Open Journal of Orthopedics
Vol.3 No.2(2013), Article ID:32706,5 pages DOI:10.4236/ojo.2013.32014
Autologous Tendon Grafts Used in Upper Limb Surgery
![]()
1Department of Orthopaedics, Wrightington Hospital, Wigan, UK; 2Blackpool Victoria Hospital, Blackpool, UK.
Email: avinashalva@gmail.com
Copyright © 2013 Avinash Alva et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 19th, 2013; revised May 6th, 2013; accepted May 19th, 2013
Keywords: Autologous Tendon Graft; Palmaris Longus; Plantaris; Extensor Digitorum Longus; Extensor Hallucis Longus; Flexor Carpi Radialis; Hamstrings
ABSTRACT
Tendon autografts play an important role in upper limb reconstruction and a working knowledge of tendon autograft options is essential for the surgeon. Although palmaris longus is often the first choice, other options like plantaris, extensor Hallucis longus, flexor carpi radialis are readily available. Advantages of autografts include easy availability, satisfactory biomechanical properties and the human body tends to accept its own tendons than from a donor. This review highlights the various options available and their anatomical and surgical considerations in procuring grafts for upper limb reconstructive work.
1. Introduction
Autologous tendon grafting forms an integral part of reconstructive upper limb surgery. It is utilised in restoration of tendon length, joint stability, motion and ultimately function of the limb. Allografts have been used with limited success as irradiation prior to use may result in their loss of biomechanical properties [1,2]. Moreover, potential risks of disease transmission, limited availability and additional costs have prevented its widespread use [3-5]. Synthetic materials such as nylon, carbon fibres and silicone have also been employed but they can cause an inflammatory reaction or an antigenic response leading to failure at fixation sites and deficiencies in long-term biocompatibility [3,4]. The decision in choosing a specific tendon autograft involves consideration of the anatomy of the tendon, dispensability and potential morbidity of harvesting the graft as well as the demands of the surgical reconstruction. In this article, we review the anatomy and clinical applications of tendon autografts commonly used in upper limb surgery.
2. Palmaris Longus (PL)
PL arises from the medial epicondyle of the distal humerus and adjacent intermuscular septa and lies ulnar to the flexor carpi radialis. The tendon then passes palmar to the flexor retinaculum [6] and flattens into a sheet before being incorporated into the palmar aponeurosis. The vascular supply is from the anterior ulnar recurrent artery and it is innervated by the median nerve with root values of C7 and 8. It serves as an anchor for the skin and facia of the hand and resists horizontal shearing forces in a distal direction [6]. The tendon can be identified clinically by opposing the thumb to the little finger with the wrist flexed against resistance. PL is absent in about 15% of the population [7,8]. Its absence is more common among Caucasian and Turkish populations [9]. It has also been noted that right-sided absence was more common in left-handed persons while left-sided absence was more common in right-handed persons [10]. The tendon can be harvested without risk of compromising function of the hand and wrist.
In order to harvest the tendon, a small transverse incision is made just proximal to the wrist crease to identify the distal end of the tendon. It is then retracted firmly to create tenting of the overlying skin. At the desired length, a stab incision is made right over the tendon to disconnect it proximally. The tendon is then pulled through before division at the distal end. Alternatively, a tendon stripper may be used to facilitate harvesting through a single transverse incision at the wrist crease. Firm traction is maintained on the tendon while the stripper is advanced in a back and forth rotatory fashion. The instrument is aimed at the medial epicondyle of the humerus [11]. Complications of harvesting PL include damage to the median nerve, palmar cutaneous branch of the median nerve, medial cutaneous nerve of the forearm, adjacent tendons and flexion contracture at the wrist [12].
The tendon is usually long enough for a graft of about 15 cm [13]. Occasionally there may be a double tendon or multiple insertions [13]. PL is valuable for palm-tofingertip tendon reconstructions as it is in the same field of surgery and is easily accessible. It has also been used in a variety of reconstructions, including A2 pulley, triceps, distal biceps and collateral ligaments of the elbow and metacarpophalangeal joints [14-16].
