Open Journal of Orthopedics
Vol.04 No.06(2014), Article ID:47214,7 pages
10.4236/ojo.2014.46027
Changes in Attitudes toward Lumbar Spinal Stenosis Treatment
Shin-ichi Konno, Miho Sekiguchi
Department of Orthopaedic Surgery, Fukushima Medical University School of Medicine, Fukushima, Japan
Email: fortho@fmu.ac.jp
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 20 April 2014; revised 3 June 2014; accepted 20 June 2014
ABSTRACT
As the environment surrounding healthcare continues to evolve, there is a need to revise outcome assessment criteria. A shift is being demanded in diagnosis and treatment outcome assessment practices from objective to subjective assessment and from evaluation by doctors to assessment that is based on the patient’s own perspective. Therefore, lumbar diseases must now be assessed from multiple perspectives. Some major indices for evaluation are pain and numbness, functional status, general health status, disability, and patient satisfaction. An effective assessment method for lumbar spinal stenos is that examines symptoms, quality of life, and healthcare economics as key assessment factor is reviewed.
Keywords:
Lumbar Spinal Stenosis, Quality of Life, Healthcare Economics, Multiple Assessments

1. Introduction
As the environment surrounding healthcare continues to evolve, there is a need to revise outcome assessment criteria. A shift from objective to subjective assessment and from evaluation by doctors to assessment that is based on the patient’s own perspective is being demanded. Lumbar spinal stenosis (LSS) is one of the spinal disorders, and causes various symptoms. In the past, the principal assessment item was whether symptoms were eliminated. However, new concept requires a focus on not only relief from symptoms but also quality of life (QOL) and patient satisfaction as a multidimensional assessment. An effective assessment method for lumbar spinal stenosis that examines symptoms, QOL, and healthcare economics as key assessment factors is reviewed.
2. Current Need for Re-Evaluation of Diagnosis and Assessment Criteria
The environment surrounding healthcare is evolving. One reason is the awareness of those paying for treatment of the risk of escalating healthcare costs. As a result, patients and those paying for treatment now demand that healthcare professionals use methods and concepts of evidence-based medicine (EBM), assessment of cost- effectiveness, and patient satisfaction ratings. Accordingly, revisions must also be made to outcome assessment criteria. Tests to verify the appropriateness of conventional medical care practices assume that assessment crite- ria are correct measurements of their appropriateness. As healthcare costs continue to rise, patients and those paying for care are requesting accountability, clarification of treatment efficacy, and proof of the appropriate- ness of expensive medical care treatments. There are several reasons for this trend.
First is the relationship between the cost and the quality of treatment, since there is a cap on the efficacy of treatment past which the outcome cannot be improved no matter how much more money is invested in medical care. A second reason is that there are regional differences in the frequency of surgical procedures performed. Healthcare providers do not have sufficient grounds for convincing third parties that such a difference is ac- ceptable. The third reason is changes in public attitudes. There is an increasing public awareness that individuals must be held responsible for their own health, and that they must actively seek out healthcare professionals to willingly offer expert advice and guidance required for the individual’s various health-related needs. Meanwhile, healthcare providers are becoming more concerned that their historical privilege of autonomy is gradually being lost in the current medical world.
The British Medical Association gives four reasons for the need to revise the current state of the medical community: 1) first and foremost, the responsibilities of patients and society related to limited financial resources; 2) for maintenance of autonomy in the medical community, demands from the public that such autonomy is effective and clearly serves the public interest and that it is transparent; 3) demands from the public that the medical community more actively seeks collaboration with other entities in the field of health to provide better treatment for patients; and 4) generational differences among medical practitioners in their response to the various issues faced in the field of medicine.
