Open Journal of Obstetrics and Gynecology
Vol.3 No.1A(2013), Article ID:27690,6 pages DOI:10.4236/ojog.2013.31A028
Five-year impact of a new departmental protocol on emergency cesarean target times
![]()
Department of Obstetrics, University Hospital of Zurich, Zurich, Switzerland
Email: roland.zimmermann@usz.ch
Received 31 October 2012; revised 1 December 2012; accepted 9 December 2012
Keywords: Emergency Cesarean Delivery; Decision-to-Delivery Interval; Neonatal Outcome; Maternal Outcome
ABSTRACT
Objective: To evaluate the impact of an emergency cesarean standard operating procedure (SOP) on the decision-to-delivery interval (DDI) and to determine whether a shorter DDI improves neonatal outcome. Methods: Retrospective analysis of emergency cesareans from 2004 (introduction of the new SOP) to 2009 in a Swiss Level 3 perinatal center. Primary endpoints were the DDI, the pathology-to-decision interval (PDI), the 5-year learning curve, and neonatal and maternal outcome. Results: In the emergency cesarean group (175 women and 188 infants), mean DDI decreased over the observation period from 15 to 9 minutes (mean 10 minutes 41 seconds), and mean PDI from 11 to 6 minutes (mean 8 minutes). Not only did the DDI not exceed 15 minutes in over 90% of cases during the 5 years, but it fell consistently below 10 minutes in the latter stages of the learning curve. Only 2/188 infants had an umbilical artery pH < 7.00 and 19/188 had an Apgar score < 5 at 5 minutes. Maternal morbidity comprised three cases of superficial wound infection. Conclusion: Logistic prerequisites comprise a surgical capability directly within the delivery suite, a standby surgical and anesthetic team, a crash call system, and clear duty allocation. International guideline target times are readily achievable at no additional significant fetal or maternal cost.
1. INTRODUCTION
Animal studies show that the risk of irreversible fetal damage is proportional to the duration of pre-delivery asphyxia [1]. In humans, fetal distress apparent in the cardiotocogram (CTG) in obstetric emergencies such as placental abruption, uterine rupture, umbilical cord prolapse, and maternal respiratory failure prompted the definition, a little over 25 years ago, of a maximum decision-to-delivery (DDI) interval for an endangered child. US guidelines require all hospital obstetric services to be geared to performing emergency delivery within 30 minutes of the decision to operate [2]. UK guidelines recommend delivery as soon as possible, ideally also within 30 minutes [3]. German guidelines prefer a 20-minute DDI [4]. However, several studies have challenged the totemic 30 minutes [5-7], while others have reported that obstetric departments often fail to achieve the target times in practice, for various reasons [8-10].
Our aim was to analyze the impact on neonatal and maternal mortality and morbidity of a new standard operating procedure (SOP) for emergency cesarean delivery. We wished to determine whether an obstetric department is capable, under appropriate logistic preconditions, of undercutting the 30- or even 20-minute DDI target without simultaneously threatening the safety of mother or child.
2. MATERIALS AND METHODS
Zurich University Hospital obstetric department is a Level 3 facility with 2500 deliveries per year and a cesarean delivery rate of 38%. In addition to a dedicated operating suite, all rooms in the labor suite are equipped to accommodate emergency cesarean delivery should the operating suite be busy.
The deficits of old SOP were no clearly defined tasks for each individual participating in the emergency caesarean delivery, inconsistent communication about the urgency of caesarean delivery, no documentation of DDI and no written protocol specifying in particular the tasks that would normally be performed (e.g. hand disinfection und skin disinfection), but must be skipped to ensure fast and safe caesarean delivery. Also we wasted most of DDI-Time in informing all participants about the emergency caesarean delivery, calling each of them personally.
In 2004 our department produced a revised SOP detailing the duties of each health professional in the event of a life-threatening fetal and/or maternal emergency [11], designed to ensure that emergency deliveries are performed within the shortest possible time frame at minimum fetomaternal cost. A central feature was the introduction of an electronically timed “Emergency Cesarean” crash call paged to each member of the designated standby team. We analyzed all emergency deliveries recorded in the departmental database from November 2004 to December 2009. The primary analysis excluded cases with incomplete data and those in which the decision to proceed to emergency cesarean was taken in the operating room. We analyzed maternal morbidity and fetal mortality and morbidity by comparing emergency cesarean deliveries with elective cesarean deliveries matched for gestational age and number of children in the ratio 1:2. Study parameters were DDI, PDI, neonatal pH, Apgar scores, admission to the neonatal intensive care unit, neonatal mortality, and maternal preand postoperative complications. DDI was timed from crash call to birth and PDI from the beginning of pathology to crash call. The beginning of pathology was validated by the obstetrician deciding on emergency cesarean delivery (e.g. The beginning of fetal bradycardia was timed manually from the electronic CTG (OB TraceVue, Philips); by vaginal bleeding midwife’s call to obstetrician was timed as a beginning of pathologie). All cesarean deliveries met the grade 1 urgency criteria proposed by Lucas et al. [12], and pathologies were classified as proposed by Leung et al. as irreversible, potentially reversible, and unknown (no identifiable cause) [7]. All infants underwent predischarge assessment. In a separate analysis, in order to exclude systematic bias, we compared Apgar scores and umbilical artery pH between included cases and all births with incomplete data.
