Open Journal of Genetics
Vol.3 No.1(2013), Article ID:29006,20 pages DOI:10.4236/ojgen.2013.31004
Splenomegaly, hypersplenism, and hereditary disorders with splenomegaly
![]()
1University Research Foundation for Lysosomal Storage Diseases, Coral Springs, USA 2University of Miami Miller School of Medicine, Miami, USA
3Cedars-Sinai Medical Center/Tower Hematology Oncology, Los Angeles, USA
Email: boneal@winning.com; rosenbloomb@toweroncology.com
Received 20 January 2013; revised 28 February 2013; accepted 5 March 2013
Keywords: Splenomegaly; Hereditary Metabolic Disorders; Splenectomy; Lysosomal Storage Diseases; Gaucher Disease; Spherocytosis; Thalassemia
ABSTRACT
Splenomegaly, sometimes of massive extent, occurs in a large number of hereditary diseases, some relatively prevalent and others, rare to ultra-rare. Because physicians are often unfamiliar with the less common disorders, patients may suffer because of diagnostic delay or diagnostic error and may undergo invasive, non-innocuous procedures such as splenectomy that are potentially avoidable were the correct diagnosis suspected. In this review article, we discuss the definition and clinical ramifications of “massive” splenomegaly and describe several rare genetic disorders that are sometimes associated with marked splenic enlargement as well as four additional hereditary “splenomegalic” lysosomal storage diseases (cholesterol esterase storage disease, Niemann-Pick C disease, acid sphingomyelinase deficiency disease, Gaucher disease) in which approved or promising experimental treatments should generally obviate the need for palliative splenectomy. We also summarize current concepts about the appropriate use of splenectomy in patients with β-thalassemia, hereditary spherocytosis and Gaucher disease and discuss surgical alternatives to classical total splenectomy for these disorders.
1. INTRODUCTION
The differential diagnosis of splenomegaly is extensive (Table 1). Most often, the etiology is evident in light of historical and genealogical information and the concurrent presence of familiar, often pathognomonic, physical or laboratory findings (e.g. lymphadenopathy, stigmata of chronic cirrhosis or rheumatoid arthritis, abnormal blood morphology suggestive of hematological malignancies, hemoglobinopathies or red cell cytoskeletal disorders). Less commonly, there may be no relevant past or family history and accompanying findings may be non-specific (e.g. hematologic cytopenias without abnormal morphology), rare and unfamiliar (e.g. “gray” platelets), or simply not present. It is this scenario that so often leads to diagnostic error or delay in patients with splenomegaly that ultimately proves to be attributable to rare hereditary genetic diseases with which many physicians are unfamiliar.
Sustained diagnostic uncertainty is particularly stressful (for patient and physician) when splenomegaly is “massive”, overtly symptomatic and sometimes accompanied by fear of an underlying malignancy. In such circumstances, clinicians, who are sometimes unaware of available biochemical or genetic testing possibilities, may feel pressed to seek a quick answer through invasive procedures such as bone marrow and liver biopsy or even total splenectomy that they may regard as not only diagnostic but also therapeutic. Although sometimes still necessary in the absence of diagnostic or therapeutic alternatives, this strategy is increasingly less tenable with the advent of effective specific treatments for some hereditary metabolic diseases and in light of cross-disease evidence of significant increased post-splenectomy morbidity risk in children and adults.
The following case report, describing a young woman with Gaucher disease, a lysosomal enzyme deficiency disorder with multiple available pharmacological treatment options, is instructive:
A 21-year-old woman of Ashkenazi Jewish descent presented with abdominal pain and protuberance of 10 months duration. As a child, she had frequent abdominal discomfort and easy bruising, occasional episodes of epistaxis and gum bleeding and an extensive hematoma of the jaw and chin following wisdom tooth extraction at age 12. In terms of height, weight and sexual maturation, growth and development were unremarkable. An abdominal CT scan revealed massive splenomegaly and cholelithiasis. She had mild anemia and leucopenia (hemo-
Table 1. A Partial Differential Diagnosis of Splenomegaly*+.
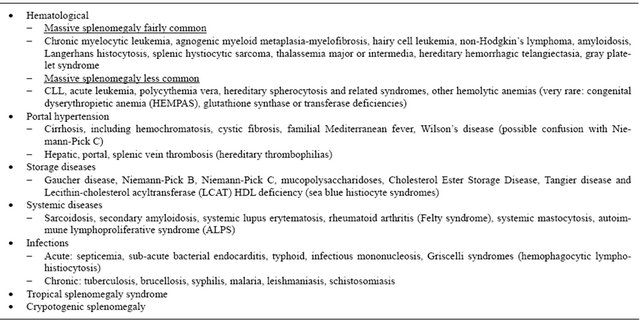
*Adapted from Hoffbrand, Av., Moss, P.A.H., Pettit, J.E., Essential Haematology, 5th Edition, 2006, Wiley Blackwell, p. 126; +Hereditary disorders appear in bold type.
globin concentration 9.7 g/dL; WBC 3400/µL) and marked thrombocytopenia (platelet count 44,000/µL. Gaucher disease was suspected, but, because of the thrombocytopenia, fear of potential splenic rupture and in anticipation of a possible forthcoming pregnancy, a total splenectomy was performed with a liver biopsy, cholecystectomy and removal of a small accessory spleen. The post-operative spleen weighed 2.6 kg (4.3% of body weight; 22 times normal) and was infiltrated with sheets and aggregates of CD68 positive macrophages with the characteristic histological features of Gaucher cells. Two months post-splenectomy, the patient had clinically evident progressive hepatomegaly and thrombocytosis (platelet count 569,000/µL).
The presumed diagnosis of Gaucher disease was confirmed by WBC β-glucosidase testing. Without further therapeutic intervention, we feared that this patient, now asplenic, would have accelerated Gaucher disease manifestations including irreversible skeletal, hepatic and possibly pulmonary morbidity and an increased risk for post-splenectomy complications. There is strong evidence that ERT is highly effective for the hematological, visceral and skeletal manifestations of Gaucher disease in both asplenic patients and those with intact spleens (see below). Biweekly intravenous ERT infusions were begun. 16 months after beginning treatment, the CBC and liver volume are normal. She will continue regularly scheduled physical, laboratory and imaging evaluations with particular attention to changes in bone marrow infiltration, skeletal structure, bone mineral density, pulmonary function and health related quality of life.
In this review article, we discuss:
• The definition and clinical ramifications of “massive” splenomegaly;
• Several rare genetic disorders at times associated with marked splenic enlargement (some only recently described);
• Four hereditary “splenomegalic” lysosomal storage diseases (cholesterol esterase storage disease, Niemann-Pick C disease, acid sphingomyelinase deficiency disease, Gaucher disease) in which approved or promising experimental treatments should generally obviate the need for palliative splenectomy;
• Current concepts about the appropriate use of splenectomy in patients with β-thalassemia, hereditary spherocytosis and Gaucher disease and discuss surgical alternatives to classical total splenectomy for these disorders.
2. DEFINITION OF AND CLINICAL PROBLEMS ASSOCIATED WITH MASSIVE SPLENOMEGALY
Based on weight measurements and calculation of volume by water displacement of cadaveric and surgically resected spleens, normal splenic volume in mL in children and adults of all ethnicities and “racial” backgrounds is generally assumed to be 0.2% of total body weight in kilograms (approximately 200 ± 50 mL in an adult 70 kg man) [1]. The normal splenic volume in vivo may actually be 25% - 50% greater because of dissipation of the splenic blood volume post mortem or post resection [2], may have somewhat greater upwards variability in children and adolescents, and likely correlates better with body height [3,4] than with body weight, particularly in obese individuals. Nevertheless, the 0.2% of body weight calculation is a commonly applied parametric standard for the definition of mild degrees of splenomegaly detectable by CT, MR or ultrasonic imaging techniques. In normal individuals or in patients with mild splenomegaly, the spleen generally retains its usual tetrahedral shape and there appears to be a good correlation between measurements whether by MR, CT or ultrasound [1].
On the other hand, as the spleen progressively and chronically enlarges, and particularly when it reaches massive proportions so that it is patently evident on physical examination (unless the examiner misses a lower splenic margin that extends below the left iliac crest into the pelvis), the shape may be distorted due to processes of infarction, necrosis, fibrosis and scarring rendering volume calculations based on longitudinal or even three dimensional measurements notoriously inaccurate. Nevertheless, most of the published criteria for defining massive splenomegaly are based on physical examination or unidimensional measurements of the spleen. Not surprisingly, there is considerable variation in how massive splenomegaly is defined. In recent publications describing techniques for laparascopic splenectomy, massive splenomegaly has been described as ≥17 cm craniocaudal length, >20 cm, or splenic margin below the umbilicus or anteriorly extending over the midline [5,6].
Although delineating what constitutes massive splenomegaly is of considerable importance in determining surgical technique should the need for splenectomy arise [5], the contribution of splenic size to clinical symptoms and functional impairment is surprisingly unpredictable. Among 33 type 1 Gaucher disease patients older than age 10 in whom ultrasound-measured splenic volumes exceeded 40 times normal, 18 (55%) had no abdominal symptoms at all. Four patients complained of abdominal discomfort, five had early satiety and only 6 reported episodes of some type of abdominal pain [7]. Although there was a statistically significant inverse correlation between spleen volume and red blood cell and platelet counts presumably attributable to more pronounced hypersplenism, the actual changes in cell counts per “fold-increase” in spleen size were clinically unimportant. Similarly, a recent report from the International Collaborative Gaucher Registry and Amsterdam Medical Center demonstrated that although splenomegalic patients with Gaucher disease with volumes in excess of 2000 mL almost always have persistent moderate to severe decreases in platelet count, the magnitude of thrombocytopenia differs relatively little over a spleen volume range of 2000 - 5000 mL [8].