3. Importance of Diagnosis and Assessment Criteria
If asked what diagnosis and treatment methods can achieve the best outcome with the minimal healthcare resources, medical providers would not have enough data to provide an answer. One reason for this is that various reports on treatment outcomes for a single disease cannot be compared, as there are no unified criteria for assessing the disease. A particular issue is that conventional methods of analysis have often not even been tested for reliability. Even if data are provided with claims of good efficacy of the relevant treatment, issues remain with the reliability of the treatment method that is the underlying foundation. A certain conclusion based on such results may be unfounded due to the lack of reliability. Another problem is that conventional diagnosis and assessment criteria have not necessarily evolved to adapt to changes in public attitudes towards healthcare. In the current era, the public is demanding that healthcare providers alter the general concepts surrounding diagnosis and treatment outcome assessment. Such changes include a shift from objective to subjective assessment and from evaluation by doctors to assessment that is based on the patient’s own perspective.
Under such circumstances, unfortunately, it is difficult for healthcare providers to respond to these demands of patients and society with information on diagnosis and treatment that is based on conventional assessment criteria. Diagnosis and treatment assessment criteria are already being overhauled in Western countries. For Japan to continue contributing to the diagnosis and treatment of musculoskeletal diseases, it must provide third parties with results that conform to global standards.
4. Requirements for Diagnosis and Assessment Criteria
In the past, assessments of diagnosis and treatment outcome were solely the interest of healthcare professionals. Now, such assessments are essential information required by the government and those who are paying for healthcare. This is because assessment criteria are the most critical measure of not only cost, but also of the appropriateness and efficacy of diagnosis and treatment. A critical challenge right now is to develop assessment criteria that satisfy not only healthcare professionals, but also patients and society as a whole.
Naturally, multiple assessment items are needed to satisfy all these different players, each with their own perspectives. In addition, the presence and extent of various impairments in day-to-day life that give rise to chief complaints must all be assessed simultaneously. The chief complaints of herniated discs and lumbar spinal stenosis (LSS) are lower back and leg pain and leg numbness. In the past, the principal assessment item was
whether pain and numbness were eliminated. Multidimensional assessment based on new concepts requires a focus on not only relief from pain and numbness, but also other factors such as change in walking ability, patient quality of life (QOL), and patient satisfaction. In other words, diagnosing and treating herniated discs and LSS requires healthcare that is not aimed at eliminating pain and numbness, but rather at asking the reason for pain and numbness and determining what impairments exist. For example, in a person with a herniated disc, the most characteristic pain-related impairments are painful at the flexion position and painful kneeling. In a person with LSS, it is the inability to walk long distances. Even if the Japanese Orthopaedic Association (JOA) score (a criteria for assessing back pain disease outcome) improves with surgery, soon after the operation, nearly all of those with herniated discs and over half of those with LSS avoid heavy labor, and more than half of patients must use handrails when climbing stairs. Assessing treatment outcome with multiple dimensions to determine impairments caused by the disease can elucidate the whole picture. Developing such assessment criteria could help clarify the most appropriate diagnosis and treatment methods and eventually yield great benefits to patients and society as a whole.
5. Multimodal Assessment of LSS
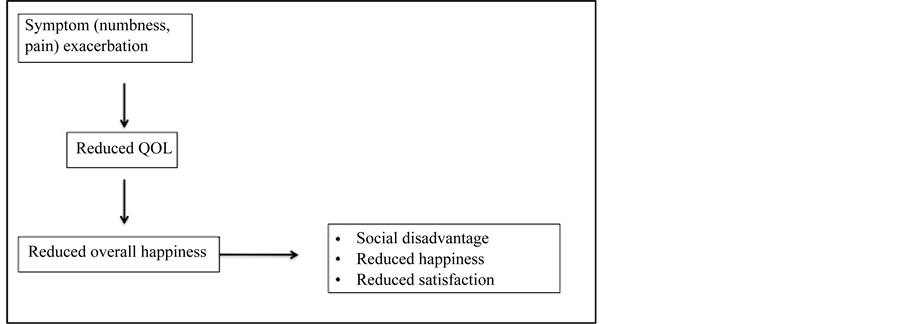
LSS can hinder the activities of not only the patients themselves, but also of their friends and family. In recent years, new indices that assess LSS from the perspective of the effects on the community, as opposed to the patient alone, have been coming into the spotlight. These indices, called patient-based outcomes, are subjective outcome indicators that are based on the perspective of patients and their family members. Some major such indices are pain and numbness (symptoms), functional status, general health status, disability, and patient satisfaction. Considering LSS from this point of view enables the development of the following LSS-related model. Specifically, the onset of leg pain and numbness induces a reduction in QOL, i.e. a reduction in functional status. According to the model, this affects the overall health and, by extension, the level of social disadvantage and of subjective happiness and satisfaction of the patient (Figure 1).
