Open Journal of Gastroenterology
Vol. 2 No. 3 (2012) , Article ID: 22038 , 4 pages DOI:10.4236/ojgas.2012.2323
Stapled haemorrhoidopexy—Complications and patient satisfaction*
![]()
Department of General Surgical, Inverclyde Royal Infirmary, National Health Service Greater Glasgow and Clyde, Greenock, UK
Email: jasimshekhani@gmail.com
Received 5 April 2012; revised 21 May 2012; accepted 29 May 2012
Keywords: Haemorrhoidectomy; Haemorrhoidopexy; Anopexy
ABSTRACT
Background: Surgical haemorrhoidectomy is recognised as an effective but often painful intervention for haemorrhoids. Performed in a district hospital setting, this survey studied the success rates of stapled haemorrhoidopexy (SH) technique according to reported symptoms and patient satisfaction, post operatively. Methods: A cohort of 108 patients admitted for circular stapled procedure at Inverclyde Royal Hospital between June 2006 and December 2011 gave their consent to be interviewed over the telephone after their procedure. 101 out of the 108 patients responded. Assessment of patient satisfaction was made on the basis of pre operative symptoms, postoperative results and complications. Results: Preoperatively, all patients had Grade lll or lV haemorrhoids complicated by haemorrhage. 33% of patients reported associated pain, and 25% complained of anal leakage. Mean follow up time was 23.8 months (7 - 38 months). Overall reported complication rate was 17%, with 9% reporting short term bleeding, 4% reporting shortlived post-operative pain and 3% with recurrence of prolapsed haemorrhoids. 88% of patients were happy with results, with 87% of patients happy to recommend the procedure to others. Conclusion: Stapled anopexy is a relatively new procedure. It has been found to be a successful and well-tolerated procedure for prolapsing haemorrhoids in this district general setting. It has a low recurrence rate, low incidence of post operative pain and a high level of patient satisfaction. However, there are associated complications and it has a steep training curve.
1. INTRODUCTION
Haemorrhoids are amongst the most common anal disorders. They are engorged blood vessels (cushions of specialized sub mucosal tissue which assist the continence mechanism) covered by the lining of the anal canal that may slide down, prolapse, enlarge and bleed. It occurs especially with suspensor ligament dysfunction [1-4].
Stapled Hemorrhoidopexy (SH) was first described by an Italian surgeon, Dr. Antonio Longo, Department of Surgery, University of Palermo, in late 1990’s [5] and since then has been widely adopted worldwide. This operation involves the use of a stapled gun inserted through the anus to hold back the internal haemorrhoids and reduce the degree of prolapse by excising a circumferential strip of mucosa from the proximal anal canal. Stapled haemorrhoidopexy is usually reserved for 3rd and 4th degree haemorrhoids. It is sometimes used to treat 2nd degree haemorrhoids as well. It gives minimal pain after the operation and earlier return to work or normal activity, compared to open haemorrhoidectomy. It does not need to be performed in stages and there is no external wound. Apart from a few isolated severe complications like pelvic abscess and severe bleeding [6], the complication rates of SH are comparable to other conventional haemorrhoid (CH) operations [7-9]. A large multicentre study in Italy showed a complication rate of 15%. The commonest complications were severe pain and bleeding, at 5% and 4% respectively.
2. METHODS
This is a prospective single institutional study. Aim of the study was to check the level of satisfaction and evaluate the rate of significant complications amongst the cohort of patients undergoing SH. A proforma was used to note the main symptoms and grade of haemorrhoids preoperatively and then patients were tele-interviewed with preset questions, 6 - 12 months after SH. One hundred and eight cases of stapled haemorrhoidopexy were performed from June 2006 to June 2011. The inclusion criteria were adults 18 - 80 years, grade 3 - 4 haemorrhoids and ASA l, ll, lll. Patients with thrombosed haemorrhoids, active bleeding, and those unfit for GA were excluded. All cases were done under GA in lithotomy position. All patients received postoperative analgesia and no prophylactic antibiotics were administered. Prolene 3 - 0 was used for purse string, 3 cm proximal to dentate line and circular stapler was used to excise and staple the mucosa around the purse string. All patients were reviewed in outpatient clinic, 4 - 6 weeks after the operation. The interviewer used a simple questionnaire for all patients over the phone. The questionnaire included questions on postoperative pain, bleeding, recurrence, recommending SH to others and patient’s level of satisfaction.