Other complications that are often attributed to massive splenomegaly include initial and recurrent splenic infarctions, splenic rupture, hemodynamic abnormalities including an elevation in plasma volume and a high cardiac output state, increased splenic blood flow leading to portal hypertension, increased intra-abdominal pressure causing respiratory impairment and pulmonary hypertension, and obstructive hydronephrosis. However, there is reason to believe that these events are less a generalized function of splenic size but rather outcomes driven by pathophysiology specific to the disease state causing the splenomegaly. For example, regardless of spleen size, splenic infarction occurs infrequently in patients with cirrhosis, portal hypertension and congestive splenomegaly [9,10] and in splenomegalic patients with hereditary spherocytosis or autoimmune hemolytic anemia in the absence of coexistent hemoglobin S mutations or hereditary or transient thrombophilia [11-13]. On the other hand, infarction is a more common complication in splenomegalic patients with hematological malignancies (e.g. agnogenic myeloid metaplasia-myelofibrosis) or collagen vascular diseases (systemic lupus erythematosis, Wegener’s granulomatosis or rheumatoid arthritis with Felty’s syndrome) largely attributable to the frequency of coexistent hyperproliferation and/or hypercoagulability [14-16].
Non-traumatic splenic rupture is a rare event which may occur in the absence of any known prior diagnosis but nonetheless is likely attributable to the presence of pre-existent splenic cysts, abscesses, areas of infarction or other parenchymal changes that may increase tissue friability as sometimes noted in patients with infectious monocucleosis [17]. The contribution of spleen size per se to the risk of either spontaneous or traumatic splenic rupture is unclear although rapid, acute enlargement may be a favorable setting and the above mentioned intrasplenic pathologies are more common in patients with progressive splenomegaly. However, as is often the case in patients with splenomegaly that is associated with hereditary disorders, chronic splenic enlargement that develops over many years commonly results in a rubbery or fibrotic consistency of splenic tissue that is believed to decrease the risk for splenic rupture [18]. Nevertheless, rare instances of life-threatening splenic bleeding due to intracapsular hemorrhage and splenic rupture have been reported in such circumstances [19].
Portal hypertension in the absence of primary liver disease (hyperkinetic portal hypertension) has been attributed to increased spleen-derived portal blood flow in patients with massive splenomegaly due to myelofibrosis, tropical splenomegaly syndrome, progressive systemic sclerosis with Sjogren’s syndrome, and hereditary hemorrhagic telangiectasia [20-23]. Nevertheless, a number of quantitative studies have shown that splenic volume actually has a weak correlation with splenic vein diameter, portal hypertension or the presence of gastroesophageal varices [24,25]. Clinically significant portal hypertension in the absence of hepatic fibrosis and cirrhosis is very rare in splenomegalic patients with type 1 Gaucher disease [26,27]. A putative case of hyperkinetic portal hypertension in a patient with myelofibrosis in fact turned out to be attributable to combined splenic and portal vein thrombosis [28].
Whether other hemodynamic abnormalities such as high cardiac output and pulmonary hypertension (PHT) are directly related to massive splenomegaly is also uncertain. Splenomegalic, transfusion-dependent patients with beta-thalassemia major and intermedia frequently have evidence of a high cardiac output state, left ventricular remodeling and increased pulmonary artery pressure prior to splenectomy. However, these abnormalities were observed to remain unchanged even after splenectomy [29]. PHT has been reported in connection with several hemolytic conditions that are often associated with splenomegaly including various hemoglobinopathies and, more rarely, hereditary spherocytosis [30-32]. However, the key provocative factor appears to be vasculopathy consequent to a chronic hemolytic state rather than any mechanical effect associated with splenomegaly particularly in view of repeated observations that PHT is much more likely to be encountered in these conditions after rather than prior to splenectomy. PHT in patients with myelofibrosis secondary to myeloproliferative disease is also more likely attributable to combinations of hematopoietic infiltration of the pulmonary parenchyma, thrombocytosis, hypercoagulability associated with chronic disseminated intravascular coagulation, and left ventricular failure than to the mechanical effects of massive splenomegaly although a contribution from splenomegaly-induced portal hypertension and increased abdominal pressure cannot be discounted [33,34].
It might be thought that marked compression of the left kidney is a common event in patient with massive splenomegaly. Surprisingly, however, there is only one report of renal insufficiency reversible with splenectomy due to such a mass effect [35]. However, I recently have encountered a patient with type 1 Gaucher disease, massive splenomegaly, renal insufficiency and left hydronephrosis whose renal function has improved after cystoscopic stenting and reduction in splenomegaly with enzyme replacement therapy.
From the above, it is evident that a management plan for a patient with massive splenomegaly (however defined) must entail an individualized, comprehensive evaluation beyond the obvious elements of age, gender, primary and secondary diagnoses, quantitative spleen size and acuity of enlargement, hematological parameters, clinical symptoms and an overall health profile to include information about splenic internal architecture and external anatomy, other organs and vasculature of the abdomen and chest, bleeding risk, thrombophilia and activated coagulation, cardiac, hepatic and renal function, portal and pulmonary hypertension as well as the potential virtues and risks of either medical or surgical treatment. Similarly, for potentially reversible disorders involving the spleen such as the inherited metabolic disease, Gaucher disease, assessment of treatment efficacy or creation of therapeutic goals for splenomegaly based solely on decreasing spleen volume to the exclusion of even non-invasive information about splenic architecture and internal organization, although more practical and amenable to statistical analysis, is probably overly simplistic.
3. HEREDITARY DISORDERS SOMETIMES ASSOCIATED WITH MASSIVE SPLENOMEGALY
When asked for a differential diagnosis for a 42-year-old man with splenomegaly, anemia, thrombocytopenia, hepatomegaly, and acute and chronic bone pain, a survey group of 406 hematologists from the United States, Canada, Brazil, Argentina, Spain, Japan and Australia overwhelmingly chose various hematological malignancies to the exclusion of anything else [36]. Although the extent to which the practice of hematology is dominated by oncological blood diseases is widely recognized and sometimes lamented, the above results are nonetheless somewhat surprising considering the large number of non-oncological diseases accompanied by splenomegaly, hematological cytopenias and often, hepatomegaly, as shown in Table 1.
In the remainder of this paper, I will briefly describe some of the rare hereditary disorders listed above that are sometimes associated with massive splenomegaly and conclude with a more detailed discussion of Gaucher disease and issues related to splenectomy.
4. GRAY PLATELET SYNDROME (GPS)
GPS [37] is a rare, hereditary bleeding disorder characterized by progressively more severe thrombocytopenia and the presence of giant platelets with a grayish appearance on light microscopic examination of a Wright-Giemsa stained peripheral blood smear. Electron microscopic examination indicates that this unusual morphology is attributable to the virtual absence of platelet alpha granules, intracytoplasmic vesicules normally packed with megakaryocyte-synthesized proteins such as platelet factor 4 and β-thromboglobulin that are secreted during platelet activation and that are promoters of platelet adhesiveness and wound healing [38]. This primary defect leads to a shortened platelet survival time and may also promote release of platelet derived growth factor and other pro-fibrotic substances resulting in deposition of bone marrow reticulin and eventual development of myelofibrosis with splenomegaly. Thrombocytopenia, bone marrow fibrosis and splenomegaly are progressive with age. Nearly all patients have markedly elevated serum vitamin B12 concentrations, an abnormality that is also frequently encountered in patients with neoplastic myeloproliferative diseases [39].
The major clinical manifestation is spontaneous as well as post-traumatic and post-surgical mucosal bleeding that often begins prior to 6 years of age. The bleeding tendency is variable in the known patient population but is reported as severe in about 40 percent. Menometorrhagia is particularly prominent and commonly associated with iron deficiency. Because GPS is so rare, there is usually diagnostic delay and most patients are initially thought to have ITP. Nearly 90 percent of the patients develop splenomegaly. Splenectomy in one patient slowed but did not prevent the eventual onset of thrombocytopenia. Other useful non-specific treatments include prophylactic pre-operative DDAVP and platelet transfusions. One patient is known to have an IgM monoclonal gammopathy and Waldenstrom’s macroglobulinemia developing when 47 years old.
There are probably fewer than 50 identified patients world-wide. Affected families (oftentimes with evidence of consanguinity) of Arab-Bedouin, Turkish, Somalian, and northwestern European Caucasian ethnicity have been described. The pattern of inheritance is consistent with autosomal recessive transmission. The GPS gene was mapped to a 9.4-Mb interval on 3p21.1 - 3p22 and recently, the mutated gene was identified as NBEAL2, a protein-coding gene whose precise function in platelet alpha granule formation is still unknown. As with many other hereditary disorders, patients with the same genotype may have highly variable phenotypes.
5. AUTOIMMUNE LYMPHOPROLIFERATIVE SYNDROME (ALPS) [40]
This autosomal dominant hereditary disorder generally is diagnosed in infants and children who present with fatigue, pallor, icterus, chronic lymphadenopathy and/or splenomegaly accompanied by combinations of autoimmune hemolytic anemia, symptomatic thrombocytopenia, and bacterial infections associated with neutropenia, eosinophilia and monocytosis. The hematological cytopenias tend to improve in adolescents and young adults who nonetheless, over years of follow up, develop other autoimmune or lymphoproliferative disorders including uveitis, hepatitis, glomerulitis, infiltrative pulmonary lesions and Hodgkin’s and non-Hodgkin’s lymphoma.
