Open Journal of Nursing
Vol.07 No.08(2017), Article ID:78795,19 pages
10.4236/ojn.2017.78069
Continuing Professional Development: Needs, Facilitators and Barriers of Registered Nurses in India in Rural and Remote Settings: Findings from a Cross Sectional Survey
Leah Macaden1*, Maryann Washington2, Annetta Smith3, Virgin Thooya2, Sumithra P. Selvam2, Nivya George2, Prem K. Mony2
1Faculty of Health Sciences & Sport, University of Stirling [Highland Campus], Centre for Health Science, Inverness, UK
2Division of Epidemiology and Population Health, St John’s Research Institute, Opposite BDA Complex, Koramangala, India
3Department of Nursing, School of Health, Social Care and Life Sciences, Centre for Health Science, University of the Highlands & Islands, Inverness, UK

Copyright © 2017 by author and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: July 18, 2017; Accepted: August 27, 2017; Published: August 30, 2017
ABSTRACT
Background: Nurses constitute a major portion of the health care workforce in India. A priority to develop pre and post registration nurse education in India has increasingly been highlighted in nursing and health policy imperatives in recent years. Nurses are often the only health care professionals in primary and secondary care within rural and remote healthcare settings in India. They are confronted with the dual challenge of resource constraints and rapidly changing disease profile with little or no access to continuing professional development. Objectives: 1) To identify key continuing professional development priorities of registered nurses working in remote and rural health care settings in India. 2) To identify barriers and facilitators to continuing professional development as perceived by registered nurses working in these settings. 3) To identify preferred modes of continuing professional development by registered nurses working in remote and rural health care settings in India. Design: Quantitative Design. Setting: Two large health care facilities in remote and rural parts of India. Participants: Registered Nurses working in two large not for profit health care organisations participated in the study. Nursing assistants and student nurses were excluded from the study. 368 participants consented to participate in the survey and 271 (73.6%) participants completed the survey. Methods: A questionnaire based cross sectional survey was undertaken as part of the Continuing Professional Development needs assessment among registered nurses working in rural and remote settings. Results: Continuing Professional Development priorities included training on clinical competencies focussed on managing emergency situations related to non-communicable diseases [50%], managerial competencies related to ethical dilemmas [60%] such as support for families with financial difficulties accessing health care [17.8%], women undergoing abortions [14.6%], or those with HIV infection [12.9%]. Preferred modes for Continuing Professional Development included conference attendance [54%], skills training [48%] and in-house training [32%]. Key facilitators for Continuing Professional Development included, professional development [77%], personal interest [42%], opportunities for professional engagement with colleagues [39%], the need to reduce knowledge and skill gap [36%] and career progression [28%]. Geographic distance [59%], low staffing levels [51%], cost [43%], domestic responsibilities [40%], and work commitments [39%] were reported as key barriers to Continuing Professional Development. Conclusions: The findings from this survey, the first of its kind in India, provides evidence on priorities, barriers and facilitators for continuing professional development of registered nurses working in rural and remote settings in India.
Keywords:
Continuing Professional Development, Registered Nurses, Remote, Rural, India, Survey, Questionnaire

1. Introduction
Nurses constitute a major portion [38%] of human resources within the healthcare system in India [1] . A priority to develop nurse education in India is increasingly highlighted in nursing and health policy imperatives in recent years [2] . Nurses in India face challenges that can be viewed within the global context, with shared solutions to problems becoming increasingly relevant. Demographic transition, the looming non-communicable disease [NCD] epidemic in India, national health priorities such as reduction in child and infant mortality yet to be achieved, the delay in the improvement of maternal health of the Millennium Development Goals [MDG] [3] and India becoming a recent signatory to the sustainable development goals all signpost an imminent changing role for nurses [3] [4] . Given the paucity India has on health care outcomes that are strongly influenced by political-socio-economic factors, gender, education and geography and inequalities in health services [4] , it is vital that relevant Continuing Professional Development [CPD] programs for nurses are developed to help mitigate some of the challenges to effective healthcare delivery.
“Continuing professional development (CPD) helps health professionals to maintain, improve and broaden their knowledge, expertise and competence” [5] . A recent needs assessment of preparedness of facility and personnel for management of emergency obstetric and new born care in public and private health settings in northern Karnataka revealed that staff nurses had the most significant knowledge gaps [6] . These gaps raise major concern since nurses are often the first point of contact or only professional contact for populations in remote and rural parts of India.