2.1. Flexor Carpi Radialis (FCR)
The muscle originates from the medial epicondyle through the common flexor tendon. It runs over a groove on the trapezium and the long tendon inserts into the base of the second and third metacarpal. In the distal portion of the tendon the radial artery lies between the FCR and the brachioradialis. It is innervated by the median nerve [17]. To harvest the tendon a 1 cm incision is made on the radial aspect of the wrist crease (Figure 1). The paratenon is incised. A tendon stripper is then passed along the proximal length of the tendon. The maximum width of the tendon harvested is usually a third of its maximum thickness. At the proximal end of the tendon a stab incision is made into 30% to 40% thickness of the tendon although some surgeons use the entire FCR without any significant problems with wrist function. It is then folded on to the stripper. The stripper is then retracted reminding oneself that the tendon rotates over thetop from the ulnar to radial direction (TROTTUR). About 10 cm long graft can be generally harvested (Figure 2). Due precautions are taken to avoid injuring the median nerve and radial artery. The graft has been used in trapeziometacarpal arthroplasty and volar beak ligament reconstruction [18].
2.2. Plantaris
Plantaris is present in over 90% of individuals [13]. It takes origin from the lateral supracondylar line of femur and the oblique popliteal ligament. The tendon then crosses obliquely between gastrocnemius and soleus and then, runs along the medial border of the tendoachilles [6]. It either inserts into the calcaneum or fuses with the tendoachilles. There are numerous variations in the long axis and insertion of the muscle [19]. It is supplied by the lateral sural, popliteal and additionally from the lateral superior genicular artery. It is innervated by the tibial nerve [6]. When present it can serve up to three palmto-fingertip grafts or one long forearm-to-fingertip graft [14] and as such it is popular for forearm-to-fingertip reconstruction or when multiple or long grafts are needed [14]. In order to harvest the tendon, a longitudinal incision is made just posterior to the medial malleolus. The tendonis identified, tagged and divided. The tendon stripper is aimed at the lateral aspect of the knee joint. Its attachments to the triceps surae may make it difficult to
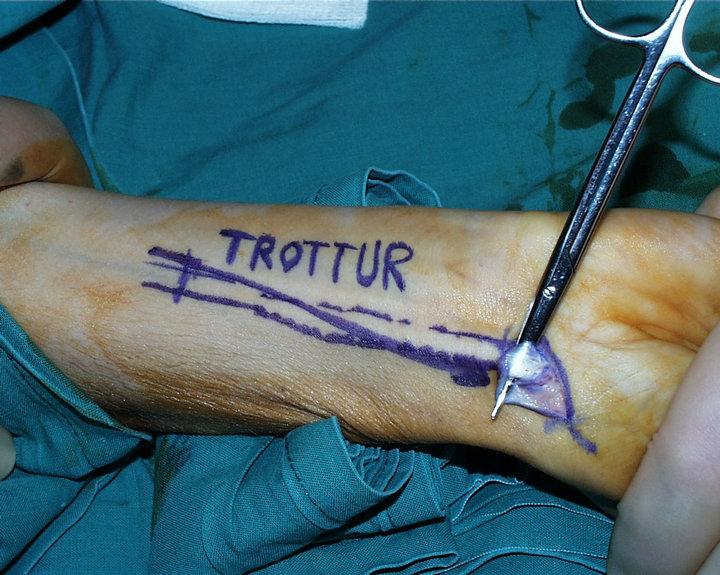
Figure 1. Incision to harvest the flexor carpi radialis.

Figure 2. Length of tendon harvested.
harvest in one length. Brand reported only a single case of lower extremity pain following 100 free plantaris tendon harvesting [15]. However compartment syndrome that was caused by a small arterial vessel laceration at the musculotendinous junction had been reported [14].
Plantaris is often used when the PL is absent [16]. Yamazaki et al reported satisfactory results from onestage flexor tendon grafting in paediatric patients using plantaris tendon [20]. Indications for its use are similar to PL [16,21-24]. Ligamentous stabilisation of distal radioulnar joint has been described using the Plantaris [24].
2.3. Extensor Digitorum Longus (EDL)
The EDL arises from the lateral condyle of the tibia, proximal three-quarters of the medial surface of the fibula, interosseous membrane and the deep fascia. It then divides into four slips to insert into the lesser toes. At the metacarpophalangeal joints MTPJ the tendons to the second, third and fourth toes are joined on the lateral side by a tendon slip of extensor digitorum brevis EDB [6]. The dorsal digital expansion thus formed also receives contribution from the lumbrical and interossei. The expansion narrows and divides into three slips which insert into the base of the middle and distal phalanges. It is innervated by the deep peroneal nerve which runs obliquely posterior to its upper half. The blood supply is derived from the anterior tibial artery and perforating branch of the peroneal artery [6]. In the foot, it is supplied by the anterior lateral malleolar artery, lateral tarsal, metatarsal plantar and digital arteries. The EDL is harvested with an incision at the level of the metatarsophalangeal joint. A tendon stripper is used to facilitate harvest. Additional incisions are made over the extensor retinaculum and at the level of disconnection of the tendon proximally. Dissection is often required proximally to identify the tendon end.
