Open Journal of Biophysics
Vol. 3 No. 3 (2013) , Article ID: 34502 , 3 pages DOI:10.4236/ojbiphy.2013.33023
The Fusability of Erythrocytes as a Method for Evaluating the Instability of Their Membranes
Nizhny Novgorod Scientific Research Institute of Traumatology and Ortopedics, Nizhny Novgorod, Russia
Email: *ya.sher@rambler.ru
Copyright © 2013 Yury A. Sheremet’ev et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received December 7, 2012; revised January 10, 2013; accepted January 17, 2013
Keywords: Erythrocytes; Fusability; Membrane Instability; La3+
ABSTRACT
A novel approach to the study of erythrocytes instability based on assessment fusability of their plasma membrane is presented. The fusability of erythrocytes normal blood, stored for 7 days at 4˚C, and type 2 patients with diabetes were studied. Human erythrocytes were fused by incubation with La3+ at final concentrations from 50 to 200 µM. Erythrocytes aggregates were incubated at 37˚C for 120 min. The fusability of erythrocytes was evaluated using a light microscope. It was shown that La3+ induced extensive fusion of erythrocytes after 7 days of blood storage and erythrocytes of patients with diabetes. Incubation of normal erythrocytes at 37˚C for 120 min does not induce cell fusion.
1. Introduction
Membrane fusion is ubiquitous cellular process mediating such phenomena as fertilization, exocytosis, phagocytosis, etc. [1]. Fusion can be induced by chemical agents [2]. We have previously shown that La3+ induced extensive fusion of erythrocytes with an altered ATP content [3].
It is known that the lanthanides have an extremely high affinity for phosphatidylserine [4]. It is shown that La3+ at low concentrations induces fusion phosphatidylserine vesicles [5]. Exposure of phosphatidylserine on the surface of lipid-symmetric erythrocytes may be responsible for their enhanced fusion [6]. Phosphatidylserine externalization leads to erythrocyte disintegration, or, in the presence of macrophages, to macrophage ingestion of dying erythrocytes [7,8]. It has been shown that chronic inflammation [9] and heart shock [10] greatly increase the frequency of cell fusion.
When whole blood is stored in a preservative medium, there may be morphological, biochemical, and metabolic change in the red blood cells [11].
Diabetes mellitus is the most prevalent metabolic disease and represents a serious clinical and public health problem. Increased oxidative stress and decreased life span of erythrocytes are reported in patients with type 2 diabetes. A positive correlation between lipoperoxidation and phosphatidylserine externalization in erythrocytes of patients with diabetes was found [12].
In the present study, we investigated the influence of La3+ on the fusion of erythrocytes blood storage and erythrocytes of patients with diabetes.
2. Methods and Materials
This study included 8 healthy volunteers and 5 type 2 patients with diabetes. Blood from all study subjects was obtained by venous puncture in vacuum tubes containing 3.2% sodium citrate (in а ratio 9:1) as an anticoagulant. Each sample was centrifuged (3000 × g, 20 min), and the
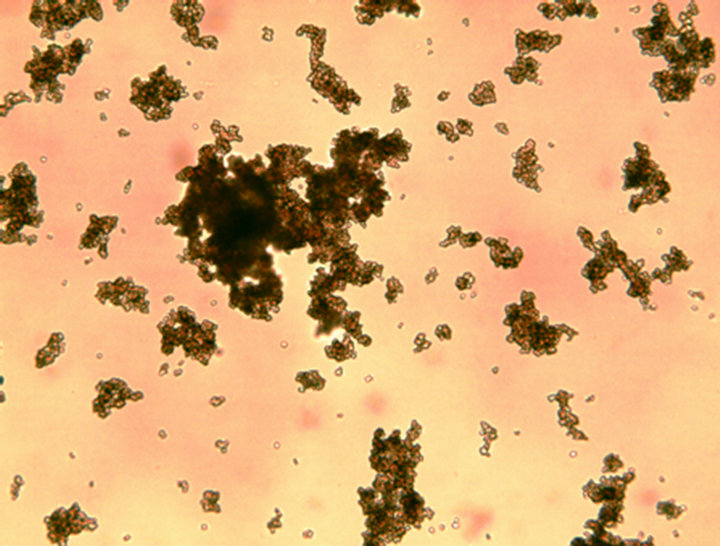
Figure 1. Influence of La3+ (150 µM) on fusion of normal of human erythrocytes. Incubation for 120 min at 37˚C × 100.
