outcomes such as duration of the procedure, identification of the bronchial segments and collisions with the bronchial wall. These relatively objective parameters can be incorporated within the software technology of the high fidelity simulators. The limitations of using these parameters are related to the fact that they mainly assess technical skills. As the repetitive practice on the simulator should increase muscle memory and hand-eye co-ordination, the studies confirmed that simulation training improved these outcomes for novices and trainees of different level bronchoscopy skills [10,31,41, 50]. The improvement in these outcomes was seen with both one off session on a simulator as well as repeated training over time [10,12,33,51]. Although at initial sessions the novices’ performance was inferior to that of experienced bronchoscopists, after a short period of training novices compared with experienced operators were able to perform more thorough examinations and missed significantly fewer segments in both the inanimate and VRS models [51]. Moreover by assessing these outcomes investigators were able to distinguish between the level of bronchoscopy experience [10]. Other shortfalls of these randomized controlled studies were the small subject number, variation in study designs and use of different VRS. The size limitation relates to the fact that each training program recruits a small number of new trainees each year, which is partially compensated by studying bronchoscopists at different levels of expertise or by
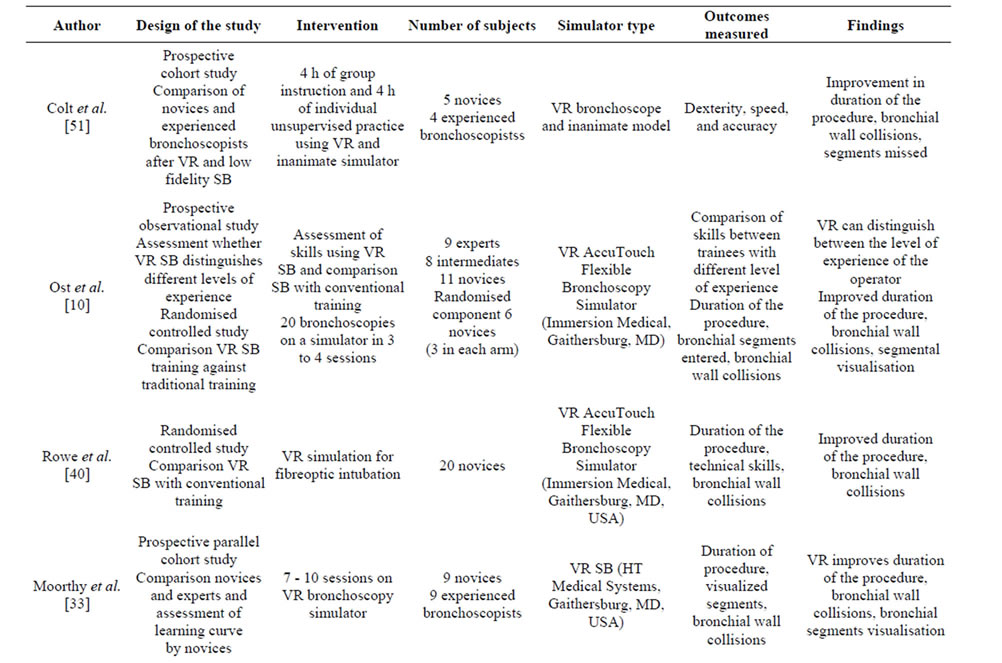
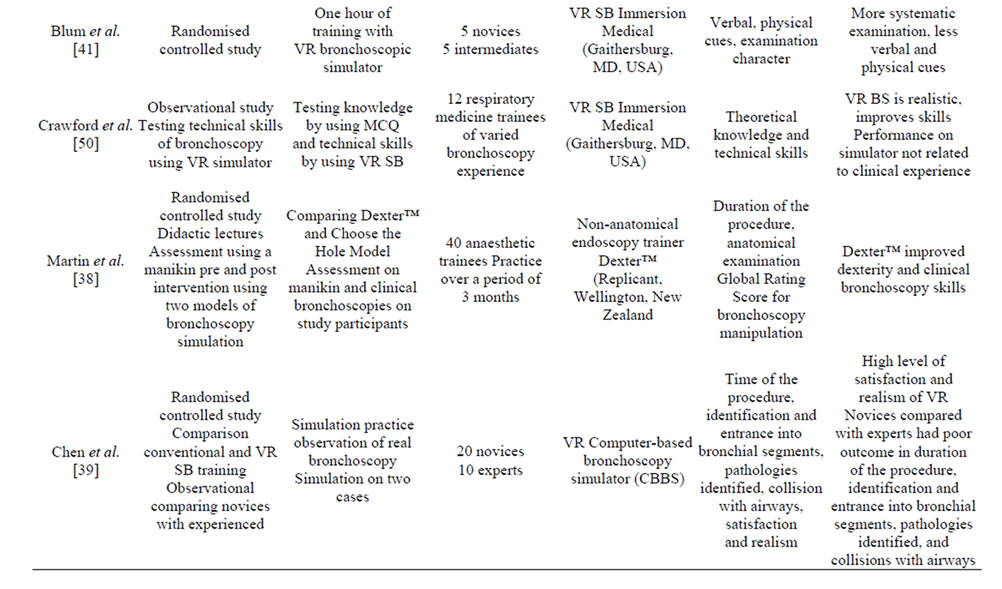
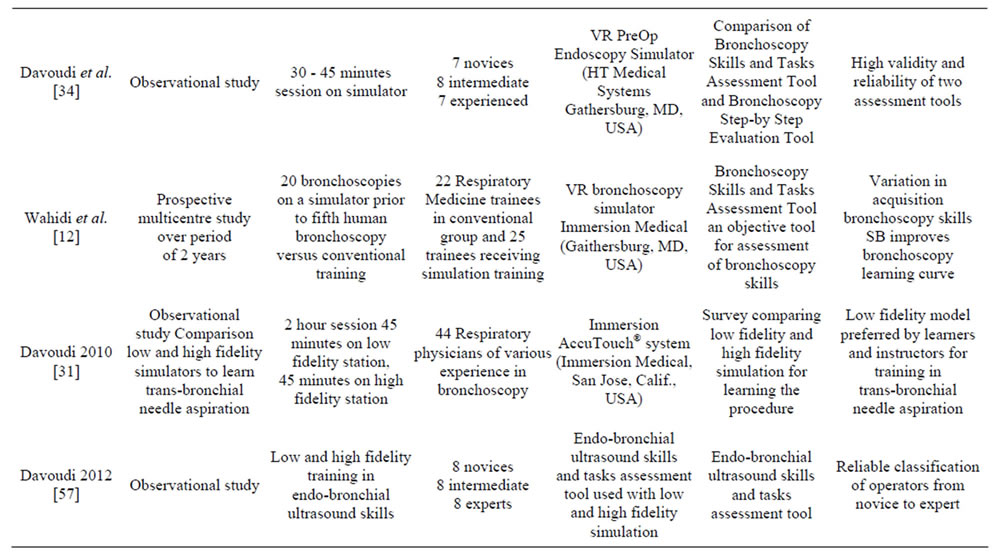
Table 2. Studies using virtual reality (VR) simulation bronchoscopy (SB).
performing multicenter studies [12,31]. Furthermore, the studies used different designs either comparing trainees’ performance before and after a period on a simulator or against experienced operators, thus introducing bias related to different speeds of learning the procedure, preference of learning styles, experts’ perception of reality of the simulators and the difference in handling the proxy instruments on VRS with that of a real bronchoscope. Despite these limitations the studies have produced some common theme results.