We used Microsoft Excel for the statistical analysis, Fisher’s exact test or the chi square to compare proportions depending on group size, Student’s t test for normally distributed variables, the Mann-Whitney U test for non-normally distributed variables, odds ratios and 95% confidence intervals, and a significance level of <0.05.
3. RESULTS
The database contained 228 emergency cesarean deliveries. We excluded eight for failing to meet the criteria for emergency cesarean delivery, two because emergency cesarean delivery was decided in the operating room, and 43 because of missing DDI/PDI data: in most of the latter cases, subject to a separate analysis, the pathology was already present on admission or on initiation of fetal monitoring, making it impossible to determine an actual time of onset. The primary analysis population thus comprised 175 emergency cesareans and 188 infants, matched to 350 elective cesareans and 376 infants (Table 1).
Emergency cesarean indications were irreversible in 81 cases (46%) and potentially reversible (e.g. uterine hyperstimulation, refractory hypotension after induction of epidural anesthesia) in ten cases (6%). The cause of fetal bradycardia was unknown in 84 cases (48%). Irreversible causes included placental abruption (23%), umbilical cord prolapse (9%), malpresentation and/or tocolytic breakthrough (9%), uterine rupture (3%), failed vaginal operative delivery (2%), and severe preeclampsia (1%).
The mean DDI of 15 minutes in 2004 fell steadily until plateauing at 9 minutes in 2009 (Figure 1).
Mean DDI was 10 minutes 42 seconds (range 5 - 31 minutes) (Figure 2). Mean PDI was 8 minutes and showed a similar year-on-year decline in the final 3 years from 11 to 6 minutes.
Fetal outcome data (Table 2) showed a premature birth rate of 52%. Neonatal mortality was 5% in the study group compared to 4% in the controls (nonsignificant [NS]). The nine study group deaths were due to extreme prematurity (25 - 28 weeks [n = 6]), severe preeclampsia, class 3 abruption, and velamentous vessel rupture (n = 1 each). All 13 control deaths were due to extreme prematurity.
Table 1. Maternal characteristics (mean ± standard deviation unless otherwise stated).
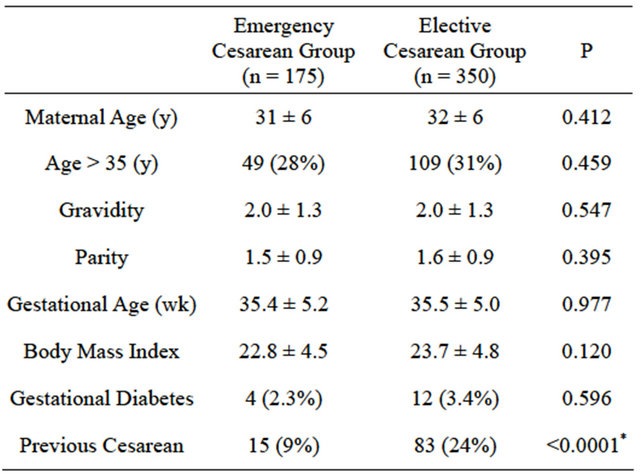
*Significant.
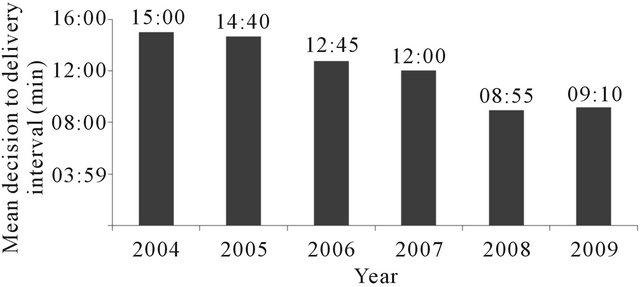
Figure 1. Learning curve.
Table 2. Neonatal outcome.