plasma and white cells were carefully removed by aspiration to avoid loss of erythrocytes. Erythrocytes were washed three times with a physiological solution (150 mM). Then 0.05 ml of washed red blood cells was resuspended in 10 ml of 10 mM Tris-HCl (pH 7.4) containing 150 mM NaCl. To 0.9 ml of the erythrocyte suspension in plastic tubes was added 0.1 ml lanthanum ion in final concentration from 50 to 200 µM and after cell aggregation incubated for 120 min at 37˚C. Fusion of red blood cells was studied in the day taking and after 7 day storage of whole blood healthy volunteers at 4˚C. Fusion of red blood cells was studied using light microscopy (Primo Star Carl Zeiss). Tris and LaCI3∙7H2O were purchased from Sigma-Aldrich (St. Louis, MO, USA).
3. Results and Discussion
The results show that La3+ induced aggregation of human
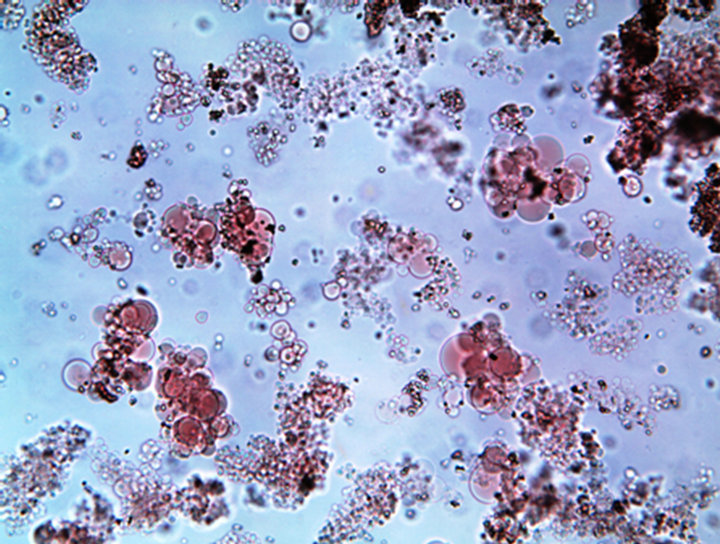
Figure 2. La3+ (150 µM)-induced fusion of human erythrocytes after 7 days blood storage. Incubation for 120 min at 37˚C × 100.
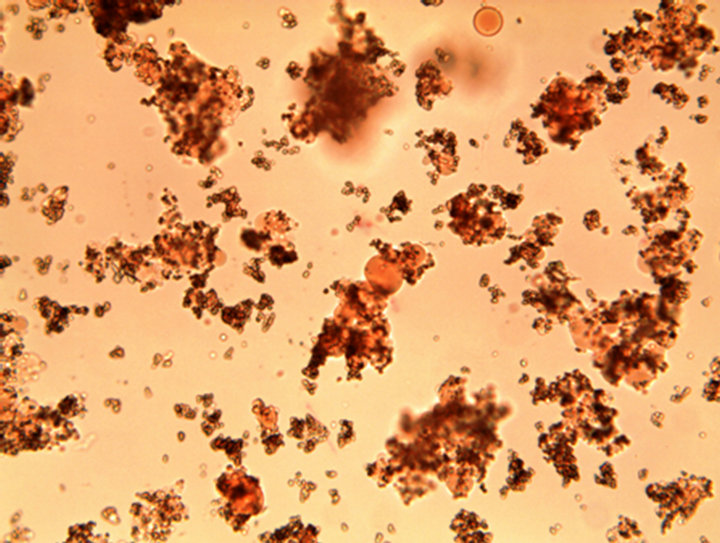
Figure 3. La3+ (150 µM)-induced fusion of erythrocytes of patients with diabetes. Incubation for 120 min at 37˚C × 100.
erythrocytes. Incubation of aggregates normal erythrocytes for 120 min at 37˚C does not cause cell fusion (association of contents cell) (Figure 1).
Figure 2 shows that La3+ induced extensive fusion of erythrocytes after 7 days of blood storage.
Figure 3 shows that La3+ induced fusion of erythrocytes of patients with diabetes.
Our results indicate that La3+ induced fusion of erythrocytes with instability their membranes.