7. Training Novices and the Learning Curve
There is good evidence to suggest that novice trainees can gain basic skills of bronchoscopy through simulation training [10,12,41]. VRS bronchoscopy can improve cognitive and technical skills [51]. Additionally, novice trainees who practiced on a bronchoscopy simulator when compared with those trained using conventional methods performed better with regards to procedure time, nurse observer perception and percentage of identified bronchial anatomy [10]. Studies using VRS bronchoscopy were able to assess the learning curve for skill acquisition of this procedure. Smith and colleagues have reported that during naso-tracheal intubation training using endoscopic video camera system and a bronchial tree model, the half-time learning curve was 9 procedures with time reduction between the first and the eighteenth procedure from 132 to 49 seconds [52]. Following simulation training the novices exhibited similar level of skill as trainees who had performed ten naso-tracheal intubation bronchoscopy procedures on real patients [40]. Similarly, novices improved their skills after performing 20 bronchoscopies on a simulator in terms of speed, percentage of segments visualized, and collisions [10]. Others observed that 1 hour of practice on VRS bronchoscopy effectively trained novices’ basic bronchoscopy skills and anatomy [41]. In fact, there was no difference when novices’ skills were assessed on a real patient against trainees with 2 - 3 years experience in bronchoscopy [41]. When testing on a simulator there is a significant improvement in the performance in the novices between first and sixth sessions as percentage of visualized segments, time taken for the procedure and number of collisions with the bronchial wall [33].