The development of relevant and co-produced continuing educational programmes for health care professionals is vital through engagement with related stakeholders [7] . Lack of consistent and structured nurse education at pre- and post-registration levels, poor access to a contemporary and robust evidence base, lack of standardised/accredited training programmes and protocols to acquire and evaluate skills have all been highlighted as key reasons for poor quality of care delivery [7] [8] in India. Given that knowledge gained through basic education has a half-life of 2.5 years [9] , it is important that CPD training programmes that are both contextually relevant, and accessible [10] [11] are developed creatively.
Recruiting highly qualified health care professionals to rural, remote, and underserved areas in India is very challenging [2] . Because of the shortage of doctors in these settings, there is an expectation that nurses substitute for this deficiency and provide the required care [12] [13] [14] . It is therefore important that nurses, who choose to work in such settings have access to CPD programmes that regularly update both knowledge and clinical skills required to initiate standard management, recognize complications early, provide initial treatment and make appropriate and prompt referrals. Nurses in these settings also play key roles in health promotion and prevention of illnesses but this role might require strengthening. Planning CPD programs that are contextualised to local and national needs with robust quality, relevance and accessibility to facilitate change in professional practice is imperative for nurses in these settings, so that they can contribute to the health care outcomes of the communities they serve [2] [15] . Additionally, the professional development and career progression needs of nurses need to be considered when developing CPD programs [16] , as nurses will also assume managerial roles alongside their clinical responsibilities in clinical or public health settings.
The Indian Nursing Council [INC] has recently made CPD mandatory towards the renewal of professional registration and has stipulated a minimum of 30 credit hours per year or 150 hours of CPD related activities over 5 years [17] . It is therefore timely and appropriate to explore the CPD needs of nurses working in remote and rural settings given the current lack of structure, and the paucity of literature in this area through a formal needs assessment to inform relevant program design and delivery. Additionally a co-produced CPD strategy developed with nurses and stakeholders working in remote and rural settings would help robustly validate content and relevance of CPD for nurses [18] .
This paper aims to describe findings from a formal needs assessment that was undertaken to explore the CPD needs of nurses working in two not for profit large health care organisations in remote and rural India.
2. Methods
Aims:
1) To identify key CPD priorities of registered nurses working in remote and rural health care settings in India.
2) To identify barriers and facilitators to CPD as perceived by registered nurses working in these settings.
3) To identify preferred modes of delivery for CPD by registered nurses working in remote and rural health care settings in India.
Design: A cross sectional questionnaire based survey.
Setting: Two large health care networks-the Catholic Health Association of India [CHAI] and the Emmanuel Hospital Association [EHA] that are largely operational in remote and rural parts of India were identified for the needs assessment. The CHAI network has a base of 3841 affiliated hospitals and health centres across India with over 25,000 nurses employed [19] . Emmanuel Hospital Association [EHA] is a large, non-profit provider of health care in India, with a network of 20 hospitals and two community health projects mostly located in rural and remote settings across 12 states of India. The EHA employs close to 910 [34% of total health care workers] nurses [20] . Both organisations responded positively and assigned designated coordinators to assist with data collection for the survey.
Sample size: Due to the paucity of literature on CPD needs of nurses, the sample size computed to estimate a proportion of 0.8 with 10% precision and 95% confidence interval was 96.
Sample selection: Participants were purposively chosen using the criteria below:
1) Inclusion Criteria
a) All nurses [Staff nurses and Charge Nurses] working in selected hospitals within CHAI/EHA network
b) Nurses who were available at the time of the data collection
c) Nurses who consented to participate in the study
2) Exclusion Criteria
a) Nursing Assistants/Nursing Auxiliaries
b) Multipurpose Health workers
c) Nursing students
2.1. Recruitment of Participants
The administrative heads and study coordinators from both organisations were contacted by telephone or email and briefed about the purpose of the study. A total of 183 questionnaires to CHAI and 185 to EHA were distributed via email or by post and were based on the number of hospital beds, nurses employed and the sample size calculation. The coordinators from both organisations were involved in recruiting study participants based on the inclusion criteria, obtaining informed consent and the distribution and collection of completed questionnaires. Informed consent was obtained from the participants and the questionnaires did not contain personal identifiable information except for the name of the organisation participants worked for to ensure confidentiality of the data.
Questionnaire Design: A three part questionnaire was designed in April 2015 by the project team based on literature review and professional expertise. Content validity was ensured by subject experts and a pilot was conducted with 10 participants to ensure feasibility, validity and reliability. No changes were made to the questionnaire following the pilot. The first section contained baseline information and demographic data such as type of health care facility, designation, area of practice, qualification, and work experience. The second section had 27 items related to clinical and managerial competencies with sub sections to most items. Participants were expected to self-assess their level of competence on a 5 point Likert scale with 1 being very confident, 2-confident, 3-confident with support, 4-lack of confidence, and 5-not relevant to the area of practice along with examples of clinical situations they most commonly faced if they had assessed their level of competence between 1 - 4 on the scale. For example, item 1a on the questionnaire was “Recognizing an acute clinical emergency” and 1b on the questionnaire was “Specify the commonest emergency situation you face in practice”.