The disease is caused by failure of apoptotic mechanisms to maintain lymphocyte homeostasis, permitting accumulation of lymphoid mass and persistence of a small population (>1.5% of total lymphocytes) of autoreactive cells (double negative T cells) characterized as CD3+ TCRαβ+ CD4− CD8− in the setting of a normal or elevated lymphocyte count. The majority of cases are associated with autosomal dominant transmission of heterozygous germ line FAS mutations although somatic FAS mutations restricted to subsets of lymphocytes may occur as well. FAS is a membrane bound member of the tumor necrosis factor receptor super-family that, when bound to FAS ligand, triggers caspase mediated lymphocyte apoptosis that is essential for maintenance of lymphocyte homeostasis and prevention of autoimmunity. Phenotypic expression is heterogeneous and some family members with germ line FAS mutations may have mild manifestations or even be asymptomatic. Additional acquired FAS mutations superimposed on mild germ line mutations may contribute to disease expression in some families. The increased risk of developing B cell lymphomas appears to be associated with FAS mutations affecting the intracellular portion of the FAS protein.
More than 300 families and 500 patients with hereditary ALPS have been identified. The diagnosis is dependent on demonstration of non-malignant, noninfectious lymphadenopathy and/or splenomegaly of at least 6 months duration, identification of an increased population of double negative T cells, and germline or somatic mutations in FAS, FAS ligand or Caspase 10. Additional biomarker abnormalities that help establish the diagnosis include elevated plasma levels of FAS ligand, plasma IL-10, plasma IL-18, and plasma vitamin B12 particularly when associated with autoimmune cytopenias and polyclonal hypergammaglobulinemia.
In terms of both genetic counseling and prudent management, it is important to note that, in many patients, the chronic cytopenias appear to spontaneously improve and symptoms regress as children grow older and that later phenomena such as liver disease and infiltrative pulmonary disease have so far been noted in fewer than 5 percent. In fact, most recorded deaths are attributed to post-splenectomy sepsis strongly suggesting that splenectomy should be avoided. Although short-term courses of steroids and IVIG can be useful, when sustained treatment of autoimmune cytopenias is medically indicated, Rao and Oliveira [40] recommend the use of steroid-sparing measures including mycophenolate mofetil (MMF) and sirolimus. Periodic monitoring for development of lymphoma is also recommended.
6. DYSLIPIDEMIA AND SEA BLUE HISTIOCYTOSIS
Sea blue histiocytes have been reported in both the bone marrow and spleen in various hematological malignancies including CML, AML and lymphoma, in various infectious or inflammatory illnesses, and in a patient with alleged ITP [41-43]. They may also be encountered on histological examination of enlarged spleens in patients with Gaucher disease and Niemann-Pick disease and in patients with rare hereditary dyslipidemias.
Familial hypo-α-lipoproteinemia is a rare genetic disorder that is caused by mutations either in the ATP binding cassette A transport protein (Tangier disease), in lecithin-cholesterol acyl transferase (LCAT), or by specific mutations in the apolipoprotein A-1 (APO A-I) gene that affect amino acid residues 121-186 and retard the activation of LCAT by APO A-I (Other APO A-1 mutations that affect the amino terminus residues 1-90 create a different phenotype: APO A-I amyloidosis) [44, 45].
Patients with Tangier disease usually have mild hypertriglyceridemia, peripheral neuropathy, marked enlargement of the tonsils that have a characteristic yellow or orange hue, corneal clouding with arcus senilis, premature atherosclerosis with early onset cardiovascular disease, hepatomegaly and splenomegaly with sea blue histiocytosis. The mode of inheritance is autosomal recessive (chromosome 9q31). There are only about 50 known patients world-wide [46,47].
LCAT deficiency is also very rare with only about 30 families described in the literature. LCAT mutations that result in only partial enzyme deficiency cause an attenuated phenotype restricted to plasma HDL < 10% of normal and corneal opacities that give rise to the moniker “fish eye disease”. Patients in whom there is total LCAT deficiency have a more severe phenotype that includes not only decreased plasma HDL, hypercholesterolemia, corneal clouding and arcus senilis but also splenomegaly with sea blue histiocytosis, normocytic anemia with target cells on the peripheral smear, and deposition of lipoproteins in the kidney leading to microhematuria, sometimes severe proteinuria, and potentially to renal failure [48]. Curiously, LCAT deficiency is not invariably associated with premature atherosclerosis and increased cardiovascular risk possibly because the major determinant of those phenomena is impaired macrophage cholesterol efflux which appears not to be solely dependent on HDL concentration [49,50].
Splenomegaly with sea blue histiocytosis was also noted in two unrelated French Canadian patients, 29 and 49 years old, with an autosomal dominant mutation in apoliproprotein E3, a protein that is a ligand for the LDL receptor. Both patients had moderate splenomegaly and mild thrombocytopenia but nevertheless underwent splenectomy following which both developed severe hypertriglyceridemia despite having had minimal dyslipidemia prior to surgery. Both also developed evidence for premature coronary atherosclerosis suggesting that mutant apoE containing lipoproteins that had been targeted to splenic macrophages might be diverted to vessel wall macrophages as well as to liver and bone marrow macrophages post-splenectomy [51].
7. CHOLESTEROL ESTER STORAGE DISEASE (LAL DFICIENCY)
Cholesterol ester storage disease (CESD) is a very rare autosomal lipid storage disease that is associated with deficiency of lysosomal acid lipase (LAL). Total absence of enzyme activity causes a very severe phenotype called Wolman’s disease that is manifest in infants and that is fatal usually within the first year of life due to malabsorption, growth failure and hepatic failure. When LAL deficiency is less profound, the phenotype is less severe. Symptoms develop later in life and are dominated by liver dysfunction and type II hyperlipidemia. The liver is most severely affected with marked hepatomegaly, hepatocyte necrosis, elevation of transaminases and liver fibrosis that may progress to overt cirrhosis. Cardiovascular involvement is characterized by dyslipidemia (high cholesterol, high triglyceride and low HDL) and accelerated atherosclerosis [52,53]. As with many other hereditary lipid storage disorders, the clinical manifestations are heterogeneous. Some patients are undiagnosed until complications manifest in late adulthood. Others can present with hepatomegaly and hepatocellular dysfunction during childhood or adolescence. Although most clinical descriptions of CESD emphasize the hepatic and cardiovascular abnormalities, some patients also present with splenomegaly even prior to development of cirrhosis and portal hypertension. They also may have hematological cytopenias, modest elevation of serum lysosomal enzymes such as chitotriosidase that are more commonly associated with Gaucher disease, and bone marrow infiltration with sea-blue histiocytes, vacuolated macrophages and plasma cells [54].
The estimated prevalence is less than 0.2 lives per 100,000. Both the CESD and Wolman phenotypes are due to mutations in the LAL gene located on chromosome 10q23.2 - q23.3. Many CESD cases are associated with a homozygous G- > A mutation at position 1 of the exon 8 splice donor site (E8SJM-allele) that allows transcription and translation of a protein with some residual enzyme activity [55].
Although no approved intravenous enzyme replacement therapy (ERT) is yet available for treatment of CESD, SBC-102 (Synageva BioPharma Corporation), a recombinant human LAL is currently undergoing clinical trials. Prior supportive treatments concentrated on dietary restrictions and suppression of cholesterol synthesis and apolipoprotein B production through administration of statins and other lipid lowering therapies [56]. Although sometimes associated with transient improvement, these approaches did not prevent eventual disease progression. There is limited literature regarding liver transplantation for CESD [57].
8. NIEMANN-PICK C DISEASE (NP-C)
Niemann-Pick C disease is a rare autosomal recessive neurovisceral lysosomal storage disease attributable to mutations in either NPC1 (mapped at chromosome 18q11) or NPC2 (chromosome 14q24.3) genes [58]. The product of NPC1 is an endosomal glycoprotein that apparently works in tandem with the gene product of NPC2, a small lysosomal protein, to transport cholesterol and glycosphingolipids from the lysosome to the plasma membrane and endoplasmic reticulum [59]. Loss of either NPC1 function (95% of the cases) or NPC2 function leads to accumulation and retention of cholesterol and glycolipids in late endosomes and lysosomes in visceral organs and in the brain with resultant clinical pathology. Cholesterol storage may secondarily promote neuropathology by altering processing of the β-amyloid precursor protein (APP) leading to increased formation of amyloid-β (Aβ) peptide [60].
NP-C is estimated to occur in 1:120,000 live births [61]. Disease manifestations may begin as early as at birth or may not be evident until the sixth decade of life, although most patients become symptomatic in childhood or adolescence. Discordant manifestations in siblings are commonly observed. Regardless of phenotypic classification, with the exception of infants who die at a very young age because of liver failure, all patients with NP-C eventually develop neuropsychiatric manifestations [58]. Unlike neuronopathic Gaucher disease in which the earliest eye movement abnormality is slow horizontal saccadic movement [62], patients with NP-C have a characteristic vertical supranuclear ophthalmoplegia. Other common CNS manifestations include cerebellar ataxia, dystonia, dysarthria, dysphagia, seizures, psychiatric disorders, cognitive problems and progressive dementia. A diagnostic delay of 3 - 12 years from onset of symptoms is a common experience. Significantly, although splenomegaly is found in nearly all adult patients with overt neurological findings, on retrospective analysis dating back even to childhood, many patients were found to have had pre-symptomatic splenomegaly with foam cell infiltration of the spleen and bone marrow [58]. Splenomegaly in adult patients is usually asymptomatic and non-progressive and often, detectable only with ultrasonography or other imaging procedures. It is suggested that NP-C should always be suspected when isolated splenomegaly in the absence of liver disease is found in a patient with neuropsychiatric symptoms [61]. A finding of foam cells with bone marrow or liver biopsy may heighten suspicion for NP-C. The definitive diagnosis depends on demonstration of abnormal filipin staining in cultured skin fibroblasts and detection of a characteristic mutation on DNA testing.