Considering the meaning of treatment for leg pain and numbness according to this model gives rise to a different treatment concept than the one in conventional use. Specifically, treatment for leg pain and numbness takes the perspective of traditional treatment methods aimed at alleviating those symptoms and adds a new important element, building of a healthcare system that involves asking the reason for pain and numbness and determining what impairments patients experience in their daily lives (Figure 2). In this concept, relief from pain and numbness is not the goal, but the means to achieve the goal. Intervention from healthcare providers to treat patient impairments using this perspective can also help raise patient QOL and happiness. Studies are needed to determine the effects of physical and psychological support from healthcare providers on patient impairments and differences in patient QOL and happiness versus situations without such support.
Figure 1. A model of patient’s overall health. The onset of leg pain and numbness induces a reduction of QOL, i.e., physical function, social function, role of physical, and/or general health. Reduction of QOL included mental health and/or role of emotion influences overall happiness. Furthermore, a social disadvantage and dissatisfaction of the patient are induced.
Figure 2. Treatment goals. Treatment goals should be not only relief their symptoms but also improvement of QOL. Relief from pain and numbness is the means to achieve the goal. In addition, intervention from healthcare providers to treat patient impairments can help raise patient QOL and happiness.
Such studies clearly indicate the importance of multimodal LSS assessment based on the patient’s perspective. However, cross-sectional studies cannot determine the extent to which pain and numbness relief and improvement in functional status affect health management, social participation, happiness, and health satisfaction of patients. This goal requires the use of longitudinal studies. In a recent longitudinal study, we found that exacerbation/improvement in the extraneous factors and degree of leg pain and numbness of patient affects exacerbation/improvement of functional disability related to LSS. However, this was only true in about 5% of cases. Assessing the improvement in leg pain and numbness from the patient’s perspective requires the use of multiple patient-based outcomes for a more multimodal assessment. Aside from changes in social inclusion and subjective happiness, changes in indicators observed in cross-sectional studies were shown to be interconnected in a way that is congruent with the model. In other words, limitations in day-to-day life due to leg pain and numbness affect both general sense of health and health satisfaction.
The results of the study suggested a number of patient-based outcome measures for leg pain and numbness: pain severity (Visual Analog Scale = VAS), numbness severity (VAS), walking ability (measurement of distance), physical health, social activities, and health satisfaction. As social inclusion and subjective happiness are also affected by numerous factors other than leg pain and numbness, they are not appropriate as patient-based outcome measures.
6. Multimodal Assessment of Treatment for Leg Pain and Numbness
Traditional evaluation of treatment for leg pain and numbness is centered on pathophysiological and anatomicopathological indicators. However, these indicators are not always important for the patient and society, for whom improvement of symptoms and QOL may be more relevant [1] . That said, the subjective nature of pain, numbness, and QOL make them difficult to assess objectively. Assessment of these symptoms is actually evaluation of the expression of pain and numbness and of actions related to pain and numbness, as alternatives to assessing the level of leg pain and numbness and QOL directly [2] . Moreover, judgment of efficacy differs greatly depending on whether a patient-based or healthcare provider-based assessment perspective is used. In the latter case, bias is likely to come into play. In the former case, assessment based solely on the patient’s subjective evaluation is not always appropriate. In other words, using one of the two perspectives alone can only provide a limited assessment of the efficacy of LSS treatment. A multimodal assessment that combines all required assessment methods is essential. Indices for assessing LSS can be largely grouped into three categories: (1) verbal or written expression of pain and numbness (strength, patterns, characteristics); (2) changes in activities of daily living (ADL) and QOL due to pain and numbness; and (3) psychological and mental effects of pain and numbness [3] .