The third section of the survey consisted of 16 items to ascertain participants’ preferred mode and type of CPD, barriers and facilitators to CPD. In order to understand what would be the most appropriate mode of CPD, three different questions were asked on the type of CPD attended in the recent past, five most preferred modes of CPD and the mode of CPD delivery they perceived as most important. The questionnaire was piloted in May 2015 at one rural health centre.
Data collection and organisation: A total of 183 questionnaires were distributed either via email or postal mail to 89 health care facilities from CHAI in two phases (between June and October 2015), and 185 questionnaires to 21 health care facilities within the EHA. The response rate from the two networks was 65% [120/183] and 82% [151/185] respectively; with an overall response rate of 74% [271/368]. Data from a total of 112 questionnaires [61%] from CHAI and 135 [73%] from EHA were used for analysis, accounting for attrition of only 24 [9%] since participants did not meet the inclusion criteria.
The overall clinical competencies were categorised as clinical competencies in acute medical emergencies, and non-communicable diseases [NCDs]; managerial competencies in Quality Assurance [QA], Human Resources [HR] and communication.
2.2. Data Analysis
For analysis, scores were reversed such that very confident was assigned 4, confident was 3, confident with support was 2 and lack of confidence was 1. Scores were obtained by the aggregate of the self-assessed rating of participants to items under each theme. Higher scores on the level of confidence reflected increased levels of self-assessed competence. Categories such as clinical competencies and managerial competencies were formed by summing up related items as appropriate.
Competencies where more than 70% of participants reported confidence were not considered as a CPD priority for training. CPD needs were identified as a priority only if more than 30% of participants reported low levels of confidence with any particular competency.
Descriptive statistics were reported using number and percentages for the categorical variables and the continuous variables were reported using mean ± SD and median [Q1, Q3]. Assumption of normality was assessed using Q-Q plot. Clinical competencies, managerial competencies and their domain scores were compared between baseline variables such as type of institution [CHAI/EHA], designation of nurses [manager/staff], size of health care facilities in terms of number of hospital beds [<50, 51 - 100, >100] and years of experience [<1, 1 - 5, >5] using independent t test/Mann Whitney u test/One way ANOVA/Kruskal Wallis test as appropriate. Chi-square test was used to test the association between study variables that were categorical. All statistical analyses were done using SPSS 23 and p value less than 0.05 was considered statistically significant.
Institution Ethics Committee approval: Ethics approval for the project was obtained from the Institutional Ethics Committee [IEC] of St John’s Medical College [IEC Ref No. 156/2015 dated 22 June 2015], Bangalore.
3. Results
Participant Characteristics: From among the 247 participants, 217 (88%) of them were staff nurses and women. Nearly two third of the participants [62%] had a diploma in nursing and midwifery, 30% of them had a Bachelor’s degree and 17.7% had a Master’s degree. The overall median years of experience was 3.5 years.
Participants from CHAI & EHA were compared for baseline variables. They differed significantly in that the number of male nurses were more [p < 0.001] in EHA [18%] compared to CHAI [2%]; and more nurses from EHA were younger than nurses from CHAI [p < 0.001]. There were no other statistically significant differences.
Clinical Competencies: Based on the participants’ responses [Table 1], CPD priorities focused on the following topics: managing NCDs [50%], managing patients who receive “bad news” [49%], interpreting diagnostics and blood tests [43%], performing health promotional activities [38%], managing acute medical emergencies and performing a comprehensive assessment towards a plan of action [36%], participating in a case review [36%], and knowledge on medications [33%].
The commonest medical emergencies faced by nurses included NCDs, where cardiac problems were most commonly reported [48%] followed by respiratory [26%], convulsions [17%], diabetes [9%]; obstetric emergencies [28%]
Table 1. Proportion of nurses with self-assessed competence in managing clinical scenarios.
such as postpartum haemorrhage and hypertensive disorders of pregnancy. Among those who reported [n = 81] the need for CPD training to manage NCD emergencies, managing cardiac [40%] and neurological [35%] emergencies were mostly cited. Similarly 58% of participants reported that NCDs were the commonest medical conditions seen in their daily practice whilst 23% reported infectious diseases such as HIV, diarrhoea, malaria, tuberculosis or typhoid. The need for training around life style or health behaviour change related to diet [24%], smoking avoidance [11%], exercise [10%], personal hygiene [9%], and avoiding alcohol [8%] were also reported.
