Open Journal of Modern Neurosurgery
Vol.06 No.01(2016), Article ID:62553,5 pages
10.4236/ojmn.2016.61004
Spinal Cord Compression Caused by Multifocal Histoplasmosis Treated Conservatively: Case Report and Literature Review
Dominique N’Dri Oka*, Alban Slim Mbende, Daouda Sissoko
Neurosurgery Unit, Yopougon Teaching Hospital, Abidjan, Côte d’Ivoire

Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 24 November 2015; accepted 3 January 2016; published 6 January 2016
ABSTRACT
We present the case of a 39-year-old patient admitted for a slow thoracic spinal cord compression syndrome associated with lumbar rachialgia. CT scan and MRI of the thoracic spine showed lysis of T4, T5, T6 and T7 vertebrae, an epiduritis and paravertebral abscesses. CT scan of the lumbar spine demonstrated osteolysis of the left iliac wing with skin invasion. This lesion infiltrated the sacrum and the body of L5. The iliac lesion was biopsied and the analysis revealed a granulomatous osteitis caused by Histoplasma duboisii. The treatment consisted of ketoconazole 400 mg daily for six months. Spinal decompressive surgery was not performed. Following antifungal treat- ment the patient had satisfying clinical and radiological outcome. After three years’ follow-up, the clinical course was uneventful. The patient had neither symptoms of spinal cord compression nor signs of further localizations.
Keywords:
Histoplasma duboisii, Bone Multiple Localization, Spinal Cord Compression

1. Introduction
Histoplasmosis is an infectious disease caused by two fungi: Histoplasma capsulatum and Histoplasma duboisii. Histoplasma capsulatum or American histoplasmosis is a small yeast which is responsible for granulomatous reaction rich in histiocytic mononuclear cellsandis more widespread and cosmopolitan. The duboisii variety of Histoplasma capsulatum or African histoplasmosis is a large yeast which causes giant cell granulomatous reaction and is widespread in sub-Saharan Africa. Generally speaking, the disease is acquired by inhaling the spore stage of the fungus. But Histoplasma duboisii is acquired mostly through skin opening and the digestive route [1] . Inhalation seems unlikely because of the rarity of pulmonary forms, unlike Histoplasma capsulatum, in which lung involvement is common. Disseminated forms of Histoplasma duboisii are characterized by multiple locations, mucocutaneous, visceral, neuro-meningeal, lymph node, bone and joint. Cutaneous and lymphatic involvements are the most common [2] . The disco-vertebral involvement is rare and poses the problem of differential diagnosis with spinal tuberculosis or Pott’s disease in the African context [3] . Pathological examination is usually the most contributory to the diagnosis of bone lesions [4] . The therapeutic means may be limited to the specific medical treatment, or associated with an orthopedic device and/or surgery. We sought to report a rare case of vertebral histoplasmosis associated with multiple osseous localization of Histoplasma duboisii to investigate its pathophysiology and discuss the diagnosis and treatment.
2. Observation
Mr. YKK, a 39-year-old ivorian, HIV immunocompetent and no other medical history, presented in February 2011 with progressive deterioration of his general health, thoracic rachialgia and intercostal pain, low back pain and lower limbs heaviness. Clinical examination revealed a slow thoracic spinal cord compression syndrome with a slight deficit and a 4/5 muscle strength of the lower limbs, a lumbosacral spine syndrome. CT scan and MRI of the thoracic spine showed lysis of T4, T5, T6 and T7 vertebrae, an epiduritis and paravertebral abscesses (Figure 1). CT scan of the lumbar spine demonstrated osteolysis of the left iliac wing with skin invasion. This lesion invaded the sacrum and the body of L5 (Figure 1). MRI of the lumbar spine showed no nerve root compression (Figure 1). Several diagnosis hypotheses were suggested: a multifocal tuberculosis (vertebral and iliac) or infection with other microorganisms (bacterial or parasitic), vertebral and iliac metastasis. A thoraco-abdo- minopelvic CT scan to search for a primary cancer was non-conclusive. An iliac bone biopsy performed revealed a giant cell granulomatous tissue, with large ovoid yeast consistent with Histoplasma duboisii. Histopathological examination of osseous biopsy concluded bone histoplasmosis with multiple localization of Histoplasma duboisii. The patient was treated with ketoconazole 400 mg daily for six months. Spinal decompressive surgery was not performed. Our conservative approach was based on clinical grounds of minimal neurological disorders and normal spine morphology. Following antifungal treatment the patient had satisfying clinical and radiological outcome. After three years follow-up, the clinical course was uneventful. The patient had neither symptoms of spinal cord compression nor signs of further localizations.