6.1. Degree of Leg Pain and Numbness (Quantitative Evaluation)
Measurement of the strength of leg pain and numbness must be simple and easy. In addition, measures must be able to assess pain and numbness in the patient quickly. It must also be easy to compare pre- and post-treatment pain and numbness in individual patients [4] . When evaluating treatment efficacy from the strength of pain and numbness measured before and after treatment, it must also be possible to examine ‘clinically important differences’, i.e. to consider what degree of improvement in pain and numbness symptoms is clinically significant.
A Visual Analog Scale (VAS) [5] [6] is a method for measuring the severity of pain and numbness felt by patients by showing them a 10-cm (100-mm)-long line with the left end-point being no pain/numbness and the right being the worst pain/numbness imaginable. Pain and numbness severity is noted from 0 to 100 mm. Measurements are treated as continuous variables in statistical analysis. The VAS is often used in this case for its capacity to measure pain and numbness intuitively and its ease of application. It has also been reported to be extremely sensitive. However, while it is useful for assessing short-term changes in pain and numbness, it cannot correctly show long-term changes in pain and numbness in some cases. In addition, it should be noted that this method cannot be used to compare different patients. It is useful for measuring the severity of pain and numbness and changes in that severity in individual patients. A level of pain or numbness of 30 mm or more on the VAS is considered moderate pain/numbness [7] . A change of 20 mm or more on the VAS indicates a significant change in pain/numbness, and a change of 40 mm or more by a treatment indicates a complete response [8] .
The Numeric Rating Scale (NRS) [9] - [11] is a method whereby patients select a number along an 11-point scale for strength of pain and numbness from 0 (no pain/numbness) to 10 (maximum pain/numbness). The NRS is easy to use because responses can be verbal rather than written. However, number preferences can affect the results. It has a benefit over the VAS in that it is more easily comprehensible to patients and can be given over the phone or in other situations that are not face-to-face. The Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) recommends using the NRS as a pain evaluation scale for assessing chronic pain [12] . According to the minimal clinically important difference (MCID) for chronic pain in motor organs, an improvement of 2.0 points or 33.0% is stated to be an effective improvement [13] .
With the Verbal Rating Scale (VRS) [10] , patients select the severity of pain or numbness based on words describing the severity of pain/numbness on a four- or five-point scale alongside numerical values shown in or- der. For example, with possible options of 0: no pain/numbness, 1: mild pain/numbness, 2: severe pain/numb- ness and 3: unbearable pain/numbness, patients respond verbally with the number that represents their current strength of pain/numbness. A disadvantage is that the range of scores representing pain/numbness strength is ambiguous.
The Face Rating Scale (FRS) [14] is a method whereby patients select a drawing of a face showing pain or numbness as the strength of the pain or numbness they are feeling. It is for patients aged three years and older. It is also easy for older adults to understand. The FRS shows drawings of faces exhibiting pain/numbness along a six-point scale, with 0: no hurt, 1: hurts a little bit, 2: hurts a little more, 3: hurts even more, 4: hurts a whole lot and 5: hurts worst.
6.2. QOL in Patients with LSS
There are comprehensive scales for evaluating general health status that are not limited to individuals, and there are more specific scales for assessing the QOL of specific diseases that are limited to subjects with that disease.