Without treatment, NP-C is uniformly fatal. Most patients with the more prevalent juvenile variant die before age 25 years. Patients with the less common adult phenotype usually succumb between 30 - 50 years of age. Miglustat (N-butyldeoxynojirinomycin, Actelion Corporation), a small iminosugar molecule approved in the United States and other countries for the treatment of Gaucher disease, reversibly inhibits glucosylceramide synthase, which catalyses the first committed step in glycosphingolipid synthesis. Miglustat was shown to substantially retard progression of neurological manifestations and prolong survival In NP-C mouse models. In human clinical trials, miglustat demonstrated clinically relevant beneficial effects on neurological disease progression but more so in adult, juvenile and pediatric patients than in those diagnosed before age 6 years [63]. Miglustat now has regulatory approval for the treatment of NP-C in the European Union and several other countries and is in continued clinical trial in the United States. Because the clinical trials focused primarily on the clinically crucial neurological response, there is little information on the effect of miglustat on splenomegaly or bone marrow foam cell infiltration in NP-C. Two case reports suggest that miglustat stabilizes but does not necessarily decrease spleen and liver volume in NP-C patients [64,65]. That observation, if confirmed in larger numbers of patients, might lend credence to a suggestion based on experimentation in NP-C mice, that the clinical benefit observed with imino sugar inhibitors of glucosylceramide synthase such as miglustat might not necessarily be attributable to substrate reduction but rather to some unrelated, off-target effect [66].
A second small molecule, cyclodextrin, a commonly used drug delivery vehicle, was unexpectedly shown to reduce intraneuronal lipid storage and signs of neurodegeneration and also prolong survival of NP-C mice. This agent has been given orphan status and is also undergoing clinical trial. It was of interest that cyclodextrin appeared to deplete cholesterol storage from hepatocytes in NP-C mice but with associated accumulation in Kupffer cells, a phenomenon that was observed in wild type mice as well. Additionally, there appeared to be substantial accumulation of cholesterol in pulmonary macrophages with cyclodextrin treatment. No observations were reported on the effect of cyclodextrin on the NP-C mouse spleen or bone marrow [67].
9. NIEMANN-PICK DISEASE TYPES A & B (NPD-B, ASM DEFICIENCY)
Niemann-Pick disease type A and B are biochemically related sphingolipid storage diseases that are associated with deficient activity of lysosomal acid sphingomyelinase (ASM) and therefore etiologically distinct from NP-C. ASM deficiency leads to accumulation of the sphingomyelin substrate primarily in organs rich in tissue macrophages with consequent clinical manifestations including splenomegaly and bone marrow infiltration which in combination lead to hematological cytopenias, hepatomegaly, and pulmonary disease. Although biochemically different, NPD has many clinical features in common with Gaucher disease including classification into neuronopathic and non-neuronopathic sub-types [68]. Classical NPD-A, found predominantly among Ashkenazi Jews (with an estimated carrier frequency of 1:90) is an autosomal recessive neurodegenerative disease characterized by failure to thrive, visceromegaly, progressive psychomotor deterioration with a classic finding of a cherry red macular spot (also observed in Tay-Sachs disease), and death usually before 3 years of age. Other, phenotypically less severe neuronopathic variants have now been identified in other ethnic populations.
NPD-B, on the other hand, appears to lack significant neurological involvement although it is possible that, as with type 1 Gaucher disease, late events such as Parkinsonism in elderly patients may yet emerge with larger patient accrual, longer patient follow up, and particularly if an effective treatment is successfully developed. Although pan-ethnic, NPD-B is a very rare disorder with an incidence estimated at 1:200,000 births. There has been no definitive study of survival or life expectancy [69]. The disease is phenotypically heterogeneous. In a study of 59 patients (31 male), ages ranged from 7 to 65 years although more than half the patients were children or teenagers many of whom had evidence of growth delay and early onset of osteopenia [70]. 49% reported suffering joint or limb pain. Unlike type 1 Gaucher disease (GD1) in which clinically significant lung symptomatology is rare, pulmonary involvement is common in NPD-B and may sometimes be life limiting. Many patients have quantitative evidence of pulmonary dysfunction with chronic dyspnea and intercurrent pulmonary infections [69]. Serum lipid abnormalities including decreased HDL cholesterol and increased LDL, VDL and triglycerides may increase risk for cardiovascular disease [70].
Splenomegaly was the most common physical finding (78%) with the spleen exceeding 15 multiples of normal in 20%. Splenic nodules are common in patients with NPD-B, although, unlike Gaucher disease splenic nodules that are evident on T1 MR imaging, the nodules in NPD-B are often isointense on T1-weighted images but high signal on T2-weighted images [71]. Hepatomegaly is nearly as common as splenomegaly although symptomatic portal hypertension is unusual. Half the patients are thrombocytopenic with a history of clinically significant bleeding in 42% [70]. Nevertheless, only 5 patients (8%) had undergone splenectomy (4 total), a significantly lower splenectomy percentage than usually observed among pre-ERT patients with type 1 Gaucher disease (25% - 30%) [72]. This disparity may reflect the young age of the NPD-B study population because among 887 children and teenagers with type 1 Gaucher disease, only 5% reported having splenectomy [73]. The spleen volume correlated well with liver size, growth assessment, lipid profile, and hemoglobin concentration [69,70]. Therefore, changes in splenomegaly in response to proposed treatments including ASM ERT that are currently in clinical trial may be a reasonable surrogate marker for evaluating response with the possible exception of pulmonary function where the correlation with spleen volume seems less certain [69,70]. A poor correlation between splenomegaly and platelet count that was observed in patients with NPD-B was also documented in patients with GD1, particularly for spleen volumes greater than 12 multiples of normal [8].
10. IDIOPATHIC OR CRYPTOGENIC SPLENOMEGALY
Truly idiopathic splenomegaly is rarely encountered in the medical literature. In most such cases, historically (but generally no longer) referred to as Banti’s syndrome or Banti’s disease, enlargement of the spleen was clearly secondary to underlying liver diseases including cryptogenic cirrhosis and idiopathic portal hypertension [74]. These entities are themselves increasingly associated with known causes such as non-alcoholic fatty liver disease (both obese and lean variants), underlying immunological disorders such as connective tissue diseases and celiac disease, and thrombophilia, but, in many cases, the etiology is still obscure [75-77]. Among potential genetic influences, it appears that hereditary hemochromatosis, the most common inherited disease in European populations, is not commonly associated with cryptogenic cirrhosis and secondary congestive splenomegaly [78].
In other historical reports, alleged idiopathic splenomegaly was likely attributable to post-malaria tropical splenomegaly syndrome [79] or to a preliminary stage of malignant lymphoma or other blood maligancy [80,81]. However, in one study, after diagnostic splenectomy (that was associated with a 29% morbidity and complication rate), 8 of 38 patients (21%) remained without a histologic diagnosis [82].
In this context, the following recent study of a family with combined, apparently hereditary splenomegaly and vision loss is of interest [83]. A mother and two daughters in a single non-consanguineous Caucasian family, presented with splenomegaly and underwent diagnostic splenectomy. Both light and electron microscopic studies were unrevealing of any pathology except congestion of the red pulp and bone marrow examinations (done in two of the patients) were also non-diagnostic. All three patients developed chronic optic nerve edema and progressive loss in central and color vision. The two oldest patients are now blind. “Despite numerous medical and ophthalmic evaluations, no diagnosis has been discovered”.
11. GAUCHER DISEASE (GD)
Professor Guido Banti (1852-1925) was perhaps the most eminent Italian clinician-pathologist-histologist-microbiologist of the early 20th century. Among his many diverse accomplishments, he is famous for his contributions to knowledge of the pathology of the spleen especially as related to hemolysis and hypersplenism. The first splenectomy for hemolytic jaundice was performed in Florence, on his advice, on February 20, 1903 [84]. Therefore, it is perhaps more than a bit ironical that the eponymous syndrome/disease bearing his name (see above) has fallen into disuse (only 34 PubMed references dating back to 1929) whereas the name of a then medical student Phillippe Gaucher who, in an 1882 graduate thesis, first described a single case of a woman with an enlarged spleen containing unusual engorged cells that he initially and incorrectly thought to be malignant [85], is immortalized as both a cell and disease [86] discussed in 398 scientific publications in 2011 alone!
Gaucher disease (GD) is an autosomal recessive inborn error of glycosphingolipid metabolism due to a deficiency of the lysosomal enzyme glucocerebrosidase (acid β-glucosidase) [18]. It is one of the most common hereditary lysosomal storage disorders. The disease is characterized by lysosomal storage of glucocerebroside (glucosylceramide) in macrophages predominantly in bone, bone marrow, liver, and spleen. GD has 3 major phenotypic sub-categories based on the presence or absence of early onset central nervous system manifestations.
Types 2 and 3 Gaucher disease are rare, occurring in 1 in every 100,000 to 200,000 births, and both subtypes display central nervous system pathology. Type 2 Gaucher disease, the acute neuronopathic variant, is the most severe form of the disease and causes death at an early age. In some cases, type 2 Gaucher disease can result in nonviable infants. In other cases, the disease progresses rapidly during the first 1 - 2 years of life, with infants showing neurological manifestations such as bulbar involvement, stridor, dysphagia, head retroflection, opisthotonos, spasticity, and cognitive impairment. The condition invariably causes death, typically before the age of 3 years, even with attentive supportive care [18].