3. Discussion
Regions of outbreaks of histoplasmosis Histoplasma duboisii seem limited to sub-Saharan Africa and the island of Madagascar. The cases described in Europe would be imported from Africa.
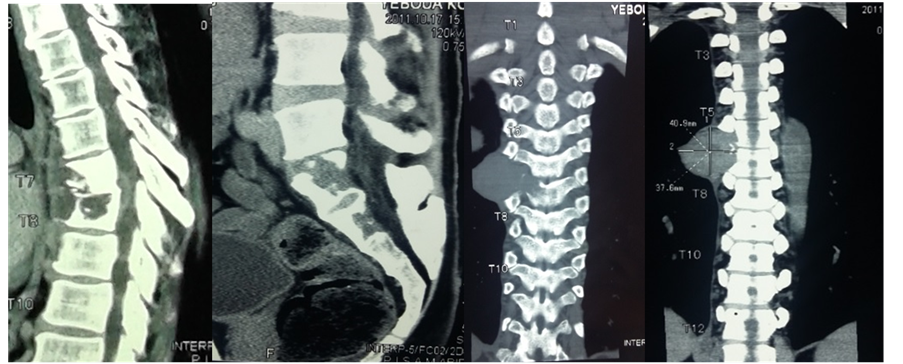

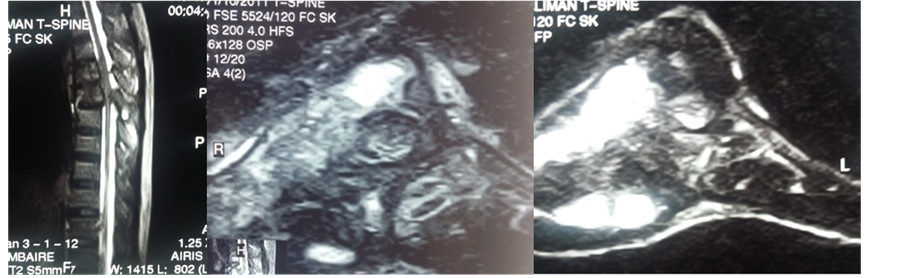
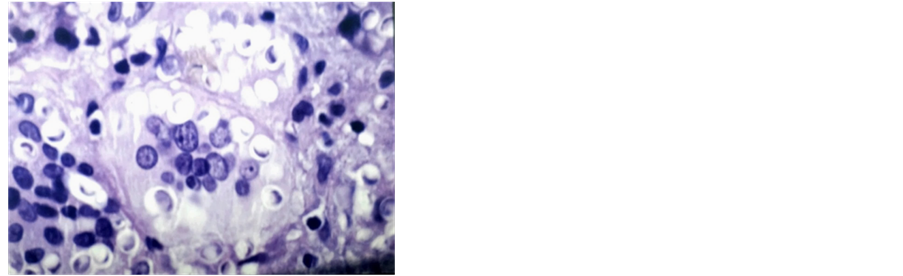
Figure 1. Sagittal view of thoracic CT scan showing osteolytic lesion T4, T5, T6 and T7 vertebral (a) at the sacrum, (b) thoracic frontal view (T5 to T7) lumbar frontal view osteolyic lesion and abcess (e) axial view with osteolytic in vertebral extending to pleural (f), axial view ilac osteolytic lesion (g) T1 weighted sagittal view showing spinal cord compression associated to vertebral body lesion (h) T2 weighed MRI on sagittal view, showing T4 - T7 epiduritis and paravertebral abscesses which is hyposignal (i) and (j). Histological examination showing Histoplasma duboisii in giant cell (Schiff periodic acid coloration ×100 (k).
Spinal localization of histoplasmosis is rare and exceptional. Very few publications have been devoted on the matter [5] - [8] . Unlike Histoplasma capsulatum, Histoplasma duboisii has rarely been associated with HIV infection [9] . The pathogenesis of Histoplasma duboisii spondylitis is the subject of numerous discussions and has not been definitively established. In fact, Histoplasma duboisii is acquired mostly through skin opening and the digestive route [10] . Dissemination of Histoplasma duboisii through bloodstream or lymphatic system might explain its multiple locations. But blood spread of the infection would better reinforce the theory of bone tropism of the Histoplasma duboisii. Thus, the initial spinal lesions would be vertebral first because the intervertebral disc and fibrocartilage are avascular.