Toe extensors have been utilised in reconstructions of elbow ligaments [21,25] and flexor tendon [26] particularly when longer grafts are needed in forearm to fingertip reconstruction.
A table can summarize all the information (Table 1).
2.4. Gracilis and Semitendinosis
The semitendinosis and gracilis take origin from the ischial tuberosity and pubic symphysis respectively. They insert, along with the sartorius tendon, as the pes anserinus at the anteromedial tibia. An accessory insertion of semitendinosis is seen in 77% of knees [27]. At least seven different anatomical variations of the pes anserinus have been described in a cadaveric study who also noted atleast one to be present in 48% of specimen [28]. The common insertion of these 3 tendons is located an average of 19 mm distal and 22.5 mm medial to the apex ofthe tibial tubercle [29]. The gracilis and semitendinosus tendons are located deep to the sartorius and over the
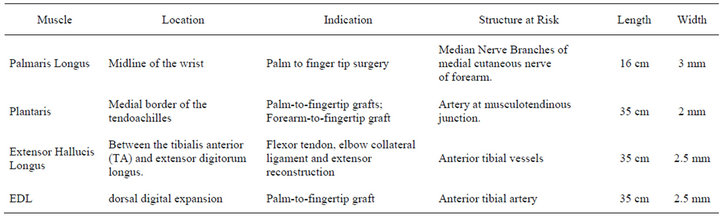
Table 1. Various autografts: Anatomy, indiations and structures at risk.
superficial medial collateral ligament [27]. The gracilis and semitendinosus tendons become distinct structures at 18 mm proximal and posteromedial to their combined insertion site [27]. The gracilis and hamstring tendons may be harvested through a vertical, transverse, or oblique incision centered about 4 cm medial to, and just distal to, the tibial tubercle [29]. A rough guide would be 3 fingerbreadths distal to the medial joint line. The subcutaneous tissue is divided in the line of the incision.
The gracilis is round whereas the semitendinosus is flatter [29]. In the upper limb they are used in reconstruction of chronic tears of distal biceps, triceps tear, medial and lateral ligament complexes in the elbow and anterior shoulder stabilization [18,30-32]. Complications of using this graft include injuries to branches of the saphenous nerve, donor site pain, medial collateral ligament injury, premature graft amputation, and temporary hamstring weakness [29].
2.5. Toe Flexors
Flexor tendons of the toes are less frequently used as graft compared to the other options already discussed, partly because of the dissection required for harvest. Recent studies have shown that toe flexor grafts heal with few adhesions but they are associated with small risk of injury to neurovascular structures [14].
3. Conclusion
A working knowledge of the various tendon autograft options should be part of the armamentarium of a reconstructive upper limb surgeon. A cadaveric study by Jakubietz et al. suggested that PL and plantaris despite being present may not be adequate for grafting hence underlining the importance of identifying alternative donor sites before embarking on surgery [33]. Other tendons which are less frequently harvested, but nonetheless are valuable, include the extensor digiti minimi and extensor carpi radialis longus. The authors prefer utilising a local graft, when available, hence limiting the surgery to a single limb. If that is not possible, the contralateral upper limb will be considered before grafts from the lower limb are employed.
