World Journal of Cardiovascular Diseases
Vol. 2 No. 1 (2012) , Article ID: 16602 , 6 pages DOI:10.4236/wjcd.2012.21004
Diabetes and hyperlipidemia: A direct quantitative analysis ——A direct analysis of the effects of insulin resistance on lipid levels in relation to atherosclerotic coronary artery disease
![]()
1Mayo Clinic, Department of Internal Medicine, Jacksonville, Florida, USA
2Florida State University College of Medicine, Orlando, Florida, USA
Email: snipelisky.david@mayo.edu
Received 25 October 2011; revised 3 December 2011; accepted 15 December 2011
Keywords: Hyperlipidemia; Dyslipidemia; Diabetic Atherosclerosis; Diabetes; Glucose Intolerance
ABSTRACT
Introduction: Diabetes and hyperlipidemia are two major factors involved in cardiovascular disease. The medical treatment and reduction of the effects of these conditions are key modalities in the prevention of heart disease. The term diabetic dyslipidemia supports the hypothesis that insulin resistance is a potential cause of dyslipidemia. This research study is one of the few that attempts to quantify a direct relationship between insulin resistant states and dyslipidemias. Methods: Data was collected by a retrospective chart review of patients diagnosed with either glucose intolerance or diabetes and hyperlipidemia. Lipid levels and either glucose, in the glucose intolerant patients, or hemoglobin A1c values, in the diabetic patients, were recorded. The data used in our study compared changes over a 6 month period in either glucose or hemoglobin A1c with changes in total cholesterol, LDL, HDL, and triglycerides during that same time period. Results: A positive relationship was seen with both change over time in glucose and hemoglobin A1c levels with that of all components of the lipid panel. The strongest relationship was seen with comparisons involving triglycerides. Discussion: Our results show that there is a statistically significant relationship between patients with either glucose intolerance or diabetes and the different components of a lipid panel. Our research helps to reinforce the necessity to be vigilant in the treatment of both diabetes and hyperlipidemia in regard to the prevention of heart disease. It is also one of the few studies that provides statistical evidence to such relationships.
1. INTRODUCTION
Diabetes and hyperlipidemia are two major factors involved in the development of cardiovascular disease. The medical treatment and reduction of the effects of these conditions are key modalities in the prevention of heart disease [1-4]. The term diabetic dyslipidemia has been used to describe the pathophysiology surrounding the effects of insulin resistance on abnormal lipid levels. This concept states that defects in insulin action and increases in glucose can lead to higher amounts of lipoproteins in the blood. The subsequent increase in lipids, secondary to a state of glucose intolerance, adds to the progression of atherosclerosis and cardiovascular disease. As well, even slight increases in lipid levels in such diabetic patients are associated with a substantial increase in cardiovascular disease, more so than the general population. Dyslipidemia affects a diabetic patient to a greater extent than a non-diabetic patient, further reinforcing the severity of diabetic dyslipidemia. Therefore, diabetic dyslipidemia is a definite concern in the management and treatment of cardiovascular disease [1-3,5]. Very few studies to date have studied the direct relationship between changing levels of insulin resistance and dyslipidemias in a clinical setting.
The Adult Treatment Panel III, or ATP III, Guidelines discusses the importance of diabetic dyslipidemia and directly states that diabetic dyslipidemia is seen more frequently in patients with premature coronary heart disease. The ATP III also states that treatment of this condition should begin promptly and must take into account the many risk factors of this condition. It separates the risk factors into categories of either modifiable or non-modifiable and places diabetes into the category of a modifiable risk factor while also mentioning that diabetic control in relation to diabetic dyslipidemia has been shown to lead to a decrease in coronary heart disease [5].