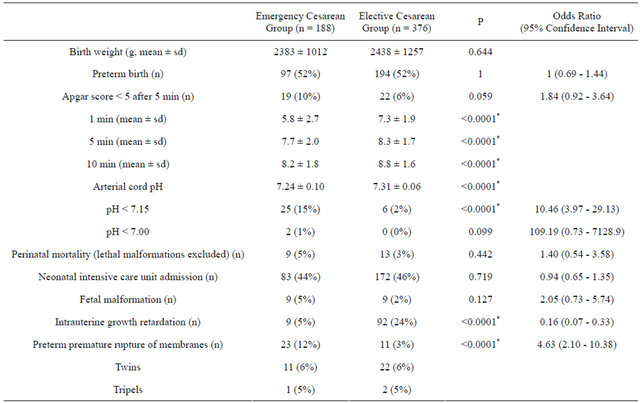
*Significant.
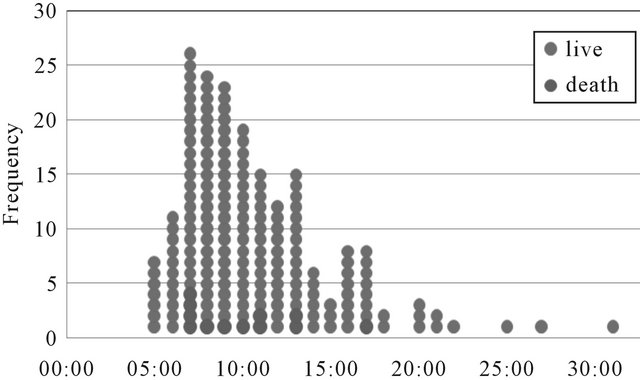
Figure 2. Decision to delivery interval.
Five-minute Apgar scores < 5 were near-significantly more frequent in the study group (19/188 vs 22/376; P = 0.06), as were umbilical artery pH values < 7.0 (2/188 vs 0/376; P = 0.099).
In the 43 infants with incomplete data the frequency of Apgar scores < 5 did not differ from that in the study group (3/43 vs 19/188; P = 0.773), but umbilical artery pH values < 7.0 were significantly more frequent (5/43 vs 2/188; P = 0.003), and there were two neonatal deaths (one due to group B streptococcal septicemia in a severely premature infant, the other to severe ischemia after the drowning of the mother during an epileptic fit at home).
The only difference in maternal morbidity versus the controls was in superficial wound infection, which was confined to the emergency group (3/175) and readily treated (Table 3).
4. DISCUSSION
Our data show that, given certain structural and logistic preconditions, a department is well able to meet a 15- minute target DDI in over 90% of emergency cesareans, and even to consistently undercut a DDI of 10 minutes on completing a learning curve. Target compliance requires a labor ward surgical capability, a stand-by anesthetic and surgical team, a crash call system, and clear task allocation.
The reasons cited for failing to meet the recommended DDI are anesthetic delay, incomplete surgical team, unavailable operating space, and patient transfer to the operating suite [5,9,10] Level 1 hospital funding cannot afford a standby team [14]. This markedly increases fetal mortality [13] and challenges such hospitals’ ability to offer the timely obstetric service required. Operating suite bottlenecks [14,15] and transfer time to the operating suite [8] emphasize the importance of equipping labor wards for emergency surgery.
Table 3. Maternal outcome (n [%]).
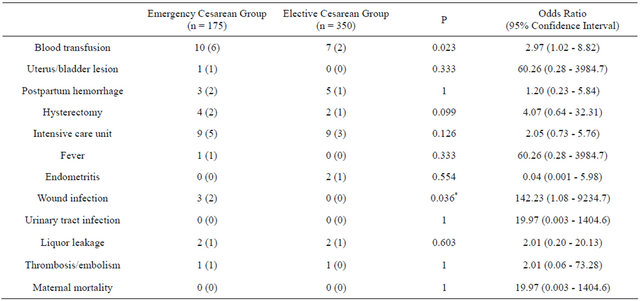
*Significant.
Anesthetic delay is the reason most cited in Level 3 hospitals [9,14,15]. We could not confirm reports of anesthetic delay being responsible for two-thirds of overlong DDI [9]. We believe this is because our SOP equates the urgency of emergency cesarean delivery with adult cardiopulmonary resuscitation.
Irreversible causes were more frequent in our population than in Leung et al. (46% vs 16.6%) [7] and unknown causes fewer (48% vs 74%). The high proportion of irreversible causes is retrospective endorsement of the crash call. Rapid delivery was associated with favorable neonatal outcome. Severe acidosis was markedly less frequent, 1.2%, than in other studies [6,7,9,13,16,17]. Given that umbilical artery pH was <7.00 in just two infants, we conclude that a DDI < 15 minutes largely prevents irreversible damage. Perinatal mortality did not exceed that in controls. However, we did not compare outcome in terms of long-term handicap.