Type 3 Gaucher disease, the subacute or chronic neuronopathic variant, is more clinically heterogeneous. Some individuals with type 3 Gaucher disease are fully functional and able to work, while others may have significant impairments. Mild manifestations include oculomotor apraxia, while more severe forms of type 3 Gaucher disease are characterized by extrapyramidal manifestations, myoclonic or generalized seizures, cerebellar ataxia, and intellectual regression. Although neurologic pathology dominates the clinical presentation in patients with type 2 or type 3 Gaucher disease, many patients with these variants also have the systemic features found in type 1 disease, including hepatosplenomegaly, hematologic abnormalities, and skeletal complications and often enjoy relief from systemic symptoms with initiation of enzyme replacement therapy [87].
Type 1 disease (GD1) constitutes 94% cases of GD currently known and is usually considered to be nonneuronopathic (20). However, recent studies have called that distinction into question because by the seventh to eighth decades of life, an intractable Parkinson-like syndrome, often with atypical features including progressive dementia is reported to occur in 5% - 10% of patients with otherwise typical GD1 [88]. Additionally as many as 15% - 20% of adult type 1 patients may have subjective or objective evidence of peripheral neuropathy [89]. In western countries, type 1 disease occurs in 1/75,000 births. However, in Jews of Ashkenazi (northcentral and eastern European) descent, the only ethnic group in whom the prevalence is markedly increased, it is seen in approximately 1/600 individuals and the carrier rate is 1/15 [90].
GD1 is highly variable in terms of its clinical presentation and manifestations even among siblings with the same genotype and in monozygotic twins [91]. The disease appears to be symptomatic only in about half of the Ashkenazi Jews who are genetically affected [90]. However, even apparently asymptomatic patients often have signs of the disease including anemia, thrombocytopenia, hepatosplenomegaly, and bone abnormalities but may sometimes be discovered only when quite elderly [92]. Individuals with overt symptomatic disease usually have significant visceral involvement, more advanced bone disease, and more severe hematological findings. Patients may be symptomatic for some time, even years, prior to being correctly diagnosed. The delay in diagnosis is often due to the relative rarity of the disease and physicians’ lack of familiarity with the full spectrum of abnormalities associated with Gaucher disease [36]. Unfortunately, this delay in diagnosis can lead to severe and potentially life-threatening complications, including avascular necrosis, severe bleeding, chronic bone pain, sepsis, pathologic fractures, growth abnormalities, and liver disease.
The accumulation of infiltrating Gaucher cells—plus, presumably, the release of cytokines and chemokines and the resulting inflammatory responses [93,94]—invariably results in splenomegaly, the most common visceral disease manifestation of GD1. The spleen size can be enlarged as much as 75-fold, but the median is 15.2 multiples of normal [72]. Solitary or multiple focal splenic nodules were reported present in 18.4% of patients with GD1 [95] although the prevalence may actually be greater because such nodules may not always be detected if MR imaging is restricted to T1-weighting. Patients with focal splenic lesions are more likely to have larger splenic volumes, more severe thrombocytopenia, and a greater prevalence of osteonecrosis than patients lacking these lesions and the response to treatment in terms of reduction in spleen size and improvement in platelet count may be less satisfactory [96] although not invariably so [8].
Although thrombocytopenia and anemia are in large part a function of splenomegaly and hypersplenism, bone marrow infiltration itself appears to contribute to impaired hematopoiesis, a process that may become irreversible once fibrosis and osteosclerosis develop. There may also be an intrinsic defect in the bone marrow endosteal hematopoietic niche associated with osteoblastic dysfunction that might impact cellular maturation [97]. Although there is a rough correlation between splenic size and magnitude of thrombocytopenia, 40% of patients with GD1 in whom the spleen volume is less than five times normal have platelet counts less than 120,000/µL and the platelet count is less than 60,000/µL in 6%. Patients who at the time of diagnosis had thrombocytopenia but minimal splenomegaly tended to be older and more likely to be homozygous for the “clinically mild” N370S genotype [98].
Fatigue, a symptom that commonly occurs even in non-anemic patients with GD1 may be cytokine dependent. Bleeding is most directly related to thrombocytopenia, but patients may have platelet defects and other coagulation factor deficiencies including coincidental factor XI deficiency that is common in Ashhenazi Jews. [99]. Patients with symptomatic skeletal disease often have elvated levels of D-dimer and thrombin-antithrombin complexes consistent with chronic coagulation activation [100,101]. It is unclear whether these abnormalities cause or derive from skeletal pathology.
Skeletal pathology often causes great morbidity and debility [102,103]. Bone and joint pain, sometimes associated with painful crises (due to acute infarcts), can disrupt and limit activities of daily living [73]. Avascular necrosis (AVN) can lead to joint collapse at the hip, knee and shoulder creating a need for joint replacement with sometimes uncertain outcome. AVN may appear unpredictably even in previously asymptomatic patients and may present solely as a radiographic finding in the absence of acute bone pain or bone crisis. Factors associated with an increased risk for AVN include a history of total splenectomy, anemia, and extensive Gaucher cell infiltration evidenced by marked decrease in bone marrow fat fraction and marked elevation of biomarkers such as serum chitotriosidase and macrophage inflammatory protein (MIP-β) [104,105]. Osteolytic lesions, pathological fractures, spinal compression fractures and extraosseous masses (Gaucheromas) also contribute to morbidity Bone disease is worse in surgically asplenic patients, especially in those who were diagnosed when young [106].
Osteopenia may begin before 10 years of age, worsen during adolescence and progress through adulthood. Because many patients do not reach normal peak bone mass, they are at a disadvantage when normal aging processes accelerate and more likely to develop severe osteoporosis [107]. Overall, the incidence of osteopenia and osteoporosis in individuals with Gaucher disease likely exceeds 60%. Although long suspected, low bone mineral density of the lumbar spine was recently confirmed as a strong risk factor for fractures of the spine and femur in patients with GD1 [104].
Symptomatic children tend to have poorer growth velocity. Many children have heights that are less than the 5th percentile for age and sex and 25 % are shorter than expected based upon mid-parental height [108-109]. Growth retardation usually was associated with a greater degree of visceral involvement. Puberty is delayed in 60% of patients who are symptomatic as children.
Hypoxemic interstitial lung disease is a serious but rare manifestation. Pulmonary hypertension attributed to occlusion of pulmonary capillaries and cytokine-associated proliferative vascular lesions also rarely occurs but represents a life threatening complication [110]. The hepatopulmonary syndrome due to abnormal shunting in the lungs also leads to hypoxemia and ultimately liver cirrhosis [111]. Pulmonary hypertension and the hepatopulmonary syndrome are generally encountered in patients who have had a splenectomy [112].
The natural history of GD1 is highly variable. In the Ashkenazi Jewish population, a substantial proportion of genetically affected individuals, not necessarily restricted to the N370S/N370S genotype, have no symptomatic manifestations and few if any signs of anatomical or functional disease. Although less commonly reported, there are undoubtedly asymptomatic patients in nonJewish populations as well. Subject to any other inborn or acquired risk factors, such individuals should have normal life expectancy although they presumably at share the increased risk for Parkinsonism that is now known to be associated with even a single Gaucher GBA mutation [113]. Because most such individuals are unidentified, save for sporadic cases that are increasingly coming to light because of genetic screening programs and greater attention to family histories, it is currently unknown whether they, like symptomatic patients with GD1, also have an enhanced risk for developing MGUS, myeloma, other hematological malignancies and possibly other cancers [114-117]. Nevertheless, there is a general consensus that such minimally affected individuals, when discovered, do not require definitive treatment for GD1 but nonetheless, should have regular annual to biannual comprehensive evaluations.
Among symptomatic patients, prior to the advent of disease-specific treatment twenty years ago, substantial morbidity as described above and shortened life expectancy were commonly observed [118]. Patients who died at a younger than expected age often succumbed to CNS and gastrointestinal bleeding, septicemia, chronic liver disease and cirrhosis, pulmonary hypertension and/ or fibrosis, post-splenectomy complications, and suicide and accidental drug overdose [119]. These deaths were most likely attributable either directly to GD1 pathophysiology or indirectly to acute or chronic complications of total splenectomy performed, absent a therapeutic alternative, to alleviate the hematological and visceral manifestations of GD1.
Most symptomatic patients with GD1 are now treated with one of several approved treatments that specifically reduce glucosylceramide storage and reliably reverse or alleviate most hematological, visceral and skeletal manifestations. Although the short and intermediate term effects of GD1-specific therapies have been very gratifying, long range outcomes in terms of risk for cancer and Parkinsonism and effect of treatment on life expectancy remain to be defined. Because of the potential for oral delivery and permeation of the central nervous system, there is considerable current interest in the therapeutic use of low molecular weight compounds that either inhibit the biosynthesis of glucosylceramide (substrate reduction therapy) or that interact with and augment the intracellular activity of mutant glucocerebrosidases [120,121]. However, the current therapeutic gold standard is enzyme replacement treatment (ERT): intravenous infusion of pharmacological recombinant glucocerebrosidase that is targeted to macrophage mannose receptors and internalized to the glycolipidladen lysosomes. ERT is considered to be safe and well tolerated. Excessively rapid infusion has caused anaphylactoid-like infusion reactions as observed with other intravenous protein products [122]. Depending on the specific product prescribed, up to 15% of treated patients sero-convert although some tolerize with continued treatment. Although sero-conversion rarely causes loss of treatment efficacy, it may be associated with a higher likelihood of generally mild allergic infusion reactions that are usually preventable with pre-medication regimens. ERT in children and adults [123,124]:
- Reverses and prevents anemia and thrombocytopenia
- Reverses and prevents hepatosplenomegaly
- Decreases marrow glucocerebroside infiltration
- Prevents bones crises and reduces osteonecrosis
- Improves and prevents bone pain
- Improves bone mineral density Among GD1 patients with severe pre-treatment splenomegaly (>15 times normal), only one of 56 study patients remained so after 10 years of ERT [125]. However, in 34 of 56 patients (61%), the spleen continued to be enlarged more than 5 times normal suggesting that persistent splenic architectural abnormalities including fibrosis, scarring from infarcts, and, as mentioned previously, multiple splenic nodules long predating the inception of therapy may limit the completeness of the response [95]. Relapsing splenomegaly in a previously well controlled GD1 patient should arouse suspicion of the possibility of emergence of a secondary hematological malignancy [126].