It is well recognized that trainees acquire bronchoscopy skills at different rate although 50 procedures may be enough to achieve competency and majority will be deemed competent by the time they perform 100 procedures [5,25]. To achieve mastery of a procedure repeated practice is necessary and there is variation in time required to develop psychomotor skills for performing bronchoscopy between individuals [12]. Moreover, there is a rapid learning curve during the first 30 bronchoscopies and this slows down when performing 30 - 100 procedures but the peak of learning persists beyond first 50 procedures. This is in contrast to previous findings that suggested that competency of bronchoscopy can be achieved by performing 50 bronchoscopies [25]. The use of bronchoscopy simulation can speed up the initial learning curve and mastering of bronchoscopy skills which is dependent on hand-eye coordination [12]. There is good evidence that learning bronchoscopic procedural skills in a clinical skills laboratory using simulation technology can be successfully transferred to patient care [41]. Also, manikin simulation skill correlates with reallife bronchoscopy performance suggesting increased likelihood of transfer of endoscopic skills from bench to clinical procedure [38].
Simulation allows for a minimally-invasive procedure such as bronchoscopy to be conducted in a controlled environment using a simulator with no risk to the patient [34]. Moreover training can be tailored to individual trainees’ requirements with feedback being delivered in a timely fashion [53]. In contrast, bronchoscopy skill acquisition in clinical settings raises issues of patient safety, lack of consistency in delivery of standardized level of knowledge, skills and competency [7,18]. Thus training bronchoscopic skills in the clinical setting not only increases potential complications, but also procedure time by a third, besides the documentation and trainee assessments, which in turn culminates into financial inefficiencies [54]. Furthermore, the clinical environment is not conducive to the variation in acquisition of bronchoscopy skills [7,23]. Presently, the markers of competency include duration of training and number of procedures performed. Progressively, there has been a trend to move training from numerical competency to a more objective competency based on knowledge and technical skills assessment. Thus, the theoretical knowledge can be acquired through didactic lectures with simulation bronchoscopy providing opportunity for practical skills acquisition both of which are relevant to comprehension, application and analysis components of learning as well as functioning as a tool for objective competency assessment [33]. Bronchoscopy competency can be defined as the use of knowledge, technical skills to perform the procedure and clinical reasoning for making decisions regarding the procedure and findings for the benefit of individual patients [55]. Whilst acquiring bronchoscopy skills, trainees progress through the stages of novice, advanced beginner, competent provider, proficient provider and expert. VRS bronchoscopy is of relevance at the novice and advanced beginner stages during which trainees follow rigid rules with limited situation perception [12,33].
There is good evidence to suggest that simulation training can address many of the flaws related to the current apprenticeship model, therefore justifying its use in learning bronchoscopy skills. Despite encouraging evidence, incorporation of simulation bronchoscopy into training has been relatively measured. Possible explanations for this may be related to a number of factors such as educators’ preference for traditional methods of bronchoscopy training, costs of simulators, time involved in implementing a simulation bronchoscopy training program and perception of lack of good quality data to support simulation bronchoscopy. There is no denying that VRS bronchoscopy equipment is currently expensive and that simulation training requires time and expertise of a trained faculty [31]. The argument for poor quality data is true in the context of low fidelity simulation bronchoscopy as the current evidence is not sufficient to advocate its use beyond the basic skills training [14,29]. In contrast, there is quality evidence from randomized controlled studies for the use of VRS bronchoscopy being recommended; firstly, for acquisition of bronchoscopy skills with the aim to subsequently transfer of the simulation learned skills to the bedside and secondly, as a tool for development and assessment of competency [11,42]. Moreover, there is evidence that bronchoscopy skills acquired through simulation can be successfully transferred to patients’ care [12,38].