Drills could perhaps have accelerated the team learning curve. Simulation training enhances knowledge, practical performance, communication, and team work in acute obstetric situations [18]. However, our department experiences emergency cesareans on a near-weekly basis, so that it is unlikely that additional training would have achieved more than marginal improvement. In less busy departments, drills are essential.
PDI is as important as DDI, if not more so. Berglund et al found a PDI > 45 minutes in 126/177 malpractice cases of fetal asphyxia, a median PDI of 120 minutes, and a PDI > 500 minutes in six cases [19]. There is no point in meeting a target DDI of 10 minutes in the absence of a matching PDI. Our concern to lower the DDI raised team awareness of fetal danger, halving mean PDI from 11 minutes to 6 minutes. Introduction of intranet monitoring cut the time to crash calls, but did not increase their overall frequency. In the excluded group, by most of the cases, pathology was present before monitoring began, hence the more frequent cases of pH < 7, confirming the crucial role of PDI in asphyxia prevention strategy.
Level 3 centers handle high rates of prematurity but the 52% among emergency cesareans was twice that in our department as a whole, largely due to placental abnormalities. Conversely, the fact that nearly half our emergencies were term deliveries is a reminder that Level 1 centers must be fully geared to urgent cesarean delivery.
Maternal complications were confined to three cases of superficial wound infection in the emergency group. Although infrequent and readily treated, this complication underlines the importance of antibiotic prophylaxis in elective surgery [20]. Lowering the DDI might increase maternal risk as emergency cesarean delivery usually requires general anesthesia with the danger of aspiration. However, anesthetic maternal deaths are listed in national registers [21], and there have been none in Switzerland in the last decade [22]. Preneutralizing the gastric contents with sodium citrate drastically reduces the risk of fatal aspiration [23].
Clinical studies show that many departments cannot perform emergency cesarean delivery within 30 minutes. Some even conclude that inability to meet this target has a positive rather than negative impact on neonatal outcome [5,6]. However, literature review reveals wide differences in the definition of urgency. Studies have frequently included all nonelective cesarean deliveries in addition to grade 1 indications. PDI data are often lacking. Also, the infants most at risk of poor outcome are those that are delivered fastest, which could lead to systematic bias. We therefore believe the contention that a DDI > 30 minutes improves neonatal outcome to be false. Studies confined to emergency cesarean delivery for irreversible causes (uterine rupture, placental abruption) have consistently shown markedly better neonatal outcome with faster intervention [24,25].
5. CONCLUSION
Our study shows that, with the right structural and logistic preconditions, an obstetric department is well able to meet a target DDI of 15 minutes in over 90% of emergency cesareans. Neonatal outcome did not differ significantly from that in the elective cesarean controls and maternal morbidity was not unacceptably raised. However, the PDI is just as important as the DDI for the newborn, and must be taken into account in future studies.
REFERENCES
- Adamsons, K. and Myers, R.E. (1977) Late decelerations and brain tolerance of the fetal monkey to intrapartum asphyxia. American Journal of Obstetrics & Gynecology, 128, 893-900.
- American Academy of Pediatrics, American College of Obstetricians and Gynecologists (1988) Intrapartum and postpartum care of women. Guidelines for perinatal care. AAP, Elk Grove Village, ACOG, Washington, 125-161.
- Royal College of Obstetricians and Gynaecologists (Great Britain) (1995) Organisational standards for maternity services: Report of a joint working group. RCOG Press, London.
- Berg, D. and Ratzel, R. (1995) Minimum requirements for procedural, structural and organizational preconditions for obstetric departments. Frauenarzt, 36, 27-33.