Self-assessed competency scores were not significantly different between any of the baseline variables except for the number of hospital beds [Table 2]. Nurses who participated from hospitals with less than 50 beds had lower self-assessed competency scores in their overall clinical competency score, management of acute clinical emergency and management of NCD scores than those from hospitals with >50 beds.
Managerial Competencies: CPD priorities for the following managerial competencies [Table 3] were identified by participants: managing ethical issues [60%], preparing a project plan [57%], initiating innovation in the area of practice [54%], conducting a clinical audit [51%], assessing and managing staff stress [47%], contributing to policies [45%], managing conflict within nursing team [43%], performance appraisal [39%] and multitasking [32%]. Participants also reported a range of ethical dilemmas in daily practice which included providing support for families with financial difficulties to access health care [17.8%],
(a)*Totals do not tally because of missing values on designation and gender.
(b)women undergoing abortions [14.6%] and those with HIV infection [12.9%].
Table 2. Comparison of self-assessed clinical competencies scores based on selected baseline variables.
Participants from both healthcare networks did not differ in their self-assessed
Table 3. Self-assessed managerial competencies of nurses.
level of confidence on managerial competencies [Table 4]. Understandably, Charge Nurses scored statistically significantly better on overall managerial competency [p = 0.021], QA [p = 0.030] and HR [p = 0.012] than staff nurses. Nurses practising in a larger hospital [>50 beds] had better overall managerial [p = 0.006] and HR [p < 0.001] competencies as did nurses with more than 5 years of clinical experience with overall managerial [p = 0.012] and HR [p = 0.009] competencies. In addition, participants who had a graduate or post graduate nursing degree rather than a diploma had higher managerial competency scores [p < 0.02].
Preferred modes of CPD Delivery: 58% (n=143) of participants reported that they had attended a CPD programme in the past 12 months. Key drivers to attending CPD training [Figure 1] were to update knowledge [75%], providing high quality care [68%], increase competence [65%], professional development [45%], and be more confident in providing care for patients [41%]. 75% of the participants perceived that the quality of CPD programmes must be monitored by professional regulatory bodies such as the Indian/State Nursing Councils, whilst [41%] perceived that nursing faculty in academic institutions, the Government [34%] and employers [32%] must be accountable for the quality of CPD delivered.
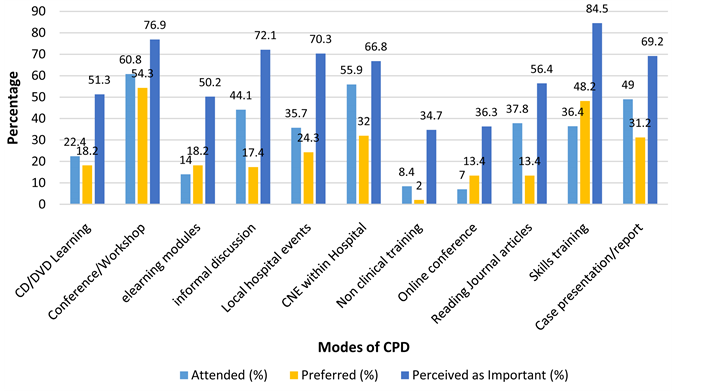
The five most common modes of CPD training [Figure 2] attended by nurses included conferences [61%], in house training [56%], case report/presentations [49%], informal professional discussions [44%] and reading journal articles [38%]. The 5 most preferred modes of CPD included conferences [54%], skills training [48%], in house training [32%], case presentation/report [31%] and local hospital events [24%]. The modes of CPD training perceived as important by
Table 4. Managerial competency scores based on selected baseline variables.
*Totals do not tally because of missing values for designation, gender, and number of hospital beds.
participants included skills training [85%], conference/workshops [77%], informal discussions [72%], local hospital events [70%], and case presentation/report [69%].
Facilitators and barriers of CPD: The 5 key facilitators identified [Figure 3] were professional development [77%], personal interest [42%], and opportunities for professional engagement with colleagues [39%], the need to reduce knowledge and skill gap [36%] and career progression [28%]. Nearly two thirds
Figure 1. Key drivers to CPD [n = 247].
Figure 2. Modes of CPD [n = 247].
of the participants preferred CPD to be both within and outside their organisation [61%] with access to study days [79%] or short term study leave [66%] to attend CPD training.
Key barriers to attending CPD training [Figure 4] included geographic distance [59%], low staffing levels [51%], cost [43%], domestic responsibilities [40%], and work commitments [39%].
