Open Journal of Stomatology
Vol.04 No.06(2014), Article ID:47220,6 pages
10.4236/ojst.2014.46043
In Vitro Simulation of Tooth Mobility Resulting from Periodontal Attachment Loss
Yasuhiko Abe, Keisuke Nogami, Keisuke Yasuda, Yohei Okazaki, Kyou Hiasa
Department of Advanced Prosthodontics, Applied Life Sciences, Institute of Biomedical & Health Sciences, Hiroshima University, Hiroshima, Japan
Email: abey@hiroshima-u.ac.jp
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 19 April 2014; revised 31 May 2014; accepted 17 June 2014
ABSTRACT
In our previous studies, we developed the normal periodontal ligament index (nPLI) and the residual periodontal ligament index (rPLI), to estimate residual periodontal ligament support for individual teeth during treatment planning for partially edentulous patients. The purpose of the current in vitro study was to analyze tooth mobility resulting from periodontal attachment loss, and to determine the application range of both nPLI and rPLI. The association of horizontal load- displacement and conditions of attachment loss was measured in triplicate for each anatomical tooth model at 10-minute intervals, using a universal tester at a crosshead speed of 0.05 mm/min, and a load of 0.1 N. The conditions of attachment loss were: (I) 0 mm (cementoenamel junction), (II) 2 mm attachment level, and (III) two-thirds, and (IV) one-half lengths of normal attachment. Except for the upper first molar, lower lateral incisor, lower first premolar, and the lower first molar, the displacement of each tooth type was increased significantly relative to Level I (P < 0.01 or 0.05). Moreover, except for the upper first molar, the displacement of each tooth type at Level IV was significantly increased compared to Level III (P < 0.01). The results indicated that nPLI at two-thirds of normal attachment and greater, and rPLI at less than two-thirds of normal attachment should be applied, respectively.
Keywords:
Tooth Mobility, Periodontal Attachment Loss

1. Introduction
The occlusal-supporting abilities (OSAs) of remaining teeth are closely related to their physiologic and pathologic periodontal tissue support, and directly affect prosthodontic treatment planning. The support status is evaluated clinically by measuring pocket depth, attachment level, and tooth mobility, as well as by assessing intraoral radiographs [1] . The crown-to-root ratio, or periodontal tissue support, is determined and evaluated by Ante’s law (1926), which postulates that in fixed partial denture design, the total periodontal ligament area of the abutment teeth should be equal to, or greater than, that of the teeth to be replaced [2] . Furthermore, the length of the abutment tooth periodontal ligament attachment should be at least one-half to two-thirds that of its normal attachment [3] . Hence, estimation of the periodontal ligament area provides useful information for the prognosis of a tooth and it’s OSA. However, when designing fixed and removable partial dentures, assessment of the OSA of the remaining teeth is usually based on the assumption that these teeth have normal, optimal periodontal ligament support [3] . Thus, the residual periodontal ligament area is not usually assessed when determining occlusal support. Yamamoto et al. [4] demonstrated that the formulae derived for estimating the residual root surface area attached to the periodontal ligament for each tooth type can be used to assess tooth prognosis, along with other factors such as mobility, oral hygiene, degree of inflammation, and occlusion. Previously, we developed an index for estimating residual periodontal ligament support and the corresponding occlusal support according to tooth type, by applying these formulae [5] . The residual periodontal ligament index (rPLI) was derived from a formula that calculated the remaining area of periodontal attachment and the normal periodontal ligament index (nPLI) value, the latter of which assesses average residual OSA (Table 1). As a result of an accumulation of fundamental clinical data regarding the OSA of each tooth type, we analyzed the occlusal force, area, and pressure of individual maxillary and mandibular teeth, and assessed their OSAs [6] . Further, the results of our prior analyses indicated that the occlusal pressure of individual teeth can be used as an indicator of OSA. Moreover, to illustrate the applicability of nPLI and rPLI, an OSA score calculated using these indices for the remaining teeth, and corresponding to Eichner’s subclasses of partial edentulism, was charted by numerically assessing the average occlusal support [7] . The resulting OSA score, based on nPLI and rPLI, was proposed as a suitable tool for epidemiologic research on the progression of tooth loss and the survival rate of prostheses.