- Tuffnell, D.J., Wilkinson, K. and Beresford, N. (2001) Interval between decision and delivery by caesarean section—Are current standards achievable? British Medical Journal, 322, 1330-1333. doi:10.1136/bmj.322.7298.1330
- Bloom, S.L., Leveno, K.J., Spong, C.Y., Gilbert, S., Hauth, J.C., Landon, M.B., et al. (2006) Decision-to-incision times and maternal and infant outcomes. Obstetrics & Gynecology, 108, 6-11. doi:10.1097/01.AOG.0000224693.07785.14
- Leung, T.Y., Chung, P.W., Rogers, M.S., Sahota, D.S., Lao, T.T. and Hung Chung, T.K. (2009) Urgent cesarean delivery for fetal bradycardia. Obstetrics & Gynecology, 14, 1023-1028. doi:10.1097/AOG.0b013e3181bc6e15
- Helmy, W.H., Jolaoso, A.S., Ifaturoti, O.O., Afify, S.A. and Jones, M.H. (2002) The decision-to-delivery interval for emergency caesarean section: Is 30 minutes a realistic target? Journal of Obstetrics & Gynaecology, 109, 505- 508. doi:10.1111/j.1471-0528.2002.00491.x
- Onah, H.E., Ibeziako, N., Umezulike, A.C., Effetie, E.R. and Ogbuokiri, C.M. (2005) Decision-delivery interval and perinatal outcome in emergency caesarean sections. Journal of Obstetrics & Gynaecology, 25, 342-346. doi:10.1080/01443610500119671
- Livermore, L.J. and Cochrane, R.M. (2006) Decision to delivery interval: A retrospective study of 1000 emergency caesarean sections. Journal of Obstetrics & Gynaecology, 26, 307-310. doi:10.1080/01443610600594898
- Zimmermann, R. (2006) Obstetric handbook. Department of Obstetrics, Zurich University Hospital, Zurich.
- Lucas, D.N., Yentis, S.M., Kinsella, S.M., Holdcroft, A., May, A.E., Wee, M., et al. (2000) Urgency of caesarean section: A new classification. Journal of the Royal Society of Medicine, 93, 346-350.
- Korhonen, J. and Kariniemi, V. (1994) Emergency cesarean section: The effect of delay on umbilical arterial gas balance and Apgar scores. Acta Obstetricia et Gynecologica Scandinavica, 73, 782-786. doi:10.3109/00016349409072505
- Spencer, M.K. and MacLennan, A.H. (2001) How long does it take to deliver a baby by emergency caesarean section? Australian and New Zealand Journal of Obstetrics and Gynaecology, 41, 7-11. doi:10.1111/j.1479-828X.2001.tb01287.x
- de Regt, H.R., Marks, K., Joseph, D.L. and Malmgren, J.A. (2009) Time from decision to incision for caesarean deliveries at a community hospital. Obstetrics & Gynecology, 113, 625-629.
- Hillemanns, P., Strauss, A., Hasbargen, U., Schulze, A., Genzel-Boroviczeny, O., Weninger, E., et al. (2005) Crash emergency cesarean section: decision-to-delivery interval under 30 min and its effect on Apgar and umbilical artery pH. Archives of Gynecology and Obstetrics, 273, 161-165. doi:10.1007/s00404-005-0045-7
- Kamoshita, E., Amano, K., Kanai, Y., Mochizuki, J., Ikeda, Y., Kikuchi, S., et al. (2010) Effect of the interval between onset of sustained fetal bradycardia and cesarean delivery on long-term neonatal neurologic prognosis. International Journal of Gynecology & Obstetrics, 111, 23- 27. doi:10.1016/j.ijgo.2010.05.022
- Merién, A.E., van de Ven, J., Mol, B.W., Houterman, S. and Oei, S.G. (2010) Multidisciplinary team training in a simulation setting for acute obstetric emergencies: A systematic review. Obstetrics & Gynecology, 115, 1022- 1031. doi:10.1097/AOG.0b013e3181d9f4cd
- Berglund, S., Grunewald, C., Pettersson, H. and Cnattingius, S. (2008) Severe asphyxia due to delivery-related malpractice in Sweden 1990-2005. British Journal of Obstetrics and Gynaecology, 115, 316-23. doi:10.1111/j.1471-0528.2007.01602.x
- Smaill, F.M. and Gyte, G.M. (2010) Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section. Cochrane Database of Systematic Reviews, 20, CD007482.
- Lewis, G. and Drife, J., Eds. (2001) Why mothers die 1997-1999. In: The Fifth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom, RCOG Press, London.
- Fässler, M., Zimmermann, R. and Quack, K. (2010) Maternal mortality in Switzerland 1995-2004. Swiss Medical Weekly, 140, 25-30.
- Lim, S.K. and Elegbe, E.O. (1991) The use of single dose of sodium citrate as a prophylaxis against acid aspiration syndrome in obstetric patients undergoing caesarean section. Medical Journal of Malaysia, 46, 349-355.
- Leung, A.S., Leung, E.K. and Paul, R.H. (1993) Uterine rupture after previous cesarean delivery: Maternal and fetal consequences. American Journal of Obstetrics & Gynecology, 169, 945-950.
- Kayani, I.K., Walkinshaw, S.A. and Preston, C. (2003) Pregnancy outcome in severe placental abruption. British Journal of Obstetrics and Gynaecology, 110, 679-683. doi:10.1046/j.1471-0528.2003.02088.x