12. SPLENECTOMY FOR HEREDITARY DISORDERS WITH MASSIVE SPLENOMEGALY
Heretofore, this discussion has concentrated exclusively on splenomegaly associated with rare hereditary disorders. The management of symptomatic splenomegaly, and, in particular, the appropriate use of splenectomy, is also a significant clinical problem in more prevalent genetic disorders such as beta-thalassemia major (TM) and hereditary spherocytosis (HS). Splenomegaly in patients with TM is often massive and usually accompanied by severe, transfusion-dependent anemia caused by ineffective erythropoiesis and chronic hemolysis due to RBC membrane damage associated with precipitation of unbound α globin chains [127]. Unlike the hypersplenism found in GD1 patients with comparable splenic enlargement, thrombocytopenia is relatively uncommon in thalassemic patients, a finding that may augment hypercoagulability that is commonly observed in patients with TM. 30 - 40 years ago, splenectomy was commonly performed in nearly 60% of thalassemic children under 10 years of age in order to reduce frequency of blood transfusion and retard iron overload [128]. By age 15 years, nearly 90% had undergone splenectomy with a resultant elimination of transfusion requirement in most TI patients and with a reduction in the need for red cell transfusions in TM patients. However, these improvement came at the expense of many splenectomy-associated complications including sepsis from encapsulated organisms (although this risk has been lessened with new protein conjugate vaccines and antibiotic prophylaxis), pulmonary hypertension, altered cytokine patterns [129] and an increased risk of thrombotic complications due to altered endothelial function attributable to larger numbers of circulating platelets and immature red cells, increased numbers of platelet derived blood microparticles, enhanced platelet activation, increases in levels of Protein C and S, and persistent post-splenectomy hemolysis [130]. Consequently, total splenectomy is now generally discouraged for children and adolescents with TM so that among children born after 1980, only 12% have had total splenectomy prior to age 20 years [128]. Partial splenectomy or radiofrequency ablation of the spleen have been proposed as alternative procedures that may be safer than total splenectomy as regards risk for infection and sepsis. However, improvement in chronic anemia and decreased transfusion dependence was less robust than in total splenectomy patients and outcomes regarding post-splenectomy complications other than infection were not reported [131,132].
Hereditary spherocytosis, transmitted as an autosomal dominant disorder and found world-wide, is the most common hemolytic anemia in northern European populations. Defects in RBC membrane proteins (e.g. ankyrin, spectrins) lead to loss of membrane surface area, reduced deformability, splenic trapping, retention and hemolytic anemia [133,134]. The spectrum of clinical severity is very broad and mildly affected individuals generally have few if any symptoms. Classical manifestations include symptomatic or asymptomatic splenomegaly, anemia, reticulocytosis, hemolytic episodes, aplastic crises, hyperbilirubinemia, cholelithiasis, decreased total and LDL cholesterol, growth failure, and skeletal changes due to erythroid hyperplasia. There is little evidence that patients with HS have an increased risk for splenic rupture and splenic infarctions rarely occur except in patients with concurrent sickle hemoglobinopathies or thrombophilia. In the past, except in the mildest cases, total splenectomy was generally advocated to arrest hemolysis and relieve symptoms due to anemia or splenomegaly, reverse growth failure or skeletal changes and prevent recurrent gall stones. However, with cumulative evidence of a significantly elevated risk for infectious complications (capsulated bacterial sepsis remaining a threat because of poor compliance with vaccination and prophylaxis regimens, babesiosis, capnocytophaga, anaplasma) as well as adverse vascular events (coronary artery disease and myocardial infarction, stroke, peripheral venous thrombosis), a more cautious attitude towards total splenectomy for HS is increasingly prevalent though still controversial [135,136]. Some issues relevant to the discussion are yet unresolved including whether splenectomy for HS confers an increased risk for pulmonary hypertension [136,137] and whether mild anemia despite ongoing hemolysis with decreased total and LDL cholesterol in pre-splenectomy patients offers any cardiovascular advantage. A review of 62 children who underwent partial splenectomy for HS between 1990-2008 indicated that most patients had a favorable initial and sustained improvement in symptoms and laboratory parameters although 5% eventually underwent total splenectomy because of splenic regeneration with recurrent anemia or abdominal pain. No patient was reported with post-splenectomy sepsis and follow up is probably yet too short for comment about symptomatic cholelithisasis and risk for cardiovascular events [138, 139].
The concern about potential adverse effects of total splenectomy on disease phenotype extends to the clinical management of patients with Gaucher disease. Among 134 consecutive patients with Type 1 GD who were screened to estimate right ventricular systolic pressure (RVSP) by Doppler echocardiography (with the caveat that consistency and accuracy relative to right heart catheterization is questionable), mild, asymptomatic PH (RVSP > 35 < 50 mmHg) was found in 30% of patients never treated with ERT and in 7.4% of treated patients. However, all patients with severe pulmonary hypertension (RVSP 50 - 130 mmHg) were surgically asplenic indicating that splenectomy is strongly associated with this life threatening manifestation of GD1 [140]. A subsequent study of 14 patients with pulmonary hypertension and hepatopulmonary syndrome confirmed that splenectomy appears to be essential to the development of this phenotype [112].
The role of splenectomy in increasing the risk for avascular necrosis (AVN) in patients with GD1 has also been controversial in the past. Those denying a causative role for splenectomy argue that patients with a splenectomy history likely have a more aggressive phenotype and are therefore more prone to complications such as AVN. However, recent data from the International Collaborative Gaucher Group Gaucher Registry indicate that splenectomy is indeed an independent risk factor for AVN. The adjusted incidence rate ratio for AVN among patients who were asplenic at the time of initiation of therapy was 2.23 (95% CI 1.61 - 3.08, P < 0.0001) compared to those who had an intact spleen [141]. Causes of death significantly more prevalent in surgically asplenic patients included chronic liver disease, septicemia, GI bleeding, pulmonary hypertension/fibrosis and post-splenectomy complications [119]. Splenectomy may predispose GD patients to portal hyper-tension, massive hepatomegaly, cirrhosis and terminal liver disease. Splenectomy may at times accelerate bone marrow infiltration leading to pancytopenia. Osteolytic lesions have been reported to appear within just a few months of splenectomy. Bone mineral densities have been found to be significantly lower in asplenic patients compared with those with an intact spleen. Orthopedic intervention in splenectomized patients carries with it a greater operative risk largely due to increased susceptibility to infection [142]. Therefore, given the availablility of effective pharmacotherapy for GD1, the consensus of opinion is that splenectomy should only be considered in exceptional circumstances after assessment by a physician experienced in the management of GD [142].
When might splenectomy nonetheless be indicated? The following examples have been suggested:
• As the only means of controlling severe thrombocytopenia accompanied by life-threatening or life-altering bleeding (e.g. retinal bleeding and possible blindness);
• To alleviate marked pressure effects (e.g. hydronephrosis) or severe cachexia, caused by massive splenomegaly;
• In the event of pathological splenic rupture that may complicate even minor trauma;
• In rare patients with autoimmune hemolytic anemia or refractory idiopathic thrombocytopenic purpura occurring on a background of Gaucher disease;
• When there is suspicion for the development of lymphoma (e.g. a growing mass in the spleen despite ERT or other GD specific treatment.
Even in these circumstances, the question might be legitimately asked whether, if feasible, partial splenectomy as with a hand-assisted laparascopic technique might be a preferable intervention to total splenectomy. Although laparascopic total splenectomy has been safely performed in patients even with massive splenomegaly with significantly less blood loss and shorter hospital stay compared to open splenectomy [4], the laparoscopic approach has not been generally adopted for a partial splenectomy because of technical difficulties. However, recent reports indicate that the hand-assisted laparoscopic approach can allow partial splenectomy as a safe and bloodless surgery for select patients, although it may not be applicable for patients with the largest spleens or who have limiting anatomical abnormalities [143]. Although classical open partial splenectomy has long been offered to patients with GD1 with variable results [144], there is as yet no report describing the outcome of laparascopic partial splenectomy followed by pharmacotherapy for the exigencies described above in patients with type 1 Gaucher disease.
13. CONCLUSION
Splenomegaly, sometimes of massive extent, occurs in a large number of hereditary diseases, some common and others, rare to ultra-rare. Although genetically and biochemically distinct, the presence of splenic enlargement and hypersplenism links these disorders not only in terms of shared symptoms, signs and laboratory abnormalities but also with respect to several challenges in clinical management. As discussed above with reference to Gaucher disease and other illustrative illnesses, these include defining indications for diagnostic splenectomy as multiplex, non-invasive biochemical and genetic tests are increasingly more accessible and affordable, continued critical appraisal of the long term benefit-risk ratio for therapeutic total splenectomy especially with the advent of disease-specific biochemical or gene replacement therapies for inborn metabolic disorders, and ongoing evaluation of the safety and efficacy of laparascopic partial splenectomy as an alternative to total splenectomy in patients with massive, even life threatening splenomegaly.Three hundred years ago, the British essayist Joseph Addison penned these lines: “Thou hast so much… spleen about thee, there is no living with thee or without thee”. Plus ça change, plus c’est la même chose!