4. Discussion
Empowering nurses with knowledge and competencies to be able to provide relevant and safe health care is an imminent need particularly in rural and remote
Figure 3. Facilitators of CPD [n = 247].
Figure 4. Barriers to CPD [n = 247].
settings in India, where resource constraints are acute. One way this can be best achieved is through regular CPD training since knowledge and skills gained whilst training to be a nurse could be redundant in less than 5 years [9] given the complexities of health care needs and changing demographic profile of the country.
4.1. CPD for Clinical and Managerial Competency Building
Nurses from the two health care networks that operate primarily in remote and rural India, reported that their clinical competencies require strengthening in two main areas: 1) management of acute and long term NCDs; 2) obstetric and new born emergencies. Evidence suggests that there is a lack of preparedness in dealing with obstetric and new-born emergencies by health care providers, particularly nurses in some high priority districts of the country [6] .
Findings from the survey, also reflect the global situation where NCDs are noted to be responsible for two-thirds of all deaths in 2011, up from 60% in 2000 that include cardiovascular disease, cancers, diabetes and chronic lung diseases [19] [20] . Nurses in this study indicated the need to strengthen their ability to provide health promotion activities relevant to NCDs. This is an important finding as several of the risk factors for NCDs could be modified with concerted efforts [21] . The rapid “health transition” globally and in India and the double burden of communicable and NCDs calls for a more dynamic nursing role both in primary and secondary care in remote and rural health care settings [19] [20] [21] . It is therefore necessary for CPD training programmes to have a more intense focus on prevention than a skewed emphasis on high tech medical environment with mounting costs for treatment for NCDs [22] .
CPD programs thus need to focus on the global action plan for the prevention and control of NCDs targeting health promotion on the four shared behavioural risk factors that include tobacco use, unhealthy diet, physical activity and alcohol abuse [20] [23] [24] . Given the strategic location of the nurses in this study, and the acute shortage of health care professionals where they work, enhancing their capability to relate to the contextual influences on the health illness continuum and health seeking behaviours of people at risk for NCDs could possibly influence the health outcomes of the community and the country at large. This focus would be in line with the voluntary global targets of 25% reduction in risk of premature mortality from NCDs, a 10% relative reduction in prevalence of insufficient physical activity, and a halt in the rise of diabetes and obesity [20] [24] [25] .
Nurses in this survey have clearly reported their preferred mode of CPD is through skills training. Skills to identify obstetric and new born emergencies, initiate immediate treatment and make prompt referrals could be key to improving maternal and new born outcomes in these settings [9] . This could be done by emergency drills or simulations to evoke a coordinated team response [9] [26] . It is also important to take cognisance of the fact that with increasing years of experience, nurses reported lower levels of clinical competence [p < 0.01]. This might imply a need for CPD programmes to target relevant clinical competencies for experienced nurses.
Alongside clinical competencies, knowledge of Quality Improvement [QI], performance appraisal, clinical audits and conflict management were identified as some key managerial competencies for development. Paradoxically, in this survey, Charge Nurses with management responsibilities scored lower for competencies around QI and communication compared to those nurses who only had clinical responsibilities [p > 0.05]. It may be that some nurses in this survey achieved managerial positions through time served and were not recipients of formal management training. Participants with either a graduate or post graduate qualification reported to be managerially more competent than those with a diploma, possibly due to management training in their nursing curriculum. However, attempts to strengthen both clinical and managerial competencies through CPD must be carefully balanced based on one’s clinical and or management roles.
4.2. Facilitators and Barriers to Attending CPD
CPD programs are critical to enhance the quality and safety of care provided by nurses in addition to promoting job satisfaction and staff morale [7] [26] . Various reasons are reported for CPD attendance including, job satisfaction, staff morale and patient safety [9] , performance appraisal or personal development, career and performance improvement [4] . These findings suggest that both personal/career development and practice improvement feature significantly. Nurses in this survey similarly reported that they attended CPD training largely for their professional development needs and their personal interest, and also interestingly as an opportunity for socialising. Nurses working in remote and rural areas can often feel isolated from their fellow professionals and it important to recognise this factor while developing CPD training opportunities.
Barriers to attending CPD training mostly included personal reasons such as domestic responsibilities, distance, cost and professional reasons such as work commitment, staff shortage and lack of information. Similar barriers to CPD attendance have been found elsewhere; including, lack of time and finance, access to CPD [4] , difficulty balancing work, continuing education, and home life [18] [27] . Therefore, to maximise participation in CPD, it is important that an environment is created for nurses to be able to participate interactively taking into account nurses’ professional, personal and social needs. This approach is borne through evidence and studies have shown that strong organisational support, such as paid study time, strong leadership and a positive attitude to CPD from both management and peers facilitates effective learning [12] [13] .
