World Journal of Cardiovascular Surgery
Vol.3 No.5(2013), Article ID:37138,3 pages DOI:10.4236/wjcs.2013.35029
Eustachian Valve Endocarditis—First Staphylococcus epidermidis Case Description
1Cardiovascular Surgery Department, Hospital Universitario de Gran Canaria Doctor Negrín, Las Palmas de Gran Canaria, Spain
2Cardiology Department, Hospital Universitario de Gran Canaria Doctor Negrín, Las Palmas de Gran Canaria, Spain
Email: erodriguezcaulo@hotmail.com
Copyright © 2013 Emiliano Andrés Rodríguez-Caulo et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received July 11, 2013; revised August 8, 2013; accepted August 22, 2013
Keywords: Endocarditis; Valves; Echocardiography
ABSTRACT
Eustachian Valve Endocarditis (EVE) has been considered an extremely rare clinical entity and only 26 adult cases have been reported in literature. Eustachian valve (EV) is an embryological remnant of the sinus venosus, redirecting oxygenated fetal blood from inferior vena cava across foramen ovale and left atrium. In adults it is considered a benign rudimentary structure and its persistence is uncommon. Only 4% of the population presents a visible and redundant EV by echocardiography. Up to 10% of infective endocarditis (IE) are right sided and occurs predominantly in patients with predisposing factors as intravenous drug abusers, permanent pacemaker wires, central venous lines, or immunologic disorders, predominantly in tricuspid valve, but with a reported incidence up to 3.3% of EVE. Vast majority of EVE are due to S. aureus in 53% - 90% cases. We strongly recommend analysing the EV when echocardiography is performed in a patient suspected of having IE, irrespective of whether vegetation in another valve is found. In this case report we describe the first EVE related to Staphylococcus epidermidis in a 35-year-old male with permanent Shaldon-catheter.
1. Introduction
Eustachian Valve Endocarditis (EVE) has been considered an extremely rare clinical entity, since 1986, when Edwards et al. [1] reported the first case description, and only 26 adult cases have been reported in literature [2].
Eustachian valve (EV) is an embryological remnant of the sinus venosus, redirecting oxygenated fetal blood from inferior vena cava across foramen ovale and left atrium. In adults it is considered a benign rudimentary structure. Right sided infective endocarditis (IE) occurs predominantly in patients with predisposing factors as intravenous drug abuse (IDA), pacemaker/defibrillator wires, permanent central venous lines or immunologic disorders, involving the tricuspid valve the vast majority of cases.
In this case report we describe the first EVE related to Staphylococcus epidermidis.
2. Case Report
A 35-year-old male with a history of hypertension, chronic kidney failure in haemodialysis treatment, mitral valve replacement 12 years ago due to rheumatic fever, and infection of a permanent right internal jugular venous access (Shaldon-catheter), was admitted in our Institution with a recent history of fever, chills and dyspnoea for the last 7 days.
On presentation he was noted to have 38.5˚C, a respiration rate of 32 breaths per minute, hypertensive 182/100, tachycardial at 122 bpm and 90% oxygen saturation. Blood analysis showed elevated white blood cell count (22.500), procalcitonin (81, reference range < 0.5 ng/ml) and CRP (235, range < 5 mg/L). An urgent transthoracic echocardiography (TTE) showed late prosthetic mitral valve endocarditis, so an urgent mitral valve rereplacement with a 25-mm Carbomedics (Sorin Group, Saluggia, Italy) mechanical valve was performed, after catheter removal and empirical antibiotic treatment institution with vancomycin, gentamicin and rifampicin. Postoperative course was stormy with mild improvement of symptoms despite antibiotic treatment, so a transoesophageal echocardiography (TEE) was performed. TEE revealed an EVE with a 10 - 12-mm vegetation (Figure 1). An intensive previous TTE examination showed the
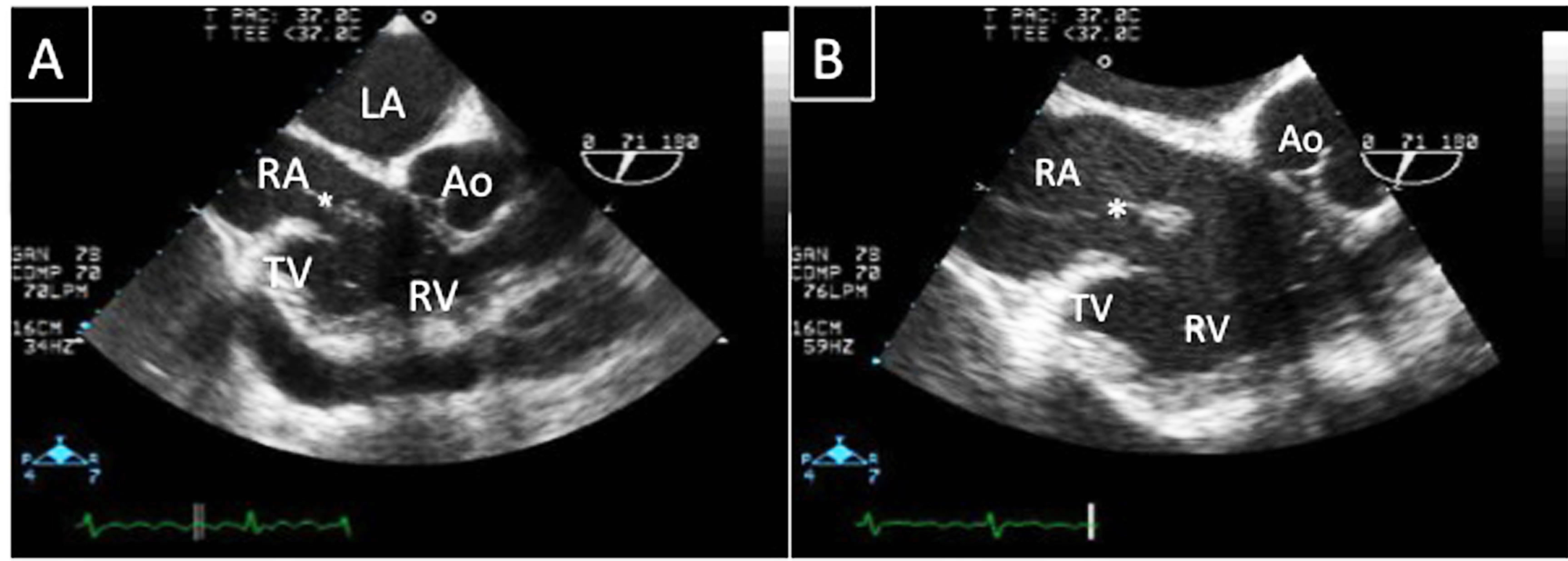
Figure 1. (A) Transoesophageal echocardiography shows a large and prominent Eustachian valve (*) with a vegetation attached to its edge. The tricuspid valve did not show any vegetation and tricuspid regurgitation was not observed; (B) A more detailed observation of the EV. Ao: aorta; LA: left atrium; RA: right atrium; RV: right ventricle; TV: tricuspid valve.