Considering actual clinical situations, we questioned whether the nPLI, based on the normal periodontal attachment, could be applied to assessments of the normal OSA. In other words, we speculated that rPLI should be applied in cases where it is determined that periodontal attachment loss does not possess the normal OSA. Since it is difficult to conduct this research in patients with periodontal attachment loss, we performed an in vitro simulation of tooth mobility resulting from periodontal attachment loss. Consequently, the purpose of this in vitro study was to analyze tooth mobility resulting from periodontal attachment loss, based on our previous studies [5] - [7] , and to determine the application range of both nPLI and rPLI.
Table 1. Root length [4] , normal periodontal ligament index (nPLI), and residual periodontal ligament index (rPLI) values for each tooth type [5] .
rPLI = (nPLI) × (a + bX)/100; X is the attachment level (mm). (1 ≤ X < root length). The formula (a + bX) for calculating the residual periodontal ligament area percentage was described by Yamamoto et al. [4] .
2. Materials and Methods
2.1. Experimental Model Preparation
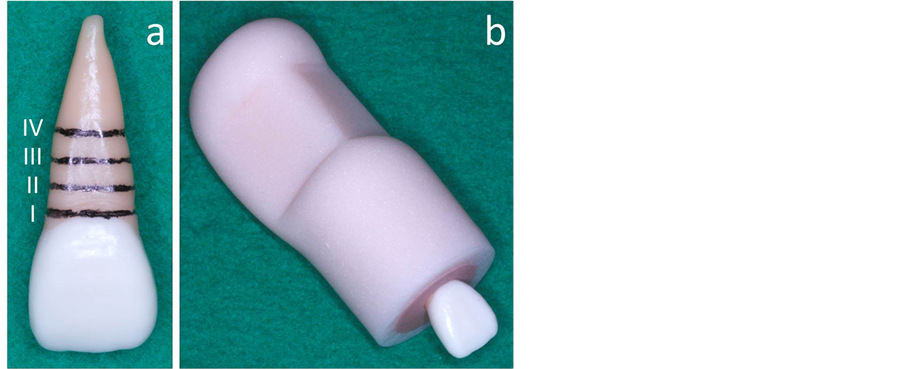
Fourteen plastic anatomical tooth models (B2-306, NISSIN Dental Products Inc., Kyoto, Japan), including seven maxillary teeth (21, 22, 23, 24, 25, 26, and 27), and seven mandibular teeth (31, 32, 33, 34, 35, 36, and 37) were used. Each model tooth implant mold had a 15-mm internal diameter, and was fabricated from an autopolymerizing polymethylmethacrylate (PMMA)-base resin (Tray Resin II, SHOFU, Kyoto, Japan). The inner surface of the mold was coated with a tray adhesive (GC, Tokyo, Japan). A hydrophilic vinyl polysiloxane impression material (Examixfine Injection Type, GC, Tokyo, Japan) was poured into the mold, and the model tooth was implanted. After polymerization of the impression material, the model tooth was removed from the mold, and the stump of the mold was trimmed and adjusted to the cementoenamel junction of the model tooth (Figure 1).
2.2. Setting of Periodontal Attachment Loss for Each Model Tooth
The experimental conditions of periodontal attachment loss were: (I) 0 mm (cementoenamel junction) and (II) 2 mm attachment levels, as well as (III) two-thirds and (IV) one-half the length of normal periodontal attachment. The attachment levels from (I) to (IV) for each model tooth are shown in Table 2 and Figure 1. For each measurement of the association of load-displacement, the stump of the mold was adjusted to each condition of periodontal attachment loss.