Too often, the ambiguity, challenges and complexities faced by nurses in the acute care practice environment are not addressed by theoretical learning [28] . It is also interesting to note from the survey results, that even though participants mostly attended conferences, in house CPD sessions and case reports, they preferred skills training for the CPD needs identified. It is therefore essential that whilst planning CPD training it would be beneficial to involve all stakeholders especially staff nurses with an emphasis to promote quality patient outcomes, critical thinking, clinical reasoning and expert judgement [16] [28] for their autonomous practice in these settings.
The merit of mandatory CPD on personal and professional development is debatable primarily since there is paucity on literature of the intended purposes of CPD [29] ; CPD is often not prioritised because of predetermined professional or personal plans, lack of equity in terms of access, and staff nurse shortages [16] [26] [30] . Until recently, CPD has not been mandatory for maintaining an active nurse or midwife registration in India. For CPD training programmes to be relevant and purposive, they need to be co-produced through maximising engagement with participants based on professional practice models of care that would improve patient care outcomes and safety [28] [31] [32] [33] ; they should also create avenues for career advancement, rather than being incidental, inflexible, ad hoc and a “tick box” exercise to ensure an active nurse/midwife registration [28] [33] [34] .
CPD activities are rarely evaluated in the context of their long term impact on practice or professional development. Since there is a lack of evidence around the impact of CPD programmes now coupled with regular CPD training being made mandatory towards maintaining professional registration for nurses in India, it is appropriate to explore developing models that are locally and contextually relevant to assess the impact of these training programs.
5. Limitations
1) Findings from the study may have been enhanced by in depth Focus Group discussions with participants around some of the survey findings. However, this was not possible due to the restrictions with the duration of the project [9 months], limited funding and geographical distances that needed to be covered.
2) Questionnaires were distributed by designated coordinators within both organisations which may have influenced recruitment of the participants to the study. However, this was overcome by obtaining individual informed consent forms from participants in the study.
3) Questionnaires were only made available in English due to lack of funds for translation and most participants’ first language was not English. However, nurse education in India is delivered in English and coordinators from both institutions were proficient bilingually in Hindi and English and were available for any interpretation if participants required.
6. Conclusions
To our knowledge, this is the first ever needs assessment undertaken on nurses’ CPD training requirements in remote and rural health care settings in India. Health care professionals in sufficient numbers, in the right places, adequately trained, motivated and supported are identified as the backbone of an effective, equitable and efficient health care system [13] . For CPD programmes to be effective, they need to be responsive to both professional and personal needs and more importantly reflect strategic health priorities of a nation. Findings from this survey have helped establish the training needs of the nurses working in areas of remote and rural India. CPD priorities identified reflect the present health transition and health priorities in India, alongside the need for developing their managerial competencies which in effect are crucial to drive their health promotion initiatives with NCDs as well as obstetric and new born emergencies in remote and rural settings.
This paper also highlights the future direction for CPD for nurses working in primary and secondary care within rural and remote settings. It would be interesting to compare these findings with a similar survey among nurses working in urban/tertiary health care settings in India. With the CPD priorities identified from this survey, the next steps would be to develop a CPD training programme either to improve a specific clinical/managerial competency, deliver it to nurses within these organisations followed by an evaluation. This also opens up the possibility to show case this as a model to coproduce CPD training that is relevant and meaningful both to clinical practice and nurses’ professional development.
Taking the cue from the WHO’s need to rejuvenate primary health care [35] , if CPD is needs assessed and co-produced with nurses for their professional development [16] and to promote health within the communities they serve, there is an opportunity for them to carve a niche towards their professional identity and earn recognition for their services [32] .
Acknowledgements
The authors are very grateful to all the participants, coordinators and support from the Management of CHAI & EHA, India; the administrative support for the project from Mrs. Sunitha Pinto & Ms. Sumi Anu Niranjan at SJRI, Bangalore, India.
Ethics Approval
This was obtained from the Institutional Ethics Committee [IEC] of St John’s Medical College [IEC Ref No. 156/2015 dated 22 June 2015], Bangalore which is recognised by the Drug Controller General of India [DCGI], Government of India.
Authors’ Contributions
LM, MW, AS, PM: Developing the methodology, designing the questionnaire and preparation of the manuscript.
VT: designing the questionnaire, data collection, organisation and preparation of the manuscript.
SP, NG: Data organisation, quality check and analysis and statistical support.