Current literature provides evidence that VRS bronchoscopy can address almost all of the twelve features of medical simulation described by McGaghie et al. [27]. There is good evidence that VRS bronchoscopy can address issues of fidelity, deliberate practice and some aspects of curriculum integration [42]. Besides VRS bronchoscopy can assess acquisition, mastering and maintenance of skills as the measured outcomes are objective and can differentiate between the novices and the experts [12,31]. Additionally, VRS bronchoscopy may have a role in competency assessment using validated tools such as Bronchoscopy Skills and Tasks Assessment (BSTAT) [12,50]. However, there is no evidence to support the use of VRS bronchoscopy for high stake testing such as specialty examinations or providing team learning. Although the latter could easily be addressed through incorporation within simulation of different groups of health workers normally involved with bronchoscopy, which would tackle issues of team composition, interactions and skill maintenance. Similarly, there is little data on the use of VRS bronchoscopy for instructor training, as clinical experience is not a proxy for VRS effectiveness, therefore highlighting need to establish mastery learning models for simulation instructors [27].
8. Conclusion
There is good evidence that VRS bronchoscopy improves technical skills of the procedure, speeds up initial learning curve and that skills acquired are transferrable to real life bronchoscopy. Therefore it can be recommended, based on evidence from randomized controlled studies that VRS should be used for training bronchoscopy prior to performing the procedure on patients as prior VRS bronchoscopy training results in decreased procedure time, bronchial wall contact, improved procedure efficacy and accuracy, and subsequent sustained improvement for procedures performed on patients. Whilst there are costs related to simulation training the benefits in the form of improved learning environment, standardized training and assessment, and patients’ safety greatly favour and grossly justify the use of VRS bronchoscopy.
REFERENCES
- A. Ernst, G. A. Silvestri and D. Johnstone, “Interventional Pulmonary Procedures: Guidelines from the American College of Chest Physicians,” Chest, Vol. 123, No. 5, 2003, pp. 1693-1717. http://dx.doi.org/10.1378/chest.123.5.1693
- G. A. Silvestri, D. Feller-Kopman, A. Chen, M. Wahidi, K. Yasufuku and A. Ernst, “Latest Advances in Advanced Diagnostic and Therapeutic Pulmonary Procedures,” Chest, Vol. 142, No. 6, 2012, pp. 1636-1644. http://dx.doi.org/10.1378/chest.12-2326
- P. A. Kvale and A. C. Mehta, “Training Bronchoscopists for the New Era,” Clinics in Chest Medicine, Vol. 22, No. 2, 2001, pp. 365-372. http://dx.doi.org/10.1016/S0272-5231(05)70050-2
- J. E. Rayl, J. M. Pittman and J. J. Shuster, “Preclinical Training in Bronchoscopic Diagnosis of Cancer,” Chest, Vol. 93, No. 4, 1988, pp. 824-827. http://dx.doi.org/10.1378/chest.93.4.824
- G. A. Silvestri, “The Evolution of Bronchoscopy Training,” Respiration; International Review of Thoracic Diseases, Vol. 76, No. 1, 2008, pp. 9-20.
- M. Davoudi and H. G. Colt, “Bronchoscopy Simulation: A Brief Review,” Advances in Health Sciences Education: Theory and Practice, Vol. 14, No. 2, 2009, pp. 287- 296. http://dx.doi.org/10.1007/s10459-007-9095-x
- E. F. Haponik, G. B. Russell, J. F. Beamis Jr., E. J. Britt, P. Kvale, P. Mathur and A. Mehta, “Bronchoscopy Training: Current Fellows’ Experiences and Some Concerns for the Future,” Chest, Vol. 118, No. 4, 2000, pp. 625- 630. http://dx.doi.org/10.1378/chest.118.3.625
- M. R. Lucarelli, C. R. Lucey and J. G. Mastronarde, “Survey of Current Practices in Fellowship Orientation,” Respiration, Vol. 74, No. 4, 2007, pp. 382-386.