REFERENCES
- T. A. Grieb, R. Y. Forng, S. Bogdansky, C. Ronholdt, B. Parks, W. N. Drohan, et al., “High-Dose Gamma Irradiation for Soft Tissue Allografts: High Margin of Safety with Biome-Chanical Integrity,” Journal of Orthopaedic Research, Vol. 24, No. 5, 2006, pp. 1011-1018. doi:10.1002/jor.20079
- O. Akkus, R. M. Belaney and P. Das, “Free Radical Scavenging Alleviates the Biomechanical Impairment of Gamma Radiation Sterilized Bone Tissue,” Journal of Orthopaedic Research, Vol. 23, No. 4, 2005, pp. 838-845. doi:10.1016/j.orthres.2005.01.007
- M. T. Cooper and C. Kaeding, “Comparison of the Hospital Cost of Autograft versus Allograft Soft-Tissue Anterior Cruciate Ligament Reconstructions,” Arthroscopy, Vol. 26, No. 11, 2010, pp. 1478-1482. doi:10.1016/j.arthro.2010.04.004
- S. H. Nagda, G. G. Altobelli, K. A. Bowdry, C. E. Brewster and S. J. Lombardo, “Cost Analysis of Outpatient Anterior Cruciate Ligament Reconstruction: Autograft versus Allograft,” Clinical Orthopaedics and Related Research, Vol. 468, No. 5, 2010, pp. 1418-1422. doi:10.1007/s11999-009-1178-y
- F. B. Oro, R. S. Sikka, B. Wolters, R. Graver, J. L. Boyd, B. Nelson, et al., “Autograft versus Allograft: An Economic Cost Comparison of Anterior Cruciate Ligament Reconstruction,” Arthroscopy, Vol. 27, No. 9, 2011, pp. 1219-1225. doi:10.1016/j.arthro.2011.04.008
- S. Standring. “Gray’s Anatomy: The Anatomical Basis of Clinical Practice,” 39th Edition, Elsevier, Amsterdam, 2008.
- S. J. Sebastin and A. Y. Lim, “Clinical Assessment of Absence of the Palmaris Longus and Its Association with Other Anatomical Anomalies—A Chinese Population Study,” ANNALS Academy of Medicine Singapore, Vol. 35, No. 4, 2006, pp. 249-253.
- S. K. Kapoor, A. Tiwari, A. Kumar, R. Bhatia, V. Tantuway and S. Kapoor, “Clinical Relevance of Palmaris Longus Agenesis: Common Anatomical Aberration,” Anatomical Science International, Vol. 83, No. 1, 2008, pp. 45-48. doi:10.1111/j.1447-073X.2007.00199.x
- S. J. Sebastin, M. E. Puhaindran, A. Y. Lim, I. J. Lim and W. H. Bee, “The Prevalence of Absence of the Palmaris Longus—A Study in a Chinese Population and a Review of the Literature,” Journal of Hand Surgery, Vol. 30, No. 5, 2005, pp. 525-527. doi:10.1016/j.jhsb.2005.05.003
- M. Eric, I. Koprivcic, N. Vucinic, R. Radic, D. Krivokuca, I. Leksan, et al., “Prevalence of the Palmaris Longus in Relation to the Hand Dominance,” Surgical and Radiologic Anatomy, Vol. 33, No. 6, 2011, pp. 481-484. doi:10.1007/s00276-010-0751-0
- M. A. Wehbe, “Tendon Graft Harvesting Techniques,” Operative Techniques in Orthopedics, Vol. 3, No. 4, 1993, pp. 293-297. doi:10.1016/S1048-6666(06)80018-2
- Y. Hattori, A. Wahegaonkar, A. Addosooki and K. Doi, “Wrist Flexion Contracture: An Unusual Complication Following Palmaris Longus Tendon Harvest,” Journal of Hand Surgery, Vol. 32, No. 6, 2007, pp. 694-696. doi:10.1016/j.jhse.2007.06.007
- S. T Canale, “Campbells Operative Orthopaedics,” 11th Edition, Mosby, St. Louis, 2011.
- S. W. Wolfe, W. C. Pederson and S. H. Kozin, “Green’s Operative Hand Surgery,” 6th Edition, Churchill Livingstone, Philadelphia, 2005.
- J. S. Taras and M. J. Fitzpatrick, “Compartment Syndrome of the Leg after Plantaris Tendon Harvest: A Case Report,” Journal of Hand Surgery, Vol. 26, No. 6, 2001, pp. 1135-1137. doi:10.1053/jhsu.2001.28942
- F. Unglaub, C. Bultmann, A. Reiter and P. Hahn, “TwoStaged Reconstruction of the Flexor Pollicis Longus Tendon,” Journal of Hand Surgery, Vol. 31, No. 4, 2006, pp. 432-435. doi:10.1016/j.jhsb.2006.02.014
- S. Standring, “Gray’s Anatomy,” In: H. Ellis, Ed., The Anatomical Basis of Clinical Practice, 39th Edition, 2005, p. 875.
- T. Quach, R. Jazayeri, O. H. Sherman and J. E. Rosen, “Distal Biceps Tendon Injuries-Current Treatment Options,” Bulletin of the NYU Hospital for Joint Diseases, Vol. 68, No. 2, 2010, pp. 103-111.