Unlike American histoplasmosis, the African variety seems less affected by HIV. Contamination in humans would be through contact with spores, particularly abundant in confined spaces such as caves and tunnels, galleries (inhabited by bats) or in rural areas, farms, silos, pigeon habitats, intensive poultry farming (chickens) [11] [12] . Our patient had a permanent contact with poultry.
Clinically, bone histoplasmosis grows insidiously with waves of bone pain, low-grade fever and slight deterioration of general health [8] . The clinical profile of spinal Histoplasma duboisii infection does not present any particularities. Also, in the absence of pathological and mycological arguments, some clinical situations are often confusing: in particular, Pott’s disease because of its radiological and even histological resemblance, brucellosis, spinal tumors and certain fungal spondylitis (aspergillosis and candidosis). This radiological resemblance was reported by several authors [12] -[14] .
Proof of vertebral involvement is based on imaging. Plain radiography revealed a vertebral osteolysis, absence of bone reconstruction and sometimes the presence of paravertebral abscesses.
MRI can show, as in our case, an image of epiduritis over spinal injuries. The 3D scanner and T1 weighted MRI imaging better specify these lesions including spinal deformities. Radiological images can mimic other conditions such as spinal vertebral metastasis or other spinal infection. Pott’s disease is the first differential diagnosis of spinal histoplasmosis in the African context where TB is endemic [3] [4] [12] .
Tumor pathologies may also be a differential diagnosis. Spinal histoplasmosis simulating a progressive relapse of a non-Hodgkin lymphoma treated 10 years ago was described in Morocco [13] .
CT scan and MRI will help decide surgical indications based on vertebral and medullary lesions.
Mycological diagnosis is established by isolation of Histoplasma duboisii from the samples taken by surgical or percutaneous biopsy guided by the scanner.
Direct examination of fresh samples might yield yeasts. Culture is possible on Sabouraud medium, to obtain the mycelium, the same appearance as that of Histoplasma capsulatum [7] [8] . Special culture techniques will reveal yeast characteristic form [8] : these are the circles and Pine Drouhet of Kurung, mid-brain-heart blood, and blood to the middle Campbell. The culture conditions are often difficult, explaining a positive culture in 50% of cases [1] [8] . Faster ways of detecting Histoplasma. capsulatum exist thanks to current advances in molecular biology: immunofluorescence on the samples, looking for antigens by ELISA and detection of DNA or RNA by PCR (polymerase chain reaction) to determine biovars of Histoplasma duboisii. Finally, other less specific means such as serology (agglutination, AGID, complement fixation test and indirect immunofluorescence) and the intradermal reaction to histoplasmin have long been diagnostic methods.
Histopathological examination of biopsy is a sensitive diagnostic method in 87% of cases [1] [2] [8] as was the case in our observation. The typical histological appearance of Histoplasmosis is a granulomatous inflammatory and giant cell with lymphocytes phenomenon, rare and polynuclear giant cells with many nuclei arranged in clusters. These giant cells are plasmodia containing many distinctivetypes of yeast. Staining on mucicarmin gives them, in polarized light, a “Maltese cross” like aspect [1] . The problem of differential diagnosis with TB may also arise at this stage since tuberculosis presents as a granulomatous reaction on pathology examination.
Treatment options are not yet well codified. But medical treatment is the first alternative and may include surgery or contention with brace. Amphotericin B, ketoconazole and itraconazole are the most used molecules. According to the American Society of Infectious Disease (ASID), the recommended treatment is amphotericin B deoxycholate (1 mg/kg per day) for 4 - 6 weeks. A therapeutic alternative is amphotericin B deoxycholate (1 mg/kg per day for 2 to 4 weeks) relayed by itraconazole (5 - 10 mg/kg per day) for 3 months [8] [15] .
Our choice fell on ketoconazole due to its easy administration and good tolerability.
Conservative treatment including antifungal therapy andorthopaedic device may be indicated in small vertebral lesions without epiduritis [15] . Orthopaedic devices are different depending on the affected segment. In the cervical spine, we have rigid or flexible collars, and in thoracolumbar lesions, corsets can be used [15] .
Surgery is indicated in spondylitis complicated with neurological disorders, loss of vertebral height of more than 50%, spinal instability and thoracic kyphosis of more than 20˚. The surgery involves debridement of lesions, diskectomy, removal of bone debris, and an opening of the dorsal longitudinal ligament when there is an epidural abscess. Surgical procedures are performed using an anterior approach. Autologous graft and osteosynthesis might be necessary.
Despite bone lysis, we opted in our case for a conservative treatment, given minimal neurological disorders and normal spine morphology. The result was satisfactory. According to Alberto Di Martino and colleagues in Italy, conservative treatment is the main attitude adopted today in the treatment of spondylitis [16] .