- W. C. McGaghie, V. J. Siddall, P. E. Mazmanian and J. Myers, “Lessons for Continuing Medical Education from Simulation Research in Undergraduate and Graduate Medical Education: Effectiveness of Continuing Medical Education: American College of Chest Physicians Evidence-Based Educational Guidelines,” Chest, Vol. 135, No. 3, 2009, pp. 62S-68S. http://dx.doi.org/10.1378/chest.08-2521
- D. Ost, A. DeRosiers, E. J. Britt, A. M. Fein, M. L. Lesser and A. C. Mehta, “Assessment of a Bronchoscopy Simulator,” American Journal of Respiratory and Critical Care Medicine, Vol. 164, No. 5, 2001, pp. 2248-2255. http://dx.doi.org/10.1164/ajrccm.164.12.2102087
- M. Davoudi, S. Quadrelli, K. Osann and H. G. Colt, “A Competency-Based Test of Bronchoscopic Knowledge Using the Essential Bronchoscopist: An Initial Concept Study,” Respirology, Vol. 13, No. 5, 2008, pp. 736-743. http://dx.doi.org/10.1111/j.1440-1843.2008.01320.x
- M. M. Wahidi, G. A. Silvestri, R. D. Coakley, J. S. Ferguson, R. W. Shepherd, L. Moses, J. Conforti, L. G. Que, K. J. Anstrom, F. McGuire, H. Colt and G. H. Downie, “A Prospective Multicenter Study of Competency Metrics and Educational Interventions in the Learning of Bronchoscopy among New Pulmonary Fellows,” Chest, Vol. 137, No. 5, 2010, pp. 1040-1049. http://dx.doi.org/10.1378/chest.09-1234
- S. Quadrelli, M. Davoudi, F. Galindez and H. G. Colt, “Reliability of a 25-Item Low-Stakes Multiple-Choice Assessment of Bronchoscopic Knowledge,” Chest, Vol. 135, No. 2, 2009, pp. 315-321. http://dx.doi.org/10.1378/chest.08-0867
- M. H. Dykes and A. Ovassapian, “Dissemination of Fibreoptic Airway Endoscopy Skills by Means of a Workshop Utilizing Models,” British Journal of Anaesthesia, Vol. 63, No. 5, 1989, pp. 595-597. http://dx.doi.org/10.1093/bja/63.5.595
- A. Ovassapian, M. H. Dykes and M. E. Golmon, “A Training Programme for Fibreoptic Nasotracheal Intubation. Use of Model and Live Patients,” Anaesthesia, Vol. 38, No. 8, 1983, pp. 795-798. http://dx.doi.org/10.1111/j.1365-2044.1983.tb12207.x
- R. E. Wood and J. R. Pick, “Model Systems for Learning Pediatric Flexible Bronchoscopy,” Pediatric Pulmonology, Vol. 8, No. 3, 1990, pp. 168-171. http://dx.doi.org/10.1002/ppul.1950080307
- N. J. Maran and R. J. Glavin, “Lowto High-Fidelity Simulation—A Continuum of Medical Education?” Medical Education, Vol. 37, Suppl. 1, 2003, pp. 22-28. http://dx.doi.org/10.1046/j.1365-2923.37.s1.9.x
- I. Choy and A. Okrainec, “Simulation in Surgery: Perfecting the Practice,” The Surgical Clinics of North America, Vol. 90, No. 3, 2010, pp. 457-473. http://dx.doi.org/10.1016/j.suc.2010.02.011
- R. J. Scalese, V. T. Obeso and S. B. Issenberg, “Simulation Technology for Skills Training and Competency Assessment in Medical Education,” Journal of General Internal Medicine, Vol. 23, Suppl. 1, 2008, pp. 46-49. http://dx.doi.org/10.1007/s11606-007-0283-4
- R. H. Steadman, W. C. Coates, Y. M. Huang, R. Matevosian, B. R. Larmon, L. McCullough and D. Ariel, “Simulation-Based Training Is Superior to Problem-Based Learning for the Acquisition of Critical Assessment and Management Skills,” Critical Care Medicine, Vol. 34, No. 1, 2006, pp. 151-157. http://dx.doi.org/10.1097/01.CCM.0000190619.42013.94
- W. T. Mason and P. W. Strike, “See One, Do One, Teach One—Is This Still How It Works? A Comparison of the Medical and Nursing Professions in the Teaching of Practical Procedures,” Medical Teacher, Vol. 25, No. 6, 2003, pp. 664-666. http://dx.doi.org/10.1080/01421590310001605705
- J. M. Rodriguez-Paz, M. Kennedy, E. Salas, A. W. Wu, J. B. Sexton, E. A. Hunt and P. J. Pronovost, “Beyond ‘See One, Do One, Teach One’: Toward a Different Training Paradigm,” Quality and Safety in Health Care, Vol. 18, No. 1, 2009, pp. 63-68.