3. RESULTS
One hundred and eight patients underwent 111 SHs (53 males and 48 females). Median age of the patient was 58 years (24 - 78). Data was collected from 101 patients who responded to the telephone interview. 2 patients moved from the area and 5 were not contactable directly, (Flow chart). The information’s about these 7 patients were taken from close relatives but not included in analysis. The main pre-operative features explained in Table 1.
Mean follow-up time was 23.8 months (7 - 38 months). Overall reported complication rate was 17%, with 9% reporting short term bleeding post operatively. Bleeding stopped two weeks after surgery in these 9 patients. 4% of patients had short-lived post-operative pain. Recurrent symptoms of haemorrhage and prolapse were reported by 3 patients (3%). All these 3 patients had recurrence of prolapse along with bleeding. 2 out of these 3 patients underwent a repeat procedure. One patient had symptoms of constipation and a sensation of foreign body in the rectum. This patient underwent a EUA where retained staples and an adhesion band was found. The band was excised and the staples removed, (Table 2). 88% of patients were happy with results of stapling procedure, with 87% happy to recommend the procedure to others.

Flow chart. The study was for 108 patients, three patients had re do operation for recurrences (total 111 procedures). The information collected from 101 the remaining 7 of which 5 patients un contactable and 2 moved. 101 results analysed.

Table 1. Presenting complaints.
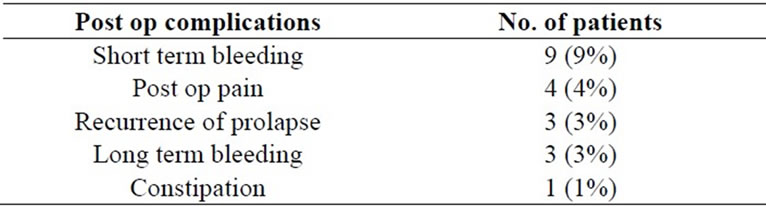
Table 2. Post op complications.
4. DISCUSSION
It has been a challenge for centuries to find the treatment that suits all patients with this benign anorectal problem. With the advances in surgical technique, stapled haemorrhoidectomy has proven to be a reasonably safe procedure. According to NICE Guidelines, stapled haemorrhoidopexy is recommended as a possible treatment for people with prolapsed internal haemorrhoids if: surgery is considered to be a suitable treatment for their condition and it is carried out with a circular stapler designed for treating haemorrhoids [10]. Meticulous technique and appropriate selection of patients may decrease the risk of adverse events associated with this procedure. Complica tions once occur, may be managed with a wide range of nonsurgical as well as surgical techniques [11].
In our study, all the stapled anopexies were done under a single surgeon, thereby adding consistency to the operative technique, reducing bias introduced by different operating surgeons and increasing reliability. Not only did we record patient’s satisfaction in terms of relief of symptoms and postoperative pain, we also asked the patients if they would recommend this procedure to other patients. Most distressing symptoms for the patients presenting with haemorrhoids was pain and prolapse. Many of the patients in the study wanted to have an operation because prolapse of haemorrhoids was causing pain and discomfort. The concept of surgery (conventional haemorrhoidectomy) to relieve pain, causing more pain was not very attractive to most patients. Patients preferred stapled anopexy as opposed to surgical haemorrhoidectomy as it claims to gives less pain in the post operative period. Reduction in postoperative pain, hospital stay and patient comfort has been approved by a number of randomised controlled trials in preference for SH over CH [12-15]. In our study, 88% of patients were satisfied, which is comparable to other studies [16-20]. Bleeding and prolapse recurring after operation was reported in only 3% of patients, results which are comparable to that of CH [21-27].