(1) Comprehensive QOL scales
The Medical Outcomes Study (MOS) 36-Item Short-Form Health Survey (SF-36®) is a scale for measuring health-related quality of life (HRQOL). It has been verified to have scientific reliability and appropriateness and is the most commonly used QOL scale internationally. A Japanese version has also been developed [15] [16] . It is a self-administered questionnaire comprised of 36 questions with responses on a three- or five-point scale. The results are scored with eight subscales: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH). Each of the eight subscales can also be used individually. Overall evaluations are based on three summary scores: a physical component summary (PCS), a mental component summary (MCS), and a role/social component summary (RCS). Since they are all formed under the common concept of HRQOL, they can measure HRQOL of various diseases, and comparisons can be made between patients with different diseases or with healthy, unimpaired individuals. National standards exist for comparing deviations. There is also a brief version called the SF-12. In addition, an SF8 Health Survey (SF-8TM) has also been developed with only eight questions to be given quickly.
The EuroQol (EQ-5D) [17] is used across the globe, mostly in Europe. It is comprised of five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) with three levels each and a VAS for self-rated health of the respondent. The sum of all the responses comprises the score (utility value), with 1 being the best health and 0 being death.
The Oswestry Low Back Pain Disability Questionnaire (ODI) [18] - [20] is a self-rated scale that assesses functional disability associated with leg pain and numbness. One of six responses (0 to 5 points) is selected for 10 questions asking about the severity of pain, disability in ADL, sleep, sex life, and social life. Higher scores indicate more severe disability. Of the 10 questions, 9 deal with limitations of daily activities. A Japanese version has also been developed.
(2) Disease-specific QOL scales
The Japanese Orthopaedic Association (JOA) Back Pain Evaluation Questionnaire (JOABPEQ) [21] [22] is a QOL scale specifically for back pain that was constructed in April 2007 as a JOA project. It is a self-rated questionnaire of 25 questions to assess five factors: pain-related disability (four questions), lumbar disability (six questions), walking disability (five questions), social activity disability (four questions), and psychological disability (seven questions). Each factor is given a score from 0 to 100, with larger scores indicating milder impairment. Since each factor is independent, they are evaluated separately, and the total score holds no meaning. One characteristic is that the questions are weighted. Questions are given more weight if they are more strongly related to the severity of back pain in order to more accurately assess severity. Since scoring is somewhat complicated, a dedicated spreadsheet is used to calculate the score. The spreadsheet can be downloaded from the JOA or Japanese Society for Spine Surgery and Related Research website.
The Zurich Claudication Questionnaire (ZCQ) [23] considers LSS severity, physical functioning, and satisfaction from various angles to give an overall assessment. The self-rated English version of the questionnaire has 18 questions and is a disease-specific scale to assess LSS. The ZCQ is known by a variety of names, including the Swiss Spinal Stenosis Measure and the Brigham Spinal Stenosis Questionnaire. There is also a Japanese translation for this scale.
6.3. Healthcare Economics Assessment of LSS
Spending large amounts of money on healthcare does not always ensure an improvement in health. It is therefore necessary to scientifically verify which treatment methods can achieve the best outcome with the minimal healthcare resources.
Quality-adjusted life years (QALY) [24] is an assessment method that does not simply assess the extension of survival, but rather emphasizes utility values that represent QOL. It measures both the survival period (quantita- tive benefits) and quality of life (qualitative benefits) at the same time. Perfect health is assigned a value of 1, and the worst case scenario is assigned a value of 0. The value measuring various health conditions is called the utility value, and QALY is the product of years of life and the utility value. QALY and the utility value are in- dices independent of type of disease and thus give results that do not depend on the disease.