- N. J. Pastis, P. J. Nietert and G. A. Silvestri, “Variation in Training for Interventional Pulmonary Procedures among Us Pulmonary/Critical Care Fellowships: A Survey of Fellowship Directors,” Chest, Vol. 127, No. 5, 2005, pp. 1614-1621. http://dx.doi.org/10.1378/chest.127.5.1614
- D. R. Stather, J. Jarand, G. A. Silvestri and A. Tremblay, “An Evaluation of Procedural Training in Canadian Respirology Fellowship Programs: Program Directors’ and Fellows’ Perspectives,” Canadian Respiratory Journal: Journal of the Canadian Thoracic Society, Vo. 16, No. 2, 2009, pp. 55-59.
- K. G. Torrington, “Bronchoscopy Training and Competency: How Many Are Enough?” Chest, Vol. 118, No. 3, 2000, pp. 572-573. http://dx.doi.org/10.1378/chest.118.3.572
- H. G. Colt, M. Davoudi, S. Murgu and N. Zamanian Rohani, “Measuring Learning Gain during a One-Day Introductory Bronchoscopy Course,” Surgical Endoscopy, Vol. 25, No. 1, 2011, pp. 207-216. http://dx.doi.org/10.1007/s00464-010-1161-4
- W. C. McGaghie, S. B. Issenberg, E. R. Petrusa and R. J. Scalese, “A Critical Review of Simulation-Based Medical Education Research: 2003-2009,” Medical Education, Vol. 44, No. 1, 2010, pp. 50-63. http://dx.doi.org/10.1111/j.1365-2923.2009.03547.x
- B. Ram, M. Oluwole, R. L. Blair, R. Mountain, P. Dunkley and P. S. White, “Surgical Simulation: An Animal Tissue Model for Training in Therapeutic and Diagnostic Bronchoscopy,” The Journal of Laryngology and Otology, Vol. 113, No. 2, 1999, pp. 149-151. http://dx.doi.org/10.1017/S0022215100143415
- A. Ovassapian, S. J. Yelich, M. H. Dykes and M. E. Golman, “Learning Fibreoptic Intubation: Use of Simulators v. Traditional Teaching,” British Journal of Anaesthesia, Vol. 61, No. 2, 1988, pp. 217-220.
- R. Goldberg, H. G. Colt, M. Davoudi and L. Cherrison, “Realistic and Affordable Lo-Fidelity Model for Learning Bronchoscopic Transbronchial Needle Aspiration,” Surgical Endoscopy, Vol. 23, No. 9, 2009, pp. 2047-2052. http://dx.doi.org/10.1007/s00464-008-9951-7
- M. Davoudi, M. M. Wahidi, N. Zamanian Rohani and H. G. Colt, “Comparative Effectiveness of Lowand HighFidelity Bronchoscopy Simulation for Training in Conventional Transbronchial Needle Aspiration and User Preferences,” Respiration, Vol. 80, No. 4, 2010, pp. 327-334. http://dx.doi.org/10.1159/000318674
- A. H. Meier, C. L. Rawn and T. M. Krummel, “Virtual Reality: Surgical Application—Challenge for the New Millennium,” Journal of the American College of Surgeons, Vol. 192, No. 3, 2001, pp. 372-384. http://dx.doi.org/10.1016/S1072-7515(01)00769-4
- K. Moorthy, S. Smith, T. Brown, S. Bann and A. Darzi, “Evaluation of Virtual Reality Bronchoscopy as a Learning and Assessment Tool,” Respiration diseases, Vol. 70, No. 2, 2003, pp. 195-199.