Limitations of this study are: It is a single institutional and non-randomized study. Questions asked over the telephone by the operating surgeon can introduce bias. Long-term follow up would be needed to assess patient satisfaction after a longer period of time. However the degree of patient satisfaction and the number of studies showing the same results suggests that stapled anopexy is a promising alternative.
Our study highlights that stapled anopexy is a very good choice for treatment of Grade III and Grade IV haemorrhoids. It has a very high patient satisfaction rate. However, surgeons should be trained in performing conventional haemorrhoidectomy as well, as there will be instances when one operation would be more advantageous over the other.
5. CONCLUSION
Stapled Hemorrhoidopexy has been found to be a successful and well-tolerated procedure for prolapsing haemorrhoids in the district general hospital setting. Although continued bleeding per rectum was reported in the shortterm post-operative period, recurrence rate and incidence of post-operative pain was low. The rate of satisfaction in patients treated with SH was high.
REFERENCES
- Haas, P.A., Fox, T.A., Jr. and Haas, G.P. (1984) The pathogenesis of haemorrhoids. Diseases of the Colon & Rectum, 27, 442-450. doi:10.1007/BF02555533
- Hancock, B.D. (1977) Internal sphincter and the nature of hemorrhoids. Gut, 18, 651-655. doi:10.1136/gut.18.8.651
- Thompson, W.H. (1975) The nature of hemorrhoids. British Journal of Surgery, 62, 542-552. doi:10.1002/bjs.1800620710
- Gibbons, C.P., Trowbridge, E.A., Bannister, J.J. and Read, N.W. (1986) The role of the anal cushions in maintaining continence. Lancet, 1, 886-888. doi:10.1016/S0140-6736(86)90990-6
- Longo, A. (1998) Treatment of haemorrhoidal disease by reduction of mucosa and haemorrhoidal prolapse with a circular suturing device: A new procedure. Proceedings of the 6th World Congress of Endoscopic Surgery, Rome, 3-6 June 1998, 777-784.
- Oughriss M., Yver R. and Faucheron J.L. (2005) Complications of stapled hemorrhoidectomy: A French multicentric study. Gastroentérologie Clinique et Biologique, 29, 429-433. doi:GCB-04-2005-29-4-0399-8320-101019-200513284
- Maw, A., Eu, K.W. and Seow-Choen, F. (2002) Retroperitoneal sepsis complicating stapled hemorrhoidectomy: Report of a case and review of the literature. Diseases of the Colon & Rectum, 45, 826-828. doi:10.1007/s10350-004-6304-z
- Wong, L.Y., Jiang, J.K., Chang, S.C. and Lin, J.K. (2003) Rectal perforation: A life threatening complication of stapled hemorrhoidectomy: Report of a case. Diseases of the Colon & Rectum, 46, 116-117. doi:10.1007/s10350-004-6505-5
- Pescatori, M. (2003) PPH stapled hemorrhoidectomy—A cautionary note [comment]. Diseases of the Colon & Rectum, 46, 131.