Cite this paper
Macaden, L., Washington, M., Smith, A., Thooya, V., Selvam, S.P., George, N. and Mony, P.K. (2017) Continuing Professional Development: Needs, Facilitators and Barriers of Registered Nurses in India in Rural and Remote Settings: Findings from a Cross Sectional Survey. Open Journal of Nursing, 7, 930-948. https://doi.org/10.4236/ojn.2017.78069
References
- 1. Gill, R. (2011) Nursing Shortage in India with Special Reference to International Migration of Nurses. Social Medicine, 6, 52-59.
- 2. Rao, M., Rao, K., Shiva Kumar, A., Chatterjee, M. and Sundararaman, T. (2011) Human Resources for Health in India. Lancet, 377, 587-598. https://doi.org/10.1016/S0140-6736(10)61888-0
- 3. United Nations (2015) India and the MDGs-Towards a Sustainable Future for All. Economic and Societal Commission for Asia and Pacific, UN, Geneva.
- 4. Tiwari, R.R., Sharma, K. and Zodpey, S.P. (2013) Situational Analysis of Nursing Education and Work Force in India. Nursing Outlook, 61, 129-136. https://doi.org/10.1016/j.outlook.2012.07.012
- 5. Australian Health Practitioners Regulatory Agency (AHPRA, Para.1) (2011) Continuing Professional Development. Retrieved 27 Jan, 2017 and Available from http://www.ahpra.gov.au/Education/Continuing-Professional-Development.aspx
- 6. Jayanna, K., et al. (2014) Assessment of Facility Readiness and Provider Preparedness for Dealing with Postpartum Haemorrhage and Pre-Eclampsia/Eclampsia in Public and Private Health Facilities of Northern Karnataka, India: A Cross Sectional Study. BioMed Central, 14, 304. https://doi.org/10.1186/1471-2393-14-304
- 7. Srinivas, D.K. and Adkoli, B.V. (2009) Faculty Development in Medical Education in India: The Need of the Day. Al Ameen Journal of Medical Sciences, 2, 6-13.
- 8. Yeo-Campbell, M., et al. (2013) Identification of Barriers and Facilitators for Education of Nurses in Care of Sick and at Risk New Born Babies in India. Retrieved on 13 Mar 2015 and Available from http://www.newbornwhocc.org/pdf/APW-WHO-SEARO-Shastri-Report.pdf
- 9. Shahhosseini, Z. and Hamzehgardeshi, Z. (2014) Psychometric Properties of an Instrument to Measure the Facilitators and Barrier to Nurses’ Participation in Continuing Education Programs. Global Journal of Health Science, 6, 184-193.
- 10. American Association of Colleges of Nursing and Association of American Medical Colleges (2010) Lifelong Learning in Medicine and Nursing-Final Conference Report. Retrieved on 11 Mar 2015 and Available from http://www.aacn.nche.edu/education-resources/MacyReport.pdf
- 11. American Nurses Credentialing Centers Commission on Accreditation (2014) The Importance of Evaluating the Impact of Continuing Nursing Education Programs on Outcomes: Professional Nursing Practice and Patient Care. http://www.nursecredentialing.org/Accreditation/ResourcesServices/Evaluating-the-Impact-CNE-Outcomes.pdf
- 12. Beatty, R.M. (2001) Continuing Professional Education, Organizational Support, and Professional Competence: Dilemmas of Rural Nurses. Journal of Continuing Education in Nursing, 32, 203-209.
- 13. Fahey, C.M. and Monaghan, J.S. (2005) Australian Rural Midwives: Perspectives on Continuing Professional Development. Rural Remote Health, 5, 468.
- 14. Fischer, E.A., Jayanna, K., Cunningham, T., Washington, M., Mony, P., Bradley, J. and Moses, S. (2015) Nurse Mentors to Advance Quality Improvement in Primary Health Centers: Lessons from a Pilot Program in Northern Karnataka, India. Global Health: Science and Practice, 3, 660-675. https://doi.org/10.9745/GHSP-D-15-00142
- 15. Goulet, F., Hudon, E., Gagnon, R., Gauvin, E., Lemire, F. and Arsenault, I. (2013) Effects of Continuing Professional Development on Clinical Performance: Results of Study Involving Family Practitioners in Quebec. Canadian Family Physician, 59, 518-525.
- 16. Goodall, J., Day, C., Lindsay, G., Muijs, D. and Harris, A. (2005) Evaluating the Impact of Continuing Professional Development. Research Report 659. Department for Education and Skills, University of Warwick. http://www.education.gov.uk/publications/eOrderingDownload/RR659.pdf
- 17. Trained Nurses Association of India (2014) Memorandum of Seventh Pay Commission on Behalf of Nurses in India. New Delhi.