Diabetic dyslipidemia also has a strong relationship with metabolic syndrome. Metabolic syndrome, a combination of risk factors including dyslipidemia, obesity, and insulin resistance, increases the risk of cardiovascular disease even more. Each factor of the metabolic syndrome perpetuates the other. For instance, obesity puts a patient at risk for diabetes or glucose intolerance, which further puts the patient at risk for dyslipidemias. To the same extent, a diabetic state can increase the risk of obesity, which can perpetuate and worsen a state of dyslipidemia even more. The underlying cause of metabolic syndrome is related to either the insulin resistant state of the patient or of the obesity. Much controversy exists regarding which of the two is the ultimate cause, yet, nevertheless, both are strongly involved with the pathogenesis of the resulting dyslipidemia. Metabolic syndrome is widely prevalent in patients with diabetic dyslipidemias, which ultimately puts these patients at an even greater risk for cardiovascular disease [1-3,5].
Patients with diabetes are predicted to have a 2 times - 3 times higher rate of coronary artery disease, 4 times higher rate of death during an acute myocardial infarction, and 2 times higher rate of post myocardial infarction morbidity when compared to the general population [1]. The link between diabetes and the development of cardiac disease revolves around such lipid abnormalities caused by insulin resistance, since atherogenesis is strongly linked to these abnormalities. The concept of diabetic atherosclerosis has been used to describe this observation [4].
Hypertriglyceridemia, increased low density lipoprotein (LDL), decreased high density lipoprotein (HDL), and post-prandial lipemia are said to be the four main processes that help to maintain an atherogenic environment in diabetic patients. Various biochemical pathways are involved, with most taking advantage of the dysfunction of the lipoprotein lipase enzyme seen with insulin resistance. As a result of this decreased lipoprotein lipase function, hypertriglyceridemia results. The hypertriglyceridemia subsequently creates an increase in LDL and decrease in HDL, further predisposing a patient to coronary artery disease [1,2].
Other possible mechanisms that influence the resulting dyslipidemia include insulin effects on the liver, apoprotein production, peripheral actions of insulin on other tissues such as adipose, as well as changes in regulation of enzymes responsible for maintaining adequate levels of lipoproteins in the blood. The liver is responsible for manufacturing apolipoprotein B, a major component of both very low density lipoprotein (VLDL) and LDL. In patients with resistance to insulin, an increase in lipolysis occurs, which will cause the liver to produce a greater amount of apolipoprotein B. This will ultimately create an increase in the amount of lipids in the blood. To the same effect, the actions of insulin are said to directly stimulate the liver to degrade apolipoprotein B. Therefore, in patients with insulin resistance, there will be an even higher amount of this substance in the blood secondary to the increase in production as well as the decrease in its degradation [1,2,5].
In patients with metabolic syndrome, there is further risk of dyslipidemias. For instance, the increased visceral fat seen in patients with metabolic syndrome secretes increased amounts of tumor necrosis factor alpha (TNFalpha) when compared to the general population. This increase in TNF-alpha has been shown to induce both insulin resistance, which will further increase one’s risk for obesity, as well as increase levels of triglycerides, further increasing one’s risk for dyslipidemia. Therefore, a state of metabolic syndrome compounded with a diabetic dyslipidemia ultimately creates even more difficulty in preventing and managing cardiovascular disease [1-3,5].
While using the basic science literature to form the hypothesis, our study attempts to quantify the direct relationship between various levels of insulin resistance and dyslipidemias in a clinical setting.
2. MATERIALS AND METHODS
Data was collected by a retrospective paper chart review of all active patients with diagnoses of either glucose intolerance or type 2 diabetes and any type of hyperlipidemia in a specialized lipid clinic that focuses on treating patients with hard-to-treat dyslipidemias. Fasting blood glucose levels in excess of 125 mg/dL on two consecutive measurements were used to classify patients as being diagnosed with type 2 diabetes while fasting blood glucose levels from 100 to 125 mg/dL on two consecutive measurements were used to classify patients as being glucose intolerant. Patients who were considered to have a diagnosis of a dyslipidemia had values of total cholesterol greater than 199 mg/dL, LDL greater than 159 mg/ dL, or triglycerides greater than 150 mg/dL. HDL levels were not used to determine whether or not a patient was considered to be dyslipidemic in our study.