EVE in this previous study but with inadequate acoustic window for early diagnosis. In both valve and blood cultures grew S. epidermidis resistant to cloxacillin. The patient received 6 weeks of daptomicin and rifampicin and became afebrile, with a second set of blood cultures turning negative.
3. Discussion
In 1986 Edwards et al. [1] reported on the first postmortem case of EVE. Few adult cases (26) have been reported ever since [2,3]. Vast majority of cases are due to S. aureus, so to our knowledge, this is the first case describing an EVE due to S. epidermidis.
The EV is a remnant of the fetal blood circulation, less frequent in adults than children. In an adult the persistence of this valve is uncommon, and only 4% of the population present a visible and redundant EV by TTE [3].
From 5% to 10% of IE are right sided [4] and occurs predominantly in patients with predisposing factors as IDA, permanent wires, central venous lines, or immunologic disorders, predominantly in tricuspid valve, but with a reported incidence of 3.3% of EVE among all these cases [3].
Staphylococcus aureus is the most common pathogenic organism in 53% - 90% of the cases [2-4]. Other organisms have been reported so far, including Klebsiella pneumoniae, Escherichia coli, Staphylococcus hominis and Actinomyces Israelii. But this is the first case reported of an EVE due to S. epidermidis, related to a permanent central venous catheter infection and concomitant to left sided prosthetic IE.
The main issue of isolated EVE is to consider the option of surgery or not. Current European Society of Cardiology infective endocarditis guidelines [4] recommend surgery (class IIa, level of evidence C) in the presence of right heart failure secondary to associated severe tricuspid regurgitation with poor response to diuretic therapy, IE caused by organisms which are difficult to eradicate (e.g. persistent fungi), persistent bacteraemia for at least 7 days (e.g. S. aureus, P. aeruginosa) despite adequate antimicrobial therapy and tricuspid valve vegetations >20 mm which persist after recurrent pulmonary emboli with or without concomitant right heart failure. In our case, surgery was performed due to concomitant left sided IE, and EVE was eradicated with subsequent 6 week antimicrobial therapy because it was detected after surgery and the patient’s evolution was slow but positive.
TEE is not indicated as initial examination in the diagnosis of native valve IE. According to American College Cardiology/American Heart Association (ACC/ AHA) guidelines for the clinical application of echocardiography [5], when the valvular structure or pathology is well visualized by TTE, there is no indication to perform TEE. In the study of San Roman et al. [3], TEE did not add any new information to that obtained by TTE in 5 cases of EVE. They stated that both techniques offer similar information although their patients were young and had excellent acoustic windows [4]. We strongly recommend analysing the EV when echocardiography is performed in a patient suspected of having IE, irrespective of whether any vegetation in another valve is found, following San Roman et al. recommendations [2].
REFERENCES
- A. D. Edwards, M. A. Vickers and C. J. Morgan, “Infective Endocarditis Affecting the Eustachian Valve,” British Heart Journal, Vol. 56, No. 6, 1986, pp. 561-562. doi:10.1136/hrt.56.6.561
- G. Alreja and A. Lofti, “Eustachian Valve Endocarditis: Rare Case Reports and Review of Literature,” Journal of Cardiovascular Disease Research, Vol. 2, No. 3, 2011, pp. 181-185. doi:10.4103/0975-3583.85266
- J. A. San Román, I. Vilacosta, C. Sarriá, I. Garcimartín, M. J. Rollán and F. Fernández-Avilés, “Eustachian Valve Endocarditis: Is It Worth Searching for?” American Heart Journal, Vol. 142, No. 6, 2001, pp. 1037-1040.
- G. Habib, B. Hoen, P. Tornos, F. Thuny, B. Prendergast, I.Vilacosta, et al., “Guidelines on the Prevention, Diagnosis, and Treatment of Infective Endocarditis,” European Heart Journal, Vol. 30, No. 19, 2009, pp. 2369- 2413. doi:10.1093/eurheartj/ehp285
- ACC/AHA, “Guidelines for the Clinical Application of Echocardiography,” Circulation, Vol. 95, No. 6, 1997, pp. 1686-1744. doi:10.1161/01.CIR.95.6.1686