7. Decision-Making for Selecting Treatment: Difficulties and Importance
As patient characteristics and values become more diverse, so do the selections for treatment. Moreover, as pa- tients become more aware of their rights and come to have higher expectations for a good QOL even in old age, the treatment level demanded by patients in recent years continues to increase. Patients with the same findings (based on physical examinations or imaging tests) may have different personal and social backgrounds. It is no exaggeration to say that patient expectations for treatment differ among all individuals with respect to content and level. Currently, healthcare providers are requested to present treatment methods adapted to each individual patient. If conventional treatment practices may be considered “ready-made”, then current requested practices are “custom-made”. Such treatment is certainly not easy for healthcare providers. Meanwhile, whether patients are happy with the treatment they themselves selected and decide to continue depends on various factors, such as the depth of patient-doctor trust, treatment flexibility their doctor, and patience of the healthcare professional (in dealing with patient anxiety and fickleness). Even if a treatment course selection is medically appropriate, it is necessary to remember that whether patients are satisfied with the treatment and actively participate in it will depend on an extremely individual-based relationship of trust that is a separate concept from medicine.
8. Changes in the Role Demanded of Orthopedic Surgeons
As discussed above, major reforms are taking place in LSS diagnosis and treatment. The main players responsible for LSS diagnosis and treatment are orthopedic surgeons, and there is concern about whether they are capable of adequately responding to these reforms. This is because traditional orthopedic surgeons were required to provide timely responses to traumatic injury and other acute conditions. They were generally required to develop short-term treatment plans on a weekly or monthly basis. Moreover, the concept of a “cure” from the symptoms of the targeted disease was emphasized. However, with the current reforms in the concept of LSS diagnosis and treatment, the targeted diseases have become primarily degenerative diseases such as osteoporosis that are chronic illnesses. Naturally, holistic primary care is required for such diseases. In other words, “care” is emphasized. These diseases require plans for long-term treatment in units of not weeks and months, but months and years. When considering LSS treatment, irrespective of new medicines and newly developed surgical technologies, healthcare providers should be able to check the cure of the degree of relief from leg pain and numbness and improved walking ability and maintain high quality in day-to-day life (e.g. ZCQ) one and two years later as part of care. These concepts are close to those for the treatment of lifestyle diseases such as diabetes and hypertension. To respond to these new concepts in LSS diagnosis and treatment and changes in the targeted disease, orthopedic surgeons must revise traditional concepts in diagnosis and treatment by using various types of scales that enable short- to medium- and long-term care.
In order to be response to these reforms, a tool to evaluate a specific LSS patient’s profile with multiple assessment items should be developed. In addition, it is necessary to verify a cost effectiveness of lumbar spinal disorder included LSS.
9. Conclusion
The shift from evaluation by doctors to assessment based on the patient’s own perspective has occurred. A multiple assessment for LSS included symptoms, QOL, and healthcare economics. It is important that patients are satisfied with the treatment according to an individual-based relationship of trust between a patient and a physician.
Funding
No benefits or funds were received in support of this paper.
Conflict of Interests
No conflict of interests.
References