- National Institute of Health and Clinical Excellence (2007) Stapled haemorrhoidopexy for the treatment of haemorrhoids. publications.nice.org.uk/stapled-haemorrhoidopexy...haemorrhoids-ta128
- Pescatori, M. and Gagliardi, G. (2008) Postoperative complications after procedure for prolapsed hemorrhoids (PPH) and stapled transanal rectal resection (STARR) procedures. Techniques in Coloproctology, 12, 7-19. doi:10.1007/s10151-008-0391-0. PMC 2778725
- Laughlan, K., Jayne, D.G., Jackson, D., Rupprecht, F. and Ribaric, G. (2009) Stapled haemorrhoidopexy compared to Milligan-Morgan and Ferguson haemorrhoidectomy: A systematic review. International Journal of Colorectal Disease, 24, 335-344. doi:10.1007/s00384-008-0611-0
- Shao, W.J., Li, G.C., Zhang, Z.H., et al. (2008) Systematic review and meta-analysis of randomized controlled trials comparing stapled haemorrhoidopexy with conventional haemorrhoidectomy. British Journal of Surgery, 95, 147-160. doi:10.1002/bjs.6078
- Sutherland, L.M., Burchard, A.K., Matsuda, K., et al. (2002) A systematic review of stapled hemorrhoidectomy. Archives of Surgery, 137, 1395-1407. doi:10.1001/archsurg.137.12.1395
- Tjandra, J.J. and Chan, M.K. (2007) Systematic review on the procedure for prolapse and hemorrhoids (stapled hemorrhoidopexy). Diseases of the Colon & Rectum, 50, 878-892. doi:10.1007/s10350-006-0852-3
- Pavlidis, T., Papaziogas, B., Souparis, A., Patsas, A., Koutelidakis, I. and Papaziogas, T. (2002) Modern stapled longo procedure vs. conventional Milligan-Morgan hemorrhoidectomy: Randomized controlled trial. International Journal of Colorectal Disease, 17, 50-53. doi:10.1007/s003840100342
- Hill, A. (2004) Stapled haemorrhoidectomy—No pain, no gain? The New Zealand Medical Journal, 117, U1104.
- Law, W.L., Tung, H.M., Chu, K.W. and Lee, F.C. (2003) Ambulatory stapled haemorrhoidectomy: A safe and feasible surgical technique. Hong Kong Medical Journal, 9, 103-107.
- Williams, L. (2012) Hemorrhoid surgery outcome marred by long-term pain. Colorectal Disease, 14, 356-361.
- Hidalgo G.L.A., Heredia, B.A. and Sunol, S.X. (2012) Day case stapled anopexy for the treatment of haemorrhoids and rectal mucosal prolapse. Colorectal Disease, 14, 765-768. doi:10.1111/j.1463-1318.2011.02751.x
- Hetzer, F.H., Demartines, N., Handschin, A.E. and Clavien, P.A. (2002) Stapled vs excision hemorrhoidectomy: Long-term results of a prospective randomized trial. Archives of Surgery, 137, 337-340. doi:10.1001/archsurg.137.3.337
- Altomare, D.F., Rinaldi, M., Sallustio, P.L., et al. (2001) Long-term effects of stapled haemorrhoidectomy on internal anal function and sensitivity. British Journal of Surgery, 88, 1487-1491. doi:10.1046/j.0007-1323.2001.01898.x
- Guy, R.J. and Seow-Choen, F. (2003) Septic complications after treatment of haemorrhoids. British Journal of Surgery, 90, 147-156. doi:10.1002/bjs.4008
- Peng, B.C., Jayne, D.G. and Ho, Y.H. (2003) Randomized trial of rubber band ligation vs. stapled hemorrhoidectomy for prolapsed piles. Diseases of the Colon & Rectum, 46, 291-297. doi:10.1007/s10350-004-6543-z
- Mehigan, B.J., Monson, J.R.T. and Hartley J.E. (2000) Stapling procedure for haemorrhoids versus MilliganMorgan haemorrhoidectomy: Randomized controlled trial. Lancet, 355, 782-785. doi:10.1016/S0140-6736(99)08362-2
- Ganio, E., Altomare, D.F., Gabrielli, F., et al. (2001) Prospective randomized multicentre trial comparing stapled with open haemorrhoidectomy. British Journal of Surgery, 88, 669-674. doi:10.1046/j.0007-1323.2001.01772.x
- Racalbuto, A., Aliotta, I., Corsaro, G., et al. (2004) Hemorrhoidal stapler prolapsectomy vs. Milligan-Morgan hemorrhoidectomy: A long-term randomized trial. International Journal of Colorectal Disease, 19, 239-244. doi:10.1007/s00384-003-0547-3
NOTES
*We declare no conflict of interest in this study.