- M. Davoudi, K. Osann and H. G. Colt, “Validation of Two Instruments to Assess Technical Bronchoscopic Skill Using Virtual Reality Simulation,” Respiration, Vol. 76, No. 1, 2008, pp. 92-101. http://dx.doi.org/10.1159/000126493
- R. Aggarwal, T. Grantcharov, K. Moorthy, J. Hance and A. Darzi, “A Competency-Based Virtual Reality Training Curriculum for the Acquisition of Laparoscopic Psychomotor Skill,” American Journal of Surgery, Vol. 191, No. 1, 2006, pp. 128-133. http://dx.doi.org/10.1016/j.amjsurg.2005.10.014
- S. Arora, D. Miskovic, L. Hull, K. Moorthy, R. Aggarwal, H. Johannsson, S. Gautama, R. Kneebone and N. Sevdalis, “Self vs Expert Assessment of Technical and Non-Technical Skills in High Fidelity Simulation,” American Journal of Surgery, Vol. 202, No. 4, 2011, pp. 500-506. http://dx.doi.org/10.1016/j.amjsurg.2011.01.024
- C. P. Marsland, B. J. Robinson, C. H. Chitty and B. J. Guy, “Acquisition and Maintenance of Endoscopic Skills: Developing an Endoscopic Dexterity Training System for Anesthesiologists,” Journal of Clinical Anesthesia, Vol. 14, No. 8, 2002, pp. 615-619. http://dx.doi.org/10.1016/S0952-8180(02)00456-7
- K. M. Martin, P. D. Larsen, R. Segal and C. P. Marsland, “Effective Nonanatomical Endoscopy Training Produces Clinical Airway Endoscopy Proficiency,” Anesthesia and Analgesia, Vol. 99, No. 3, 2004, pp. 938-944. http://dx.doi.org/10.1213/01.ANE.0000132998.19872.58
- J. S. Chen, H. H. Hsu, I. R. Lai, H. C. Tai, H. S. Lai, Y. C. Lee, J. S. Shaw, Y. P. Hung, P. H. Lee and K. J. Chang, “Validation of a Computer-Based Bronchoscopy Simulator Developed in Taiwan,” Journal of the Formosan Medical Association, Vol. 105, No. 7, 2006, pp. 569-576. http://dx.doi.org/10.1016/S0929-6646(09)60152-2
- R. Rowe and R. A. Cohen, “An Evaluation of a Virtual Reality Airway Simulator,” Anesthesia and Analgesia, Vol. 95, No. 1, 2002, pp. 62-66. http://dx.doi.org/10.1097/00000539-200207000-00011
- M. G. Blum, T. W. Powers and S. Sundaresan, “Bronchoscopy Simulator Effectively Prepares Junior Residents to Competently Perform Basic Clinical Bronchoscopy,” The Annals of Thoracic Surgery, Vol. 78, No. 1, 2004, pp. 287-291. http://dx.doi.org/10.1016/j.athoracsur.2003.11.058
- C. C. Kennedy, F. Maldonado and D. A. Cook, “Simulation-Based Bronchoscopy Training: Systematic Review and Meta-Analysis,” Chest, Vol. 144, No. 1, 2013, pp. 183-192. http://dx.doi.org/10.1378/chest.12-1786
- O. J. Hilmi, P. S. White, D. W. McGurty and M. Oluwole, “Bronchoscopy Training: Is Simulated Surgery Effective?” Clinical Otolaryngology and Allied Sciences, Vol. 27, No. 4, 2002, pp. 267-269. http://dx.doi.org/10.1046/j.1365-2273.2002.00577.x
- S. Ameur, K. Carlander, K. Grundstrom, P. Hallberg, K. Lundgren, P. G. Lundquist and T. Wikstrom, “Learning Bronchoscopy in Simulator Improved Dexterity Rather than Judgement,” Lakartidningen, Vol. 100, No. 35, 2003, pp. 2694-2699.