- Konno, S. and Kikuchi, S. (2004) How Should We Assess the Outcome of Patients with Spinal Cord Disorders? Spin & Spinal Cord, 17, 27-29. (in Japanese)
- Kawai, K., Harada, H., Matayoshi, H., et al. (2011) Pain Monitor Using Questionnaires. Pain Clinic, 32, 999-1006. (in Japanese)
- Iseki, M. (2011) The Assessment of Pain―The Evaluation of Pain. Practice of Pain Management, 2, 18-24. (in Japanese)
- Sekiguchi, M., Konno, S. and Kikuchi, S. (2009) Scales for Pain and Scoring Systems. Orthopaedic Surgery and Traumatology, 52, 483-490. (in Japanese)
- Keele, K.D. (1948) The Pain Chart. The Lancet, 2, 6-8. http://dx.doi.org/10.1016/S0140-6736(48)91787-5
- Scott, J. and Huskisson, E.C. (1976) Graphic Representation of Pain. Pain, 2, 175-184. http://dx.doi.org/10.1016/0304-3959(76)90113-5
- Downie, W.W., Leatham, P.A., Rhind, V.M., et al. (1978) Studies with Pain Rating Scales. Annals of Rheumatic Diseases, 37, 378-381. http://dx.doi.org/10.1136/ard.37.4.378
- Hamaguchi, S. (2011) Pain Monitor Using Language, Scales, and Behavior. Pain Clinic, 32, 989-998. (in Japanese)
- Williamson, A. and Hoggart, B. (2005) Pain: A Review of Three Commonly Used Pain Rating Scales. Journal of Clinical Nursing, 14, 798-804. http://dx.doi.org/10.1111/j.1365-2702.2005.01121.x
- Breivik, E.K., Björnsson, G.A. and Skovlund, E. (2000) A Comparison of Pain Rating Scales by Sampling from Clinical Trial Data. Clinical Journal of Pain, 16, 22-28. http://dx.doi.org/10.1097/00002508-200003000-00005
- Bennet, M. (2001) The LANSS Pain Scale: The Leeds Assessment of Neuropathic Symptoms and Signs. Pain, 92, 147-157. http://dx.doi.org/10.1016/S0304-3959(00)00482-6
- Dworkin, R.H., Turk, D.C., Farrar, J.T., et al. (2005) Core Outcome Measures for Chronic Pain Clinical Trials: IMMPACT Recommendations. Pain, 113, 9-19. http://dx.doi.org/10.1016/j.pain.2004.09.012
- Salaffi, F., Stancati, A., Silvestri, C.A., et al. (2004) Minimal Clinically Important Changes in Chronic Musculoskeletal Pain Intensity Measured on a Numerical Rating Scale. European Journal of Pain, 8, 283-291. http://dx.doi.org/10.1016/j.ejpain.2003.09.004
- Wong, D.L. and Backer, C.M. (1988) Pain in Children Comparison of Assessment Scale. Pediatric Nurse, 14, 9-17.
- Fukuhara, S., Suzukamo, Y., Bito, S., et al. (2001) Manual of SF-36 Japanese Version 1.2. Tokyo Public Health Research Foundation, Tokyo.
- Fukuhara, S. and Suzukamo, Y. (2004) Manual of SF-36v2 Japanese Version. Institute for Health Outcomes & Process Evaluation Research, Kyoto. (in Japanese)
- The EuroQol Group (1990) EuroQol: A New Facility for the Measurement of Health-Related Quality of Life. Health Policy, 16, 199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9
- Fairbank, J.C., Couper, J., Davies, J.B., et al. (1980) The Oswestry Low Back Pain Disability Questionnaire. Physiotherapy, 66, 271-273.
- Fujiwara, A., Kobayashi, N., Saiki, K., et al. (2003) Association of the Japanese Orthopaedic Association Score with the Oswestry Disability Index, Roland-Morris Disability Questionnaire, and Short-Form 36. Spine, 28, 1601-1607. http://dx.doi.org/10.1097/01.BRS.0000077510.95462.39
- Miyamoto, M. (2012) Evaluation of Low Back Pain. Monthly Book Orthopaedics, 25, 15-26. (in Japanese)
- Fukui, M., Chiba, K., Kawakami, M., et al. (2009) JOA Back Pain Evaluation Questionnaire (JOABPEQ)/JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): The Report on the Development of Revised Versions April 16, 2007. Journal of Orthopaedic Science, 14, 348-365, http://dx.doi.org/10.1007/s00776-009-1337-8
- Miyamoto, M., Fukui, M., Konno, S., et al. (2009) Development of New Disease-Specific QOL Measure for Patients with Low Back Pain: JOA Back Pain Evaluation Questionnaire (JOABPEQ). The Journal of the Japanese Society for Spine Surgery and Related Research, 20, 823-833. (in Japanese)
- Stucki, G., Daltroy, L., et al. (1996) Measurement Properties of a Self Administered Outcome Measure in Lumbar Spinal Stenosis. Spine, 21, 796-803. http://dx.doi.org/10.1097/00007632-199604010-00004
- Ikeda, S. (2009) Methods for Economic Evaluation of Health Care Technologies. THE BONE, 23, 145-150. (in Japanese)