- 18. Ross, K., Barr, J. and Stevens, J. (2013) Mandatory Continuing Professional Development Requirements: What Does This Mean for Australian Nurses? BMC Nursing, 12, 9. http://www.biomedcentral.com/1472-6955/12/9
- 19. Yadav, S. and Arokiaswamy, P. (2014) Understanding Epidemiological Transition in India. Global Health Action, 7. http://www.globalhealthaction.net/index.php/gha/article/view/23248 https://doi.org/10.3402/gha.v7.23248
- 20. WHO (2013) Global Action Plan for the Prevention and Control of Non-Communicable Diseases 2013-2020. Geneva. http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf
- 21. Raha, S., Berman, P. and Bhatnagar, A. (2009) Some Priority Challenges of the Nursing Sector in India. India Health Beat-Supporting Evidence-Based Policies and Implementation. Public Health Foundation of India. 1(5) World Bank 70243.
- 22. Deloitte (2014) Global Health Care Outlook. Shared Challenges, Shared Opportunities. http://www2.deloitte.com/.../global/...Health-Care/dttl-lshc-2014-global-health
- 23. WHO (2013) Country Cooperation Strategy at a Glance India. http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_ind_en.pdf
- 24. World Health Organization (2005) Report on Preventing Chronic Diseases: A Vital Investment. Geneva. http://www.who.int/chp/chronic_disease_report/en/
- 25. Evans, C., Rafia, R. and Cook, E. (2013) Building Nurse Education Capacity in India: Insights from a Faculty Development Programme in Andhra Pradesh. BMC Nursing, 12, 8. http://www.biomedcentral.com/1472-6955/12/8 https://doi.org/10.1186/1472-6955-12-8
- 26. Shields, M.A. and Ward, M. (2001) Improving Nurse Retention in the National Health Service in England: The Impact of Job Satisfaction on Intentions to Quit. Journal of Health Economics, 20, 677-701.
- 27. Pasayan, E., Pangket, P., Nialla, J. and Laban, L. (2014) Work Life Balance among Nurse Educators towards Quality Life: A Mixed Method Study. International Journal of Sciences: Basic and Applied Research (IJSBAR), 18, 386-401. Retrieved from http://gssrr.org/index.php?journal=JournalOfBasicAndApplied&page=article&op=view&path%5B%5D=2777
- 28. Duff, B. (2010) Development and Evaluation of an Integrated Clinical Learning Model to Inform Continuing Education for Acute Care Nurses. Doctor of Health Science Thesis, School of Nursing, Queensland University of Technology. http://eprints.qut.edu.au/42622/1/Beverley_Duff_Thesis.pdf
- 29. Gould, D., Kelly, D., White, I. and Chidgey, J. (2004) Training Needs Analysis. A Literature Review and Reappraisal. International Journal of Nursing Studies, 41, 471-486.
- 30. UN-ESCAP (2015) India and MDGs—Towards a Sustainable Future for All. 9. http://www.unescap.org/sites/default/files/India_and_the_MDGs_0.pdf
- 31. Angus, K., Cairns, G., Purves, R., Bryce, S., MacDonald, L. and Gordon, R. (2013) Systematic Literature Review to Examine the Evidence for the Effectiveness of Interventions That Use Theories and Models of Behaviour Change: Towards the Prevention and Control of Communicable Diseases. Insights into Health Communication. European Center for Disease Prevention and Control.
- 32. Lyons, S.S., Specht, J.P., Karlman, S.E. and Maas, M.L. (2008) Everyday Excellence: A Framework for Professional Nursing Practice in Long Term Care. Research in Gerontological Nursing, 1, 217-228. https://doi.org/10.3928/00220124-20091301-08
- 33. Clinical Education and Training (2010) Building Blocks of Life Long Learning—A Framework for Nurses and Midwives in Queensland. Queensland Govt. http://citeseerx.ist.psu.edu/viewdoc/download;jsessionid=53F09540EDC75738E5D448775DF0EBB4?doi=10.1.1.368.8475&rep=rep1&type=pdf
- 34. Mathers, N., Mitchell, C. and Hunn, A. (2012) A Study to Assess the Impact of Continuing Professional Development (CPD) on Doctors Performance and Patient/Service Outcomes for the GMC. Academic Unit of Primary Medical Care, University of Sheffield. Capita Business Services Ltd. http://www.gmc-uk.org/A_study_to_assess_the_impact_of_continuing_professional_develop-ment__CPD__on_doctors__performance_and_patient_service_outcomes_for_the_GMC_51707533.pdf
- 35. WHO (2011) Sexual and Reproductive Health—Core Competencies in Primary Health Care. Geneva. http://apps.who.int/iris/bitstream/10665/44507/1/9789241501002_eng.pdf