Lipid levels and either glucose, in the glucose intolerant patient group, or hemoglobin A1c values, in the diabetic patient group, were recorded. The data points used in our analyses compared changes over a 6 month period in either glucose or hemoglobin A1c with changes in total cholesterol, LDL, HDL, and triglycerides during that same time period. A total of 34 data points from 21 glucose intolerant patients and 100 data points from 42 diabetic patients were used. If possible, multiple data points were extracted from each individual patient.
Strict exclusion criteria were followed. Data points were excluded if any changes to medication were made within a 6 month time period of that specific laboratory data point. By doing so, our study attempted to exclude any changes in laboratory values that could have been directly manipulated by changes in medication regimen. Data lacking complete medication regimens were also excluded for that same reason. If a patient’s diabetic condition became better controlled and the data points fell into the glucose intolerant or normal range those data points were excluded. To the same extent, if a glucose intolerant patient’s glucose levels fell within normal limits those data points were excluded as well. The same was applicable to changes in diagnosis in regard to the patient’s dyslipidemia. Only patients with stable diagnoses of either diabetes or glucose intolerance and hyperlipidemia were included.
The data points were subsequently analyzed by regression analyses comparing either changes in glucose, in the glucose intolerant patients, or hemoglobin A1c, in the diabetic patients, with that of all components of a lipid panel, including total cholesterol, triglyceride, LDL and HDL levels, during that same time period.
3. RESULTS
A positive relationship was seen with both change over time in glucose in the glucose intolerant patient group and change over time in hemoglobin A1c levels in the diabetic patient group with that of all components of the lipid panel except for HDL. The strongest relationship was seen with comparisons involving triglycerides. Our results take into account the R values for each comparison as well as the independent variable coefficient value generated from the regression analyses when considering strength of relationship.
Clinical characteristics of the patients used in this study are fully represented in Table 1. It can be noted that the data used in this study are comparable in respect to both the diabetic and glucose intolerant groups as well as male and female genders. Differences in medication regimens, age, and gender did not show any significant changes in our calculations.
When comparing changes in glucose and HgbA1c with changes in triglycerides, an R value of 0.722 was observed in the glucose intolerant patient group (Figure 1) and an R value of 0.787 was observed in the diabetic patient group (Figure 2).
When comparing changes in glucose and HgbA1c with changes in total cholesterol, an R value of 0.635 was observed in the glucose intolerant patient group (Figure 3) and an R value of 0.645 was observed in the diabetic patient group (Figure 4).
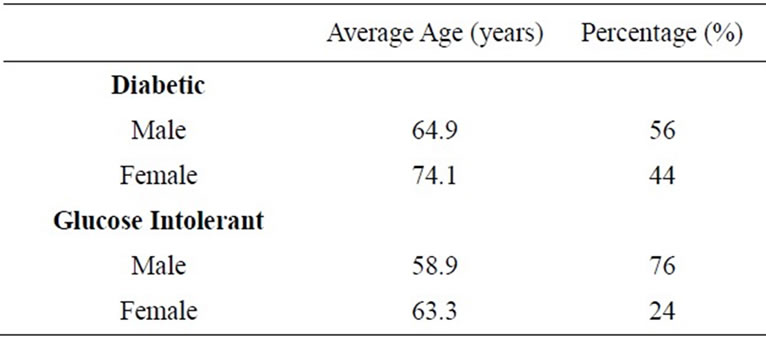
Table 1. Patient demographics in both groups.
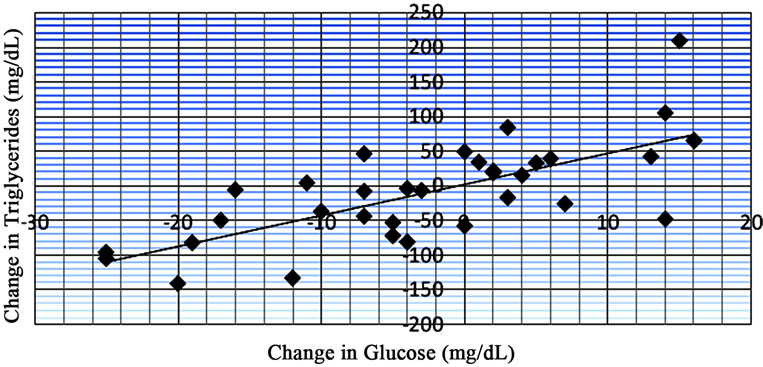
Figure 1. Data from regression analysis showing change in glucose vs change in triglycerides (n = 34) with an R value of 0.722.