2.3. Measurement of the Load-Displacement Relation
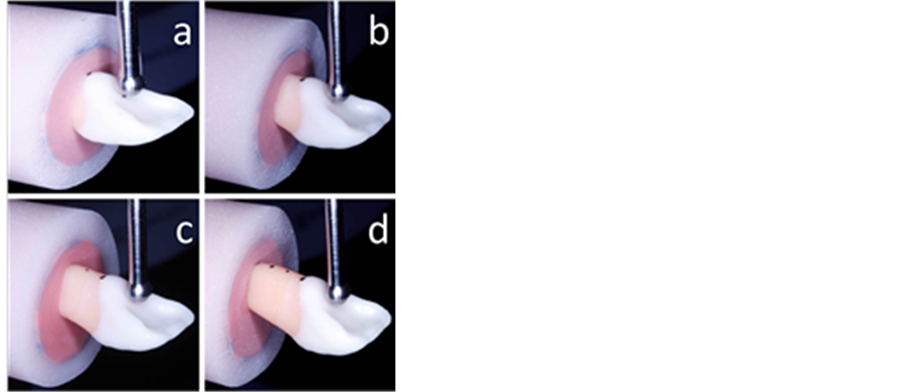
The load-displacement association of each model tooth at all conditions of periodontal attachment loss was measured in triplicate at 10-minute intervals, using a compact tabletop universal tester (EZ Test EZ-SX, SHIMADZU, Kyoto, Japan). The load point was applied with a ball stylus positioned 4 mm from the cementoenamel junction on the coronal lingual surface for maxillary teeth, and on the coronal buccal surface for mandibular teeth (Figure 2). Additionally, the load direction was perpendicular to the tooth axis. The crosshead speed was 0.05 mm/min, and the load was 0.1 N.
2.4. Statistical Analysis
The data were analyzed using one-way analysis of variance (ANOVA) and Tukey’s test for multiple comparisons. A P < 0.01 and P < 0.05 were considered statistically significant, respectively.
Figure 1. Maxillary central incisor tooth model with four lines to indicate the attachment Levels I, II, III, and IV in Table 1; the tooth model with a hydrophilic vinyl polysiloxane impression material implanted in the mold (a), and clamped by a universal tester jig (b).
Table 2. Test conditions.
*Attachment level (mm) is defined as the distance from the cementoenamel junction to the tip of the inserted probe. **III and IV are two-thirds and one-half the length of the normal periodontal ligament attachment, respectively.
Figure 2. Measurement of the load-displacement relation of the maxillary central incisor at the four attachment levels in Table 1; I (a), II (b), III (c), and IV (d). Load point applied with a ball stylus positioned 4 mm from the cementoenamel junction on a coronal lingual surface. The load direction was perpendicular to the tooth axis.
3. Results
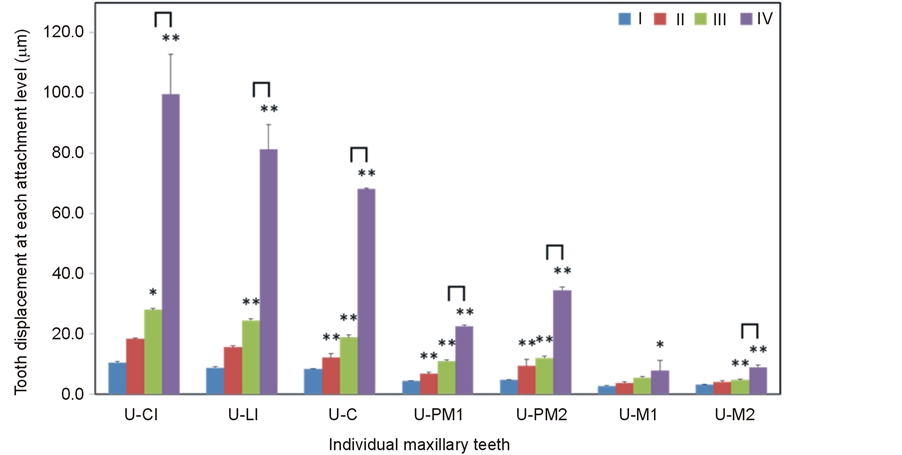
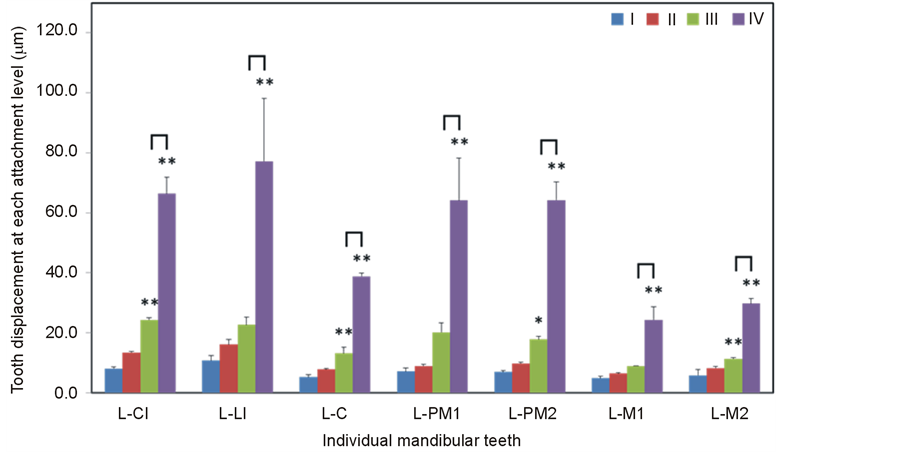
The displacements of individual maxillary and mandibular teeth at attachment levels, I, II, III, and IV are shown in Figure 3 and Figure 4, respectively. The ratios of the displacements at attachment levels, II, III, and IV compared to Level I for each tooth type are also indicated in Table 3.