- F. Agro, F. Sena, E. Lobo, S. Scarlata, N. Dardes and G. Barzoi, “The Dexter Endoscopic Dexterity Trainer Improves Fibreoptic Bronchoscopy Skills: Preliminary Observations,” Canadian Journal of Anaesthesia, Vol. 52, No. 2, 2005, pp. 215-216. http://dx.doi.org/10.1007/BF03027742
- E. S. Deutsch, T. Christenson, J. Curry, J. Hossain, K. Zur and I. Jacobs, “Multimodality Education for Airway Endoscopy Skill Development,” The Annals of Otology, Rhinology, and Laryngology, Vol. 118, No. 2, 2009, pp. 81-86.
- N. Jabbour, T. Reihsen, R. M. Sweet and J. D. Sidman, “Psychomotor Skills Training in Pediatric Airway Endoscopy Simulation,” Otolaryngology—Head and Neck Surgery, Vol. 145, No. 1, 2011, pp. 43-50. http://dx.doi.org/10.1177/0194599811403379
- D. R. Stather, P. Maceachern, K. Rimmer, C. A. Hergott and A. Tremblay, “Assessment and Learning Curve Evaluation of Endobronchial Ultrasound Skills Following Simulation and Clinical Training,” Respirology, Vol. 16, No. 4, 2011, pp. 698-704. http://dx.doi.org/10.1111/j.1440-1843.2011.01961.x
- D. R. Stather, P. MacEachern, A. Chee, E. Dumoulin and A. Tremblay, “Evaluation of Clinical Endobronchial Ultrasound Skills Following Clinical versus Simulation Training,” Respirology, Vol. 17, No. 2, 2012, pp. 291- 299. http://dx.doi.org/10.1111/j.1440-1843.2011.02068.x
- S. W. Crawford and H. G. Colt, “Virtual Reality and Written Assessments Are of Potential Value to Determine Knowledge and Skill in Flexible Bronchoscopy,” Respiration, Vol. 71, No. 3, 2004, pp. 269-275. http://dx.doi.org/10.1159/000077425
- H. G. Colt, S. W. Crawford and O. Galbraith III, “Virtual Reality Bronchoscopy Simulation: A Revolution in Procedural Training,” Chest, Vol. 120, No. 4, 2001, pp. 1333-1339. http://dx.doi.org/10.1378/chest.120.4.1333
- J. E. Smith, A. P. Jackson, J. Hurdley and P. J. Clifton, “Learning Curves for Fibreoptic Nasotracheal Intubation When Using the Endoscopic Video Camera,” Anaesthesia, Vol. 52, No. 2, 1997, pp. 101-106. http://dx.doi.org/10.1111/j.1365-2044.1997.23-az023.x
- R. M. Fanning and D. M. Gaba, “The Role of Debriefing in Simulation-Based Learning,” Simulation in Healthcare, Vol. 2, No. 2, 2007, pp. 115-125. http://dx.doi.org/10.1097/SIH.0b013e3180315539
- T. McCashland, R. Brand, E. Lyden and P. de Garmo, “The Time and Financial Impact of Training Fellows in Endoscopy. Cori Research Project. Clinical Outcomes Research Initiative,” The American Journal of Gastroenterology, Vol. 95, No. 11, 2000, pp. 3129-3132. http://dx.doi.org/10.1111/j.1572-0241.2000.03280.x
- R. M. Epstein, “The Costs of Making Practice More Cost-Effective,” JAMA: The Journal of the American Medical Association, Vol. 287, No. 13, 2002, pp. 1648-1649.
- J. B. Cooper and V. R. Taqueti, “A Brief History of the Development of Mannequin Simulators for Clinical Education and Training,” Postgraduate Medical Journal, Vol. 84, No. 997, 2008, pp. 563-570. http://dx.doi.org/10.1136/qshc.2004.009886
- M. Davoudi, H. G. Colt, K. E. Osann, C. R. Lamb and J. J. Mullon, “Endobronchial Ultrasound Skills and Tasks Assessment Tool: Assessing the Validity Evidence for a Test of Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration Operator Skill,” American Journal of Respiratory and Critical Care Medicine, Vol. 186, No. 8, 2012, pp. 773-779. http://dx.doi.org/10.1164/rccm.201111-1968OC
NOTES
*The authors do not have any conflicts of interest related to this manuscript.
#Corresponding author.