Figure 2. Data from regression analysis showing change in HgbA1c vs change in triglycerides (n = 77) with an R value of 0.787. †Hemoglobin A1c.
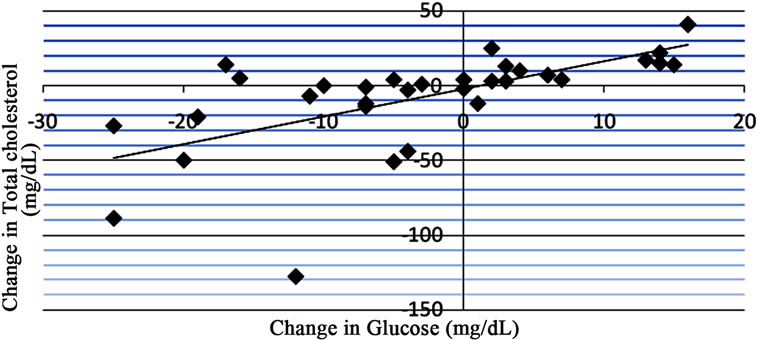
Figure 3. Data from regression analysis showing change in glucose vs change in total cholesterol (n = 33) with an R value of 0.635.
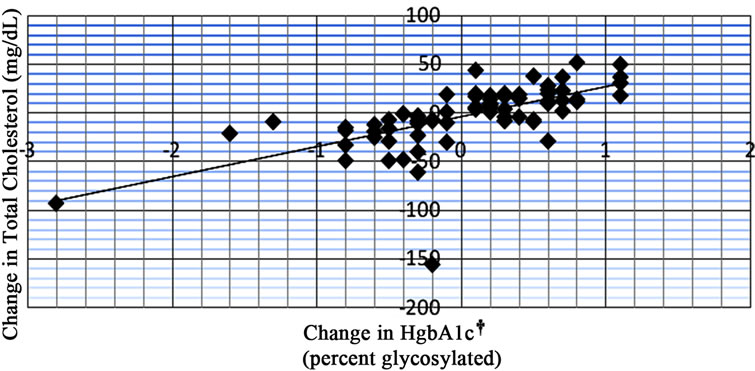
Figure 4. Data from regression analysis showing change in HgbA1c vs change in total cholesterol (n = 77) with an R value of 0.645. †Hemoglobin A1c.
When comparing changes in glucose and HgbA1c with changes in LDL, an R value of 0.484 was observed in the glucose intolerant group (Figure 5) and an R value of 0.527 was observed in the diabetic group (Figure 6).
When comparing changes in glucose and HgbA1c with changes in HDL, an R value of –0.567 was observed in the glucose intolerant patient group (Figure 7) and an R value of –0.135 was observed in the diabetic patient group (Figure 8).