4. Conclusion
Spinal involvement of Histoplasma duboisii is rare. It can simulate Pott’s disease at all stages of his diagnosis. The definitive diagnosis is made on mycological and pathological examination. In the absence of significant neurological deficit and spinal instability, conservative treatment provides a good outcome.
Conflict of Interest
No funds were received in support of this study.
Cite this paper
DominiqueN’Dri Oka,Alban SlimMbende,DaoudaSissoko, (2016) Spinal Cord Compression Caused by Multifocal Histoplasmosis Treated Conservatively: Case Report and Literature Review. Open Journal of Modern Neurosurgery,06,20-24. doi: 10.4236/ojmn.2016.61004
References
- 1. Vorhauer, R., Brière, J., Passa, P. and Chelloul, N. (1976) Diagnostic histologique de l’histoplasmose à “grandes formes”. à propos de deux observations. Arch Anat Cytol Pathol., 6, 463-467.
- 2. Debrie, J.C., Thomas, J., Menard, M., Quiniou, M. and Salaun, J.J. (1981) Laryngeal Histoplasmosis Caused by Histoplasma duboisii. Dakar Med, 26, 26-32.
- 3. Musoke, F. (2001) Spinal African Histoplamosis Simulating Tuberculous Spondylitis. African Health Sciences, 1, 28- 29.
- 4. Minta, D.K., Sylla, M., Traoré, A.M., et al. (2014) Première observation malienne d’histoplasmose africaine disséminée à prédominance osseuse chez un enfant VIH négatif. Revue de la littérature. Journal de Mycologie Médicale, 24, 152-157.
http://dx.doi.org/10.1016/j.mycmed.2013.08.001 - 5. Camain, R., Berthe, M., Klefstad-Sillonville, F., et al. (1958) Sept nouveaux cas d’histoplasmose observés en AOF. Bulletin de la Société de Pathologie Exotique, 1, 83-107.
- 6. Drexler, L. (1968) L’aspect radiologique de l’histoplasmose africaine. Annales de la Societe Belge de Medecine Tropicale, 6, 607-612.
- 7. Gentilini, M. (1995) Mycoses profondes. Médecine Tropicale, 3, 268-288.
- 8. Gentilini, M., Brucker, G., Danis, M., et al. (1980) Dix cas d’histoplasmose: Aspects cliniques, biologiques et thérapeutiques. Annales de Médecine Interne, 4, 209-212.
- 9. Chandenier, J., Gomad, D., Moyen, G., et al.(1995) Histoplasmose africaine à Histoplasma capsulatum var. duboisii: Liens avec le SIDA. à propos de cas congolais récents. Cahiers Santé, 5, 227-234.
- 10. André, C., Badoual, J., Kalifa, G. and Dubousset, J. (1984) Histoplasmose africaine: Une observation. Archives Francaises de Pédiatrie, 41, 429-431.
- 11. Peloux, Y., Camain, R., Courson, B. and Quenum, C. (1965) L’histoplasmose. Médecine Tropicale, 4, 439-445.
- 12. N’Dri Oka, D., Varlet, G., Kakou, M., et al. (2001) Spondylodiscite à Histoplasma duboisii: A propos de deux observations et revue de la littérature. Neurochirurgie, 47, 431-434.
- 13. Tazi, E.M., Essadi, I., Serraj, K., et al. (2009) Histoplasmose sacrée dix ans après un lymphome non hodgkinien du sacrum: A propos d’un cas. Cancer/Radiothérapie, 13, 337-339.
http://dx.doi.org/10.1016/j.canrad.2009.03.004 - 14. Carme, B., Hayette, M.P., Itoua-Ngaporo, A., Ngolet, A., et al. (1993) Histoplasmose africaine à Histoplasma duboisii (histoplasma capsulatum var. duboisii): Quatorze cascongolais observés en 10 ans (1981-1990). Journal de Mycologie Médicale, 3, 67-73.
- 15. Collomb, H., Camain, R., Courson, B. and Quenum, C. (1962) Paraplégie aigue par ostéolyse due à Histoplasma capsulatum variété duboisii. Bulletin de la Société de Pathologie Exotique, 5, 753-756.
- 16. Di Martino, A., Papapietro, N., Lanotte, A., et al. (2012) Spondylodiscitis: Standards of Current Treatment. Current Medical Research & Opinion, 28, 689-699.
http://dx.doi.org/10.1185/03007995.2012.678939
NOTES
*Corresponding author.