Except for the upper first molar (U-M1), lower lateral incisor (L-LI), lower first premolar (L-PM1), and the lower first molar (L-M1), the displacement of each tooth type increased significantly compared to Level I (P < 0.01 or 0.05). Except for the upper first molar, the displacement of each tooth type at Level IV (one-half the normal attachment) increased progressively (P < 0.01) in relation to displacement at Level III (two-thirds the normal attachment). The ratios of the displacements at Level IV to those at Level I for upper anterior teeth (U-CI, U-LI and U-C) ranged from 8.2 to 9.6, and the ratios for lower anterior teeth (L-CI, L-LI and L-C) ranged from 7.2 to 8.3. For premolars (U-PM2, L-PM1, and L-PM2), excepting the upper first premolar
Figure 3. The displacement (μm) of individual maxillary teeth at the four attachment levels in Table 1; I, II, III, and IV. **P < 0.01 and *P < 0.05 indicate significant differences from level I. ┌┐P < 0.01 indicates significant difference between levels III and IV.
Figure 4. The displacement (μm) of individual mandibular teeth at the four attachment levels in Table 1; I, II, III, and IV. **P < 0.01 and *P < 0.05 indicate significant differences from level I. ┌┐P < 0.01 indicates significant difference between levels III and IV.
(U-PM1), the ratios ranged from 8.2 to 9.3, and the ratio for U-PM1 was 5.1, because of the double roots. The ratios for U-M1 and U-M2 with triple roots were smaller values (2.9) compare to the ratios for lower molars with double roots (5.0 and 5.1, respectively). For the displacements at all attachment levels of upper and lower premolars and molars, there was no significant difference between upper premolars, upper molars, lower premolars, or between lower molars, respectively (P > 0.05).
4. Discussion
Except for U-M1, L-LI, L-PM1, and L-M1, the displacement of each tooth type increased significantly when
Table 3. The ratio of the displacement at each attachment level to that at level I for each tooth type.
compared to Level I (P < 0.01 or 0.05). Moreover, except for U-M1, the displacement of each tooth type at Level IV increased progressively in relation to displacement at Level III (P < 0.01). Accordingly, nPLI at two-thirds of normal attachment and greater, and rPLI at two-thirds or less of normal attachment should be applied, respectively.
Progressive periodontal disease is characterized by gingival inflammation, and a gradually developing loss of connective tissue attachment and alveolar bone. Treatment of periodontal disease can result in the reestablishment of a healthy periodontium, but at a reduced height. However, the healthy, reduced height periodontium has a capacity to adapt to altered functional demands similar to normal height periodontium [8] . When the attachment loss progresses to greater than one-half of the normal attachment, the tooth mobility tends to increase at an accelerated rate. Moreover, the effect of gingival connective tissue attachment is more profound than that of the periodontal ligament because of severe alveolar bone resorption. In this study, the alveolar bone structure was not embedded in the experimental model but, since the effect of root shape on the load-displacement relation of each tooth type was evaluated, the tooth model was implanted with a sufficient thickness in the hydrophilic vinyl polysiloxane impression mold. Further, the selection of the impression material was based on previously published methods [9] .