- H. Edward and B. J. A. Daseler, “The Plantaris Muscle an Anatomical Study of 750 Specimens,” The Journal of Bone & Joint Surgery, Vol. 25, No. 4, 1943, pp. 822-827.
- H. Yamazaki, H. Kato, S. Uchiyama, N. Iwasaki, H. Ishikura and A. Minami, “Long Term Results of Early Active Extension and Passive Flexion Mobilization Following One-Stage Tendon Grafting for Neglected Injuries of the Flexor Digitorum Profundus in Children,” Journal of Hand Surgery, Vol. 36, No. 4, 2011, pp. 303-307. doi:10.1177/1753193410395693
- A. M. Murthi, J. D. Keener, A. D. Armstrong and C. L. Getz, “The Recurrent Unstable Elbow: Diagnosis and Treatment,” Instructional Course Lectures, Vol. 60, 2011, pp. 215-226.
- H. Yamazaki, H. Kato, Y. Nakatsuchi, N. Murakami and Y. Hata, “Closed Rupture of the Flexor Tendons of the Little Finger Secondary to Non-Union of Fractures of the Hook of the Hamate,” Journal of Hand Surgery, Vol. 31, No. 3, 2006, pp. 337-341. doi:10.1016/j.jhsb.2005.12.015
- R. P. van Riet, B. F. Morrey, E. Ho and S. W. O’Driscoll, “Surgical Treatment of Distal Triceps Ruptures,” The Journal of Bone & Joint Surgery, Vol. 85-A, No. 10, 2003, pp. 1961-1967.
- M. R. Hausman and P. S. Birnbaum, “Interposition Elbow Arthroplasty,” Techniques in Hand and Upper Extremity Surgery, Vol. 8, No. 3, 2004, pp. 181-188. doi:10.1097/01.bth.0000137215.29223.9f
- E. Moberg, “Surgical Treatment for Absent Single-Hand Grip and Elbow Extension in Quadriplegia. Principles and Preliminary Experience,” The Journal of Bone & Joint Surgery, Vol. 57, No. 2, 1975, pp. 196-206.
- M. I. Boyer, J. W. Strickland, D. Engles, K. Sachar and F. J. Leversedge, “Flexor Tendon Repair and Rehabilitation: State of the Art in 2002,” Instructional Course Lectures, Vol. 52, 2003, pp. 137-161.
- M. J. Pagnani, J. J. Warner, S. J. O’Brien and R. F. Warren, “Anatomic Considerations in Harvesting the Semitendinosus and Gracilis Tendons and a Technique of Harvest,” The American Journal of Sports Medicine, Vol. 21, No. 4, 1993, pp. 565-571. doi:10.1177/036354659302100414
- M. Ivey and J. Prud’Homme, “Anatomic Variations of the Pes Anserinus: A Cadaver Study,” Orthopedics, Vol. 16, No. 5, 1993, pp. 601-606.
- J. R. Wittstein, J. B. Wilson and C. T. Moorman III, “Complications Related to Hamstring Tendon Harvest,” Operative Techniques in Sports Medicine, Vol. 14, No. 1, 2006, pp. 15-19.
- R. J. Sierra and S. P. Steinmann, “Repair and Reconstruction of Traumatic Deficiency of the Triceps,” Techniques in Shoulder and Elbow Surgery, Vol. 8, No. 2, 2007, pp. 1523-9896.
- J. G. Alcid, S. E. Powell and J. E. Tibone, “Revision AnTerior Capsular Shoulder Stabilization Using Hamstring Tendon Autograft and Tibialis Tendon Allograft Reinforcement: Minimum Two-Year Follow-Up,” Journal of Shoulder and Elbow Surgery, Vol. 16, No. 3, 2007, pp. 268-272. doi:10.1016/j.jse.2006.07.008
- R. P. van Riet, G. I. Bain, R. Baird and Y. W. Lim, “Simultaneous Reconstruction of Medial and Lateral Elbow Ligaments for Instability Using a Circumferential Graft,” Techniques in Hand and Upper Extremity Surgery, Vol. 10, No. 4, 2006, pp. 239-244. doi:10.1097/01.bth.0000236985.66040.8e
- M. G. Jakubietz, D. F. Jakubietz, J. G. Gruenert, R. Zahn, R. H. Meffert and R. G. Jakubietz, “Adequacy of palmaris Longus and Plantaris Tendons for Tendon Grafting,” Journal of Hand Surgery, Vol. 36, No. 4, 2011, pp. 695- 698. doi:10.1016/j.jhsa.2011.01.007