Table 2 shows the predicted changes in the lipid modalities that can be expected with an increase in either glucose by 1 mg/dL or hemoglobin A1c by one percentage point. These values were calculated using the independent variable coefficient that resulted from the regression analyses. Note that direct comparisons should not
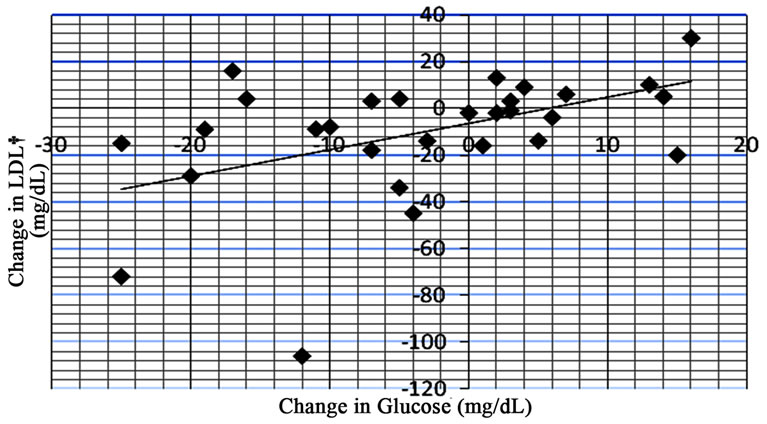
Figure 5. Data from regression analysis showing change in glucose vs change in LDL (n = 31) with an R value of 0.484.

Figure 6. Data from regression analysis showing change in HgbA1c vs change in LDL (n = 67) with an R value of 0.527. *Hemoglobin A1c; †Low density lipoprotein.
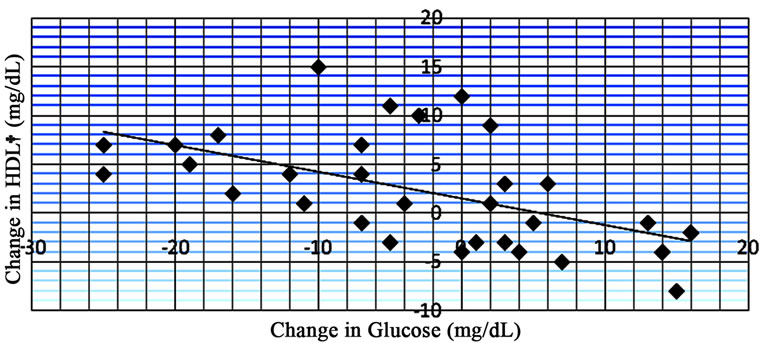
Figure 7. Data from regression analysis showing change in glucose vs change in HDL (n = 33) with an R value of –0.567. †High density lipoprotein.
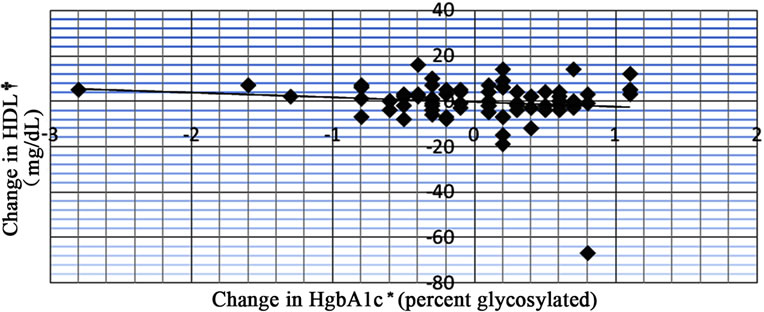
Figure 8. Data from regression analysis showing change in Hg-bA1c vs change in HDL (n = 77) with an R value of –0.135. *Hemoglobin A1c; †High density lipoprotein.
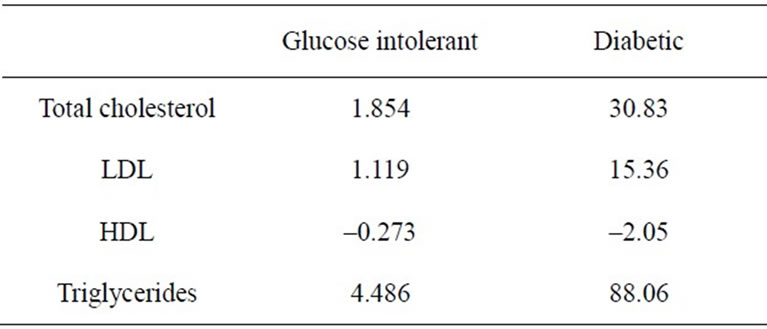
Table 2. Predicted changes in all lipid modalities in the glucose intolerant patient group with an increase in glucose by 1 mg/dL in the glucose intolerant group and an increase in hemoglobin A1c by 1 percent in the diabetic group.
be made between these two patient groups due to differrences in the scales of the independent variable (glucose vs. hemoglobin A1c).