Incisors and canines, which play a role in the shearing of foods and guide mandibular movement, respectively, as well as premolars, which are involved in crushing foods and supporting cuspid guidance, all have one or double roots. Molars, which are also involved in mashing foods, have double or triple roots. Thus, the number and attachment area of roots effects the horizontal displacement of each tooth type. The displacement of upper molars with triple roots resulted in smaller values than the other tooth types. However, the displacements of upper molars were significantly increased at Level IV compared to Level III. Therefore, the attachment loss from two-thirds to one-half of the normal attachment could significantly decrease the OSAs of all tooth types. Thus, rPLI should be applied below two-thirds of the normal attachment. In the future, the availability of OSA score [7] , based on nPLI and rPLI, will be evaluated by epidemiologic research on the progression of tooth loss and prostheses survival rate.
5. Conclusion
The objective of the current in vitro study was to analyze tooth mobility resulting from periodontal attachment, based on the results of our previous studies [5] -[7] . It was concluded that nPLI at two-thirds of normal attachment and greater, and rPLI at less than two-thirds of normal attachment should be applied, respectively.
Acknowledgments
This study was supported in part by a Grant-in-Aid for Scientific Research (no. 23592847) from the Japan Society for the Promotion of Science (JSPS), and the Ministry of Education, Culture, Sports, Science and Technology (MEXT), Japan (2011-2013). We would also like to thank Editage® for providing editorial assistance.
References
- Papapanou, P.N. and Lindhe, Y. (1997) Chapter 2 Epidemiology of Periodontal Disease. In: Lindhe, Y., Karring, T. and Lang, N.P., Eds., Clinical Periodontology and Implant Dentistry, 3rd Edition, Munksgaard, Copenhagen, 69-101.
- Johnston, J.F., Phillips, R.W. and Dykema, R.W. (1965) 1 Preoperative Study. In: Johnston, J.F., Phillips, R.W. and Dykema, R.W., Eds., Modern Practice in Crown and Bridge Prosthodontics, 2nd Edition, W. B. Saunders Company, London, 3-18.
- Lulic, M., Brӓgger, U., Lang, N.P., Zwahlen, M. and Salvi, G.E. (2007) Ante’s (1926) Law Revisited: ASystematic Review on Survival Rates and Complications of Fixed Dental Prostheses (FDPs) on Severely Reduced Periodontal Tissue Support. Clinical Oral Implants Research, 18, 63-72. http://dx.doi.org/10.1111/j.1600-0501.2007.01438.x
- Yamamoto, T., Kinoshita, Y., Tsuneishi, M., Takizawa, H., Umemura, O. and Watanabe, T. (2006) Estimation of the Remaining Periodontal Ligament from Attachment-Level Measurements. Journal of Clinical Periodontology, 33, 221-225. http://dx.doi.org/10.1111/j.1600-051X.2006.00888.x
- Abe, Y., Taji, T., Hiasa, K., Tsuga, K. and Akagawa, Y. (2010) A Proposed Index for Residual Periodontal Ligament Support. The International Journal of Prosthodontics, 23, 472-474.
- Abe, Y., Nogami, K., Mizumachi, W., Tsuka, H. and Hiasa, K. (2012) Occlusal-Supporting Ability of Individual Maxillary and Mandibular Teeth. Journal of Oral Rehabilitation, 39, 923-930. http://dx.doi.org/10.1111/joor.12008
- Abe, Y., Nogami, K., Mizumachi, W., Tsuka, H. and Hiasa, K. (2013) Proposed Score for Occlusal-Supporting Ability. Open Journal of Stomatology, 3, 230-234. http://dx.doi.org/10.4236/ojst.2013.33040
- Lindhe, Y., Nyman, S. and Ericsson, I. (1997) Chapter 8 Trauma from Occlusion. In: Lindhe, Y., Karring, T. and Lang, N.P., Eds., Clinical Periodontology and Implant Dentistry, 3rd Edition, Munksgaard, Copenhagen, 279-295.
- Brosh, T., Porat, N., Vardimon, A.D. and Pilo, R. (2011) Appropriateness of Viscoelastic Soft Materials as in Vitro Simulators of the Periodontal Ligament. Journal of Oral Rehabilitation, 38, 929-939. http://dx.doi.org/10.1111/j.1365-2842.2011.02231.x