![]()
![]()
REFERENCES
- Lamb, P.M., Lund, A., Kanagasabay, R.R., Martin, A., Webb, J.A. and Reznek, R.H. (2002) Spleen size: How well do linear ultrasound measurements correlate with three-dimensional CT volume assessments? British Journal of Radiology, 75, 573-577.
- McCorkle, R., Thomas, B., Suffaletto, H. and Jehle, D. (2010) Normative spleen size in tall healthy athletes: Implications for safe return to contact sports after infectious mononucleosis. Clinical Journal of Sport Medicine, 20, 413-415. doi:10.1097/JSM.0b013e3181f35fe5
- Spielmann, A.L., DeLong, D.M. and Kliewer, M.A. (2005) Sonographic evaluation of spleen size in tall healthy athletes. AJR American Journal of Roentgenology Diagnostic Imaging and Related Sciences, 184, 45-49.
- Kercher, K.W., Matthews, B.D., Walsh, R.M., Sing, R.F., Backus, C.L. and Heniford, B.T. (2002) Laparoscopic splenectomy for massive splenomegaly. The American Journal of Surgery, 183, 192-196. doi:10.1016/S0002-9610(01)00874-1
- Swanson, T.W., Meneghetti, A.T., Sampath, S., Connors, J.M. and Panton, O.N. (2011) Hand-assisted laparoscopic splenectomy versus open splenectomy for massive splenomegaly: 20-year experience at a Canadian centre. Canadian Journal of Surgery, 54, 189-193. doi:10.1503/cjs.044109
- Zhu, J., Ye, H., Wang, Y., Zhao, T., Zhu, Y., Xie, Z., Liu, J., Wang, K., Zhan, X. and Ye, Z. (2011) Laparoscopic versus open pediatric splenectomy for massive splenomegaly. Surgical Innovation, 18, 349-353.
- Gielchinsky, Y., Elstein, D., Hadas-Halpern, I., Lahad, A., Abrahamov, A. and Zimran, A. (1999) Is there a correlation between degree of splenomegaly, symptoms and hypersplenism? A study of 218 patients with Gaucher disease. British Journal of Haematology, 106, 812-816. doi:10.1046/j.1365-2141.1999.01616.x
- Hollak, C., Belmatoug, N., Cole, J.A., Vom Dahl, S., Deegan, P.B., Goldblatt, J., Rosenbloom, B., van Dussen, L., Tylki-Szymańska, A., Weinreb, N.J., Zimran, A. and Cappellini, M.D. (2012) Clinical characteristics associated with persisting thrombocytopenia in type 1 Gaucher patients treated with imiglucerase for 4 to 5 years. British Journal of Haematology, 158, 528-538. doi:10.1111/j.1365-2141.2012.09175.x
- Jaroch, M.T., Broughan, T.A. and Hermann, R.E. (1986) The natural history of splenic infarction. Surgery, 100, 743-750.
- Chin, J.K.T., McCormick, P.A., Hilson, A.J.W., Burroughs, A.K. and McIntyre, N. (1993) Liver/spleen scintigraphy for diagnosis of splenic infarction in cirrhotic patients. Postgraduate Medical Journal, 69, 715-717. doi:10.1136/pgmj.69.815.715
- Ustun, C., Kutlar, F., Holley, L., Seigler, M., Burgess, R. and Kutlar, A. (2003) Interaction of sickle cell trait with hereditary spherocytosis: Splenic infarcts and sequestration. Acta Haematol, 109, 46-49. doi:10.1159/000067273
- Breuer, C., Janssen, G., Laws, H.J., Schaper, J., Mayatepek, E., Schroten, H. and Tenenbaum, T. (2008) Splenic infarction in a patient hereditary spherocytosis, protein C deficiency and acute infectious mononucleosis. European Journal of Pediatrics, 167, 1449-1452. doi:10.1007/s00431-008-0781-3
- Park, M.Y., Kim, J.A., Yi, S.Y., Chang, S.H., Um, T.H. and Lee, H.R. (2011) Splenic infarction in a patient with autoimmune hemolytic anemia and protein C deficiency. The Korean Journal of Hematology, 46, 274-278.
- Gilbert, H.S. (1985) Myeloproliferative disorders. Clinics in Geriatric Medicine, 1, 773-93.
- Spangler, W.L. and Kass, P.H. (1999) Splenic myeloid metaplasia, histiocytosis, and hypersplenism in the dog (65 cases). Veterinary Pathology, 36, 583-593. doi:10.1354/vp.36-6-583
- Fishman, D. and Isenberg, D.A. (1997) Splenic involvement in rheumatic diseases. Seminars in Arthritis and Rheumatism, 27, 141-155. doi:10.1016/S0049-0172(97)80013-3
- Hadary, A., Dashkowsky, I., Rapaport, A. and Cozakov, J.C. (2008) Non-traumatic rupture of spleen: Can splenectomy be applied selectively? The Israel Medical Association Journal, 10, 889-891.
- Beutler, E. and Grabowski, G.A. (2001) Gaucher disease. In: Scriver, C.R., Beaudet, A.L., Sly, W.S., and Valle, D., Eds., The Metabolic and Molecular Bases of Inherited Disease. McGraw-Hill, New York, 3635-3668.
- Stone, D.L., Ginns, E.I., Krasnewich, D. and Sidransky, E. (2000) Life-threatening splenic hemorrhage in two patients with Gaucher disease. American Journal of Hematology, 64, 140-142. doi:10.1002/(SICI)1096-8652(200006)64:2<140::AID-AJH14>3.0.CO;2-T
- Dingli, D., Mesa, R.A. and Tefferi, A. (2004) Myelofibrosis with myeloid metaplasia; new developments in pathogenesis and treatment. Internal Medicine Journal, 43, 540-547. doi:10.2169/internalmedicine.43.540
- El-Shazly, M.A. and Okello, D.O. (1994) Tropical splenomegaly syndrome: Who gets oesophageal varices? East African Medical Journal, 71, 768-770.
- Watanabe, Y., Mizukami, T., Egawa, T., Okamoto, S., Sakauchi, M., Takita, T., Suzuki, N. and Sakuma, M. (1999) A case of progressive systemic sclerosis complicated by idiopathic portal hypertension with severe anemia. Ryumachi, 39, 586-590.
- Seçil, M., Göktay, A., Dicle, O. and Pirnar, T. (2001) Splenic vascular malformations and portal hypertension in hereditary hemorrhagic telangiectasia: Sonographic findings. Journal of Clinical Ultrasound, 29, 56-59. doi:10.1002/1097-0096(200101)29:1<56::AID-JCU10>3.0.CO;2-O
- Gusberg, R.J., Peterec, S.M., Sumpio, B.E. and Meier, G.H. (1994) Splenomegaly and variceal bleeding—Hemodynamic basis and treatment implications. Hepatogastroenterology, 41, 573-577.
- Singh, I.K., Bhatnagar, V., Gupta, A.K. and Seith, A. (2011) Correlation of splenic volume with hematological parameters, splenic vein diameter, portal pressure and grade of varices in extrahepatic portal vein obstruction in children. Pediatric Surgery International, 27, 467-471. doi:10.1007/s00383-010-2847-3
- James, S.P., Stromeyer, F.W., Stowens, D.W. and Barranger, J.A. (1982) Gaucher disease: Hepatic abnormalities in 25 patients. Progress in Clinical and Biological Research, 95, 131-142.
- Bandyopadhyay, R., Bandyopadhyay, S. and Maity, P.K. (2011) Gauchers disease presenting with portal hypertension. Indian Pediatr, 48, 801-802.
- Jacobs, P., Maze, S., Tayob, F. and Harries-Jones, E.P. (1985) Myelofibrosis, splenomegaly, and portal hypertension. Acta Haematol, 74, 45-48. doi:10.1159/000206164
- Aessopos, A., Farmakis, D., Deftereos, S., Tsironi, M., Polonifi, A., Moyssakis, I., Diamanti-Kandaraki, E. and Papalambros, E. (2005) Cardiovascular effects of splenomegaly and splenectomy in beta-thalassemia. Annals of Hematology, 84, 353-357. doi:10.1007/s00277-004-1002-4
- Farmakis, D. and Aessopos, A. (2011) Pulmonary hypertension associated with hemoglobinopathies: Prevalent but overlooked. Circulation, 123, 1227-1232. doi:10.1161/CIRCULATIONAHA.110.988089
- Smedema, J.P. and Louw, V.J. (2007) Pulmonary arterial hypertension after splenectomy for hereditary spherocytosis. Cardiovascular Journal of Africa, 18, 84-89.