4. DISCUSSION
Our data shows that there is a statistically significant relationship between disorders of insulin resistance and dyslipidemias, therefore supporting the existing guidelines to screen patients with glucose intolerance for the various dyslipidemias. Both patient populations in our study show statistically significant relationships between changes in glucose or hemoglobin A1c and changes in the various components of the lipid panel over the same time period. The only component that did not show statistical significance in both groups was that of HDL, yet there was a somewhat strong inverse relationship between those two variables in the glucose intolerant patient group.
Our research shows that the strongest relationship was seen with comparisons involving triglycerides in both patient groups. Both groups have R values in excess of 0.70. This strong relationship supports the basic science literature, which states that one of the first components of a lipid panel to increase is that of the triglyceride level secondary to lipoprotein lipase dysfunction. This increase in triglycerides helps to create the subsequent increases of total cholesterol, LDL, and decrease in HDL. Our study does show that increases in LDL and total cholesterol do occur, yet not to the extent of triglycerides. This can be expected considering that the triglyceride level is the most affected component and that elevations in triglyceride levels help create the increases in LDL and total cholesterol.
In regard to the total cholesterol and LDL components, our results show a strong relationship in both patient groups. This helps to reinforce the concept stating that insulin resistance does predispose a patient to hyperlipidemia.
HDL is the only component in which our data does not show strong relationships in both patient groups. Analyses of the patients in the glucose intolerant group show a somewhat strong inverse relationship between HDL and changing glucose levels. This helps to reinforce the idea that decreasing HDL is associated with insulin resistance. This, ultimately, aids in the progression of atherosclerotic coronary artery disease. Yet, the analyses involving patients in the diabetic population show a very weak relationship in regard to changing HDL levels. This relationship does not support the claim that increased levels of insulin resistance help maintain a decreased amount of HDL in the blood. According to the literature, HDL levels are affected most downstream in the aforementioned pathways [1-3]. Therefore, it can be expected that the changes in HDL will not be as strong as the other lipid components that are affected earlier. HDL levels are also one of the more difficult to control and follow over time, especially since many other external factors can manipulate a patient’s HDL level. Further research would be recommended as follow up to investigate this finding in the diabetic patient population.
Both groups have very similar R values when looking at the relationships between change in glucose or hemoglobin A1c and triglyceride, total cholesterol, and LDL levels. Such comparable results between both patient groups help to show the significance of our data. It also suggests that the concept of diabetic dyslipidemia can be applied to patients with varied levels of insulin resistance, therefore reinforcing the need to screen insulin resistant nondiabetic patients.
One interesting finding is that the patients in the glucose intolerant group had higher average levels of total cholesterol, LDL, and triglycerides when compared to the diabetic patient group. To the same extent, this group also has lower levels of HDL. It would have been predicted that such patients have lower overall values in total cholesterol, LDL, and triglycerides and higher levels of HDL, since the diabetic patients have increased levels of insulin resistance. One explanation to these findings is that patients in the diabetic group are likely to be on more stringent medication regimens. Such patients are deemed to be at a higher baseline risk for cardiovascular disease and are treated as such. As well, there are fewer patients and data points in the glucose intolerant group, which could add to a potential observational bias.
One of the study’s limitations is the limited amount of data points that were included. To avoid biases in data, our strict exclusion criteria reduced the number of data points substantially. Patients with both a diagnosis of either diabetes or glucose intolerance and hyperlipidemia with accurate medication records were only used. To the same extent, any changes in medication or gaps in data excluded patients. Even though charts of all active patients in a busy lipid clinic were reviewed, not all charts included complete records that were required for inclusion in our study, which ultimately limited our sample size.