In conclusion, the usability in evaluating instability cell membranes provides simple and powerful tool for novel approach in investigation of erythrocytes membranes.
REFERENCES
- J. A. Lucy, “The Fusion of Biological Membranes,” Nature, Vol. 227, No. 5260, 1970, pp. 815-817. doi:10.1038/227815a0
- J. A. Lucy, “Mechanisms of Chemically Induced Cell Fusion,” Membrane Fusion (Cell Surface Reviews), Vol. 5, 1978, pp. 267-304.
- Yu. A. Sheremet’ev and A. V. Sheremet’eva, “The Effect of Intracellular ATP Content on the La3+-Induced Aggregation and Fusion of Human Erythrocytes,” Biophysics, Vol.47, No.2, 2002, pp. 288-291.
- Y. A. Ermakov, K. Kamarajau, K. Sengupta and S. Sukharev, “Gadolinium Ions Block Mechanosensitive Channels by Altering the Packing and Lateral Pressure of Anionic Lipids,” Biophysical Journal, Vol. 98, No. 6, 2010, pp. 1018-1027. doi:10.1016/j.bpj.2009.11.044
- J. Bentz, O. Alford, J. Cohen and N. Duzgunes, “La3+- Induced Fusion of Phosphatidylserine Liposomes. Close Approach, Intramembrane Intermediates, and the Electrostatic Surface Potencial,” Biophysical Journal, Vol. 53, No. 4, 1988, pp. 593-607. doi:10.1016/S0006-3495(88)83138-2
- E. K. Tullius, P. Williamson and R. A. Schlegel, “Effect of Transbilayer Phospholipids Distribution on Erythrocyte Fusion,” Bioscience Reports, Vol. 9, No. 5, 1989, pp. 623-633. doi:10.1007/BF01119806
- D. Bratosin, J. Estaquier, F. Petit, D. Arnoult, B. Quatannens, J.-P. Tissier, C. Slomianny, C. Sartiaux, A. Alonso, J.-J. Huart, J. Montreuil and J. C. Amelsen, “Programmed Cell Death in Mature Erythrocytes: A Model for Investigating Death Effector Pathways Operating in the Absence of Mitochondia,” Cell Death and Differentiation, Vol. 8, No. 12, 2001, pp. 1143-1156. doi:10.1038/sj.cdd.4400946
- K. S. Lang, P. A. Lang, C. Bauer, C. Duranton, T. Wieder, S. Huber and F. Lang, “Mechanisms of Suicidal Erythrocyte Death,” Cellular Physiology and Biochemistry, Vol. 15, No. 5, 2005, pp. 195-202. doi:10.1159/000086406
- C. B. Johansson, S. Youssef, K. Koleckar, C. Holbrook, R. Doyonnas, S. Y. Colber, L. Steinman, F. M. Rossi and H. M. Blan, “Extensive Fusion of Haematopoietic Cells with Purkinje Neurons in Response to Chronic Inflammation,” Natural Cell Biology, Vol. 10, No. 5, 2008, pp. 575-583. doi:10.1038/ncb1720
- J. L. Spees, S. D. Olson, J. Ylostalo, P. J. Lynch, J. Smith, A. Perry, A. Peister , M. Y. Wang and D. J. Prockor, “Differentiation, Cell Fusion, and Nuclear Fusion during ex vivo Repair of Epithelium by Human Adult Stem Cells from Bone Marrow Stroma,” Proceedings of the National Academy of Sciences USA, Vol. 100, No. 5, 2003, pp. 23397-23402. doi:10.1073/pnas.0437997100
- G. M. D’Amici, S. Rinalducci and L. Zolla, “Proteomic Analysis of RBC Membrane Protein Degradation during Blood Storage,” Journal of Proteome Research, Vol. 6, No. 8, 2007, pp. 3242-3255. doi:10.1021/pr070179d
- J. V. Calderon-Salinas, E. G. Munos-Reyes, J. F. Guerrero-Romero, M. Rodriguez-Moran, R. L. Bracho-Riquelme, M. A. Carrera-Gracia and M. A. Quintanar-Escorza, “Eryptosis and Oxidative Damage in Type 2 Diabetic Mellitus Patients with Chronic Kidney Disease,” Molecular Cellular Biochemistry, Vol. 357, No. 1-2, 2011, pp. 171-179. doi:10.1007/s11010-011-0887-1
NOTES
*Corresponding author.