- Crary, S.E., Ramaciotti, C. and Buchanan, G.R. (2011) Prevalence of pulmonary hypertension in hereditary spherocytosis. American Journal of Hematology, 86, E73-E76. doi:10.1002/ajh.22182
- García-Manero, G., Schuster, S.J., Patrick, H. and Martinez, J. (1999) Pulmonary hypertension in patients with myelofibrosis secondary to myeloproliferative diseases. American Journal of Hematology, 60, 130-135. doi:10.1002/(SICI)1096-8652(199902)60:2<130::AID-AJH8>3.0.CO;2-Z
- Ziakas, P.D., Voulgarelis, M., Felekouras, E., Anagnostou, D. and Tzelepis, G.E. (2005) Myelofibrosis-associated massive splenomegaly: A cause of increased intra-abdominal pressure, pulmonary hypertension, and positional dyspnea. American Journal of Hematology, 80, 128-132. doi:10.1002/ajh.20388
- Hadj-Moussa, M. and Brown, J.A. (2010) Reversible renal insufficiency secondary to extrinsic splenic compression of the kidney in a patient with chronic lymphocytic leukemia. Scientific World Journal, 4, 796-798. doi:10.1100/tsw.2010.74
- Mistry, P.K., Sadan, S., Yang, R., Yee, J. and Yang, M. (2007) Consequences of diagnostic delays in type 1 Gaucher disease: The need for greater awareness among hematologists-oncologists and an opportunity for early diagnosis and intervention. American Journal of Hematology, 82, 697-701. doi:10.1002/ajh.20908
- Gunay-Aygun, M., Zivony-Elboum, Y., Gumruk, F., Geiger, D., Cetin, M., Khayat, M., Kleta, R., Kfir, N., Anikster, Y., Chezar, J., Arcos-Burgos, M., Shalata, A., Stanescu, H., Manaster, J., Arat, M., Edwards, H., Freiberg, A.S., Hart, P.S., Riney, L.C., Patzel, K., Tanpaiboon, P., Markello, T., Huizing, M., Maric, I., Horne, M., Kehrel, B.E., Jurk, K., Hansen, N.F., Cherukuri, P.F., Jones, M., Cruz, P., Mullikin, J.C., Nurden, A., White, J.G., Gahl, W.A. and Falik-Zaccai, T. (2010) Gray platelet syndrome: natural history of a large patient cohort and locus assignment to chromosome 3p. Blood, 116, 4990- 5001. doi:10.1182/blood-2010-05-286534
- Gunay-Aygun, M., Falik-Zaccai, T.C., Vilboux, T., Zivony-Elboum, Y., Gumruk, F., Cetin, M., Khayat, M., Boerkoel, C.F., Kfir, N., Huang, Y., Maynard, D., Dorward, H., Berger, K., Kleta, R., Anikster, Y., Arat, M., Freiberg, A.S., Kehrel, B.E., Jurk, K., Cruz, P., Mullikin, J.C., White, J.G., Huizing, M. and Gahl, W.A. (2011) NBEAL2 is mutated in gray platelet syndrome and is required for biogenesis of platelet α-granules. Nature Genetics, 43, 732-734. doi:10.1038/ng.883
- Zittoun, J., Zittoun, R., Marquet, J. and Sultan, C. (1975) The three transcobalamins in myeloproliferative disorders and acute leukaemia. British Journal of Haematology, 31, 287-298. doi:10.1111/j.1365-2141.1975.tb00860.x
- Rao, V.K. and Oliveira, J.B. (2011) How I treat autoimmune lymphoproliferative syndrome. Blood, 118, 5741- 5751. doi:10.1182/blood-2011-07-325217
- Takahashi, K., Terashima, K., Kojima, M., Yoshida, H. and Kimura, H. (1977) Pathological, histochemical and ultrastructural studies on sea-blue histiocytes and Gaucher-like cells in acquired lipidosis occurring in leukemia. Acta Pathologica Japonica, 27, 775-797.
- Mason, B.A., Bowers, G.R., Guccion, J.G. and Schechter, G.P. (1978) Sea-blue histiocytes in a patient with lymphoma. American Journal of Medicine, 64, 515-518. doi:10.1016/0002-9343(78)90245-0
- Lasser, A. (1983) Diffuse histiocytosis of the spleen and idiopathic thrombocytopenic purpura (ITP): Histochemical and ultrastructural studies. American Journal of Clinical Pathology, 80, 529-533.
- Hirayama, Y., Kohda, K., Andoh, M., Matsumoto, S., Nakazawa, O., Nobuoka, A., Mochizuki, C., Takayanagi, N. and Ezoe, A. (1996) Syndrome of the sea-blue histiocyte. Internal Medicine Journal, 35, 419-421. doi:10.2169/internalmedicine.35.419
- Norum, R.A., Lakier, J.B., Goldstein, S., Angel, A., Goldberg, R.B., Block, W.D., Noffze, D.K., Dolphin, P.J., Edelglass, J., Bogorad, D.D. and Alaupovic, P. (1982) Familial deficiency of apolipoproteins A-I and C-III and precocious coronary-artery disease. The New England Journal of Medicine, 306, 1513-1519. doi:10.1056/NEJM198206243062503
- Sorci-Thomas, M.G. and Thomas, M.J. (2002) The effects of altered apolipoprotein A-I structure on plasma HDL concentration. Trends in Cardiovascular Medicine, 12, 121-128. doi:10.1016/S1050-1738(01)00163-3
- Remaley, A.T., Rust, S., Rosier, M., Knapper, C., Naudin, L., Broccardo, C., Peterson, K.M., Koch, C., Arnould, I., Prades, C., Duverger, N., Funke, H., Assman, G., Dinger, M., Dean, M., Chimini, G., Santamarina-Fojo, S., Fredrickson, D.S., Denefle, P. and Brewer, H.B. Jr. (1999) Human ATP-binding cassette transporter 1 (ABC1): Genomic organization and identification of the genetic defect in the original Tangier disease kindred. Proceedings of the National Academy of Sciences, 96, 12685-12690. doi:10.1073/pnas.96.22.12685
- Nguyen, T.T., Kruckeberg, K.E., O’Brien, J.F., Ji, Z.S., Karnes, P.S., Crotty, T.B., Hay, I.D., Mahley, R.W. and O’Brien, T. (2000) Familial splenomegaly: macrophage hypercatabolism of lipoproteins associated with apolipoprotein E mutation [apolipoprotein E (delta 149 Leu)]. The Journal of Clinical Endocrinology & Metabolism, 85, 4354-4358. doi:10.1210/jc.85.11.4354
- Naghashpour, M. and Cualing, H. (2009) Splenomegaly with sea-blue histiocytosis, dyslipidemia, and nephropathy in a patient with lecithin-cholesterol acyltransferase deficiency: A clinicopathologic correlation. Metabolism, 58, 1459-1464. doi:10.1016/j.metabol.2009.04.033
- Khera, A.V., Cuchel, M., de la Llera-Moya, M., Rodrigues, A., Burke, M.F., Jafri, K., French, B.C., Phillips, J.A., Mucksavage, M.L., Wilensky, R.L., Mohler, E.R., Rothblat, G.H. and Rader, D.J. (2011) Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. The New England Journal of Medicine, 364, 127-135 doi:10.1056/NEJMoa1001689.
- Savel, J., Lafitte, M., Pucheu, Y., Pradeau, V., Tabarin, A. and Couffinhal, T. (2012) Very low levels of HDL cholesterol and atherosclerosis, a variable relationship—A review of LCAT deficiency. Journal of Vascular Health and Risk Management, 8, 357-361.
- Beaudet, A.L., Ferry, G.D., Nichols, B.L. and Rosenberg, H.A. (1977) Cholesterol ester storage disease: Clinical, biochemical, and pathological studies. Pediatrics, 90, 910-914. doi:10.1016/S0022-3476(77)80557-X
- Elleder, M., Chlumska, A., Hyanek, J., Poupetova, H., Ledvinova, J., Maas, S. and Lohse, P. (2000) Subclinical course of cholesteryl ester storage disease in an adult with hypercholesterolemia, accelerated atherosclerosis, and liver cancer. Journal of Hepatology, 32, 528-534. doi:10.1016/S0168-8278(00)80407-9
- vom Dahl, S., Harzer, K., Rolf, A., Albrecht, B., Niderau, C., Vogt, C., van S. Weely, S., aerts J, Muller, G. and Haussinger, D. (1999) Hepatosplenomegalic lipidosis: What unless Gaucher? Adult cholesteryl ester storage disease (CESD) with anemia, lipodystrophy, increased plasma chitotriosidase activity and homozygous lysosomal acid lipase—2 exon 8 splice junction mutation. Journal of Hepatology, 31, 741-746.
- Anderson, R.A., Bryson, G.M. and Parks, J.S. (1999) Lysosomal acid lipase mutations that determine phenotype in Wolman and cholesterol ester storage disease’. Molecular Genetics and Metabolism, 68, 333-345. doi:10.1006/mgme.1999.2904
- Tadiboyina VT, Liu DM, Miskie BA, Wang J, Hegele RA. (2005) Treatment of dyslipidemia with lovastatin and ezetimibe in an adolescent with cholesterol ester storage disease. Lipids in Health and Disease, 4, 26. doi:10.1186/1476-511X-4-26
- Hansen, K. and Horslen, S. (2008) Metabolic liver disease in children. Liver Transplantation, 14, 713-733. doi:10.1002/lt.21520
- Sévin, M., Lesca, G., Baumann, N., Millat, G., LyonCaen, O., Vanier, M.T. and Sedel, F. (2007) The adult form of Niemann-Pick disease type C. Brain, 130, 120- 133.
- Zhou, S., Davidson, C., McGlynn, R., Stephney, G., Dobrenis, K., Vanier, M.T. and Walkley, S.U. (2011) Endosomal/lysosomal processing of gangliosides affects neuronal cholesterol sequestration in Niemann-Pick disease type C. American Journal of Pathology, 179, 890- 902. doi:10.1016/j.ajpath.2011.04.017
- [61] Malnar, M., Kosicek, M., Mitterreiter, S., Omerbasic, D., Lichtenthaler, S.F., Goate, A. and Hecimovic, S. (2010) Niemann-Pick type C cells show cholesterol dependent decrease of APP expression at the cell surface and its increased processing through the beta-secretase pathway. Biochimica et Biophysica Acta, 1802, 682-691. doi:10.1016/j.bbadis.2010.05.006
- [62] Patterson, M.C., Hendriksz, C.J., Walterfang, M., Sedel, F., Vanier, M.T. and Wijburg, F. (2012) On behalf of the NP-C Guidelines Working Group. Recommendations for the diagnosis and management of Niemann-Pick disease type C: An update. Molecular Genetics and Metabolism, 106, 330-344. doi:10.1016/j.ymgme.