Another limitation is the lack of information regarding lifestyle changes and other behavioral modalities that can affect both glucose intolerant disorders and hyperlipidemia. The lipid institute has information regarding appointments with its dietician, yet information about behavior and lifestyle modifications that a patient may have otherwise undertaken outside of the lipid institute was not used to determine eligibility in the study.
5. CONCLUSIONS
Our study helps to show that diabetic dyslipidemia is a true concern in regard to atherosclerotic coronary artery disease. Increasing glucose and hemoglobin A1c levels do, in fact, create an atherogenic environment. In patients with metabolic syndrome, this further compounds the problem and increases the severity. Other studies have linked diabetes to atherosclerosis by looking at patients already diagnosed with heart disease, yet our study makes the direct link between insulin resistance and dyslipidemia. It is one of the few studies that gives statistical evidence that diabetes and hyperglycemic states directly affect lipid levels.
As discussed, the ATP III Guidelines point out that diabetes is a modifiable factor when treating patients with diabetic dyslipidemia. It also states that the risk of coronary heart disease is substantially higher in diabetic patients when compared with non-diabetic patients and remarks that it is appropriate to place patients with diabetes in a separate risk category than those without [5]. Our study reinforces this concept by showing the strong relationships between those patients with insulin intolerance and the various dyslipidemias.
To that same extent, the American Heart Association considers diabetes to be one of the major controllable risk factors for cardiovascular disease [6]. Various clinical studies, including the Heart Protection Study and Collaborative Atorvastatin Diabetes Study, have shown that there is a true reduction of cardiovascular events in diabetic patients treated with statins for dyslipidemia [7,8].
Our results help to reinforce the need to be vigilant in the treatment of hyperlipidemia in patients that are hyperglycemic. Based on the results, it can be suggested that lipid disorders be routinely tested for in both diabetic and non-diabetic insulin resistant patients and that treatment should be strongly considered if lipid levels are not at goal. It should be noted that insulin resistant states in general predispose patients to dyslipidemias, yet a patient classified to be diabetic is at a much higher risk of both metabolic syndrome and dyslipidemia than a patient with glucose intolerance that has not met the classification of a true diabetic state.
To the same effect, diet and exercise should continuously be reinforced in hyperglycemic patients to help prevent the onset of such lipid disorders, as well as prevent metabolic syndrome from further complicating the problem. Patients with a family history of diabetes should also be strongly encouraged to start participating in diet and behavioral modifications in an attempt to prevent the onset of insulin resistance, which will ultimately lead to dyslipidemias. Our study also suggests that coronary artery disease is a major concern in diabetic and glucose intolerant patients, more so than the general population.
REFERENCES
- Balasubramanyam, A. (2001) Diabetic dyslipidemia. Medscape. http://www.medscape.org/viewarticle/418584
- Goldberg, I. (2001) Diabetic dyslipidemia: Causes and consequences. The Journal of Clinical Endocrinology and Metabolism, 86, 965-971. doi:10.1210/jc.86.3.965
- Spratt, K.A. (2009) Managing diabetic dyslipidemia: Aggressive approach. The Journal of the American Osteopathic Association, 109, 2-7.
- Steiner, G. (1996) The diabetes atherosclerosis intervention study (DAIS): A study conducted in cooperation with the World Health Organization. Diabetologia, 39, 1655- 1661. doi:10.1007/s001250050630
- Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report (2002). Circulation, 106, 3143- 3421.
- American Heart Association (2010) Cardiovascular disease & diabetes. http://www.heart.org/HEARTORG/Conditions/Diabetes/WhyDiabetes Matters/Cardiovascular-Disease-Diabetes_ UCM_313865_Article.jsp
- Jialal, I. and Bajaj, M. (2009) Therapy and clinical trials: Management of diabetic dyslipidemia. Current Opinion in Lipidology, 20, 85-86. doi:10.1097/MOL.0b013e32832210b0
- Farmer, A. (2007) Diabetic dyslipidemia and atherosclerosis: Evidence from clinical trials. Current Diabetes Reports, 8, 71-77. doi:10.1007/s11892-008-0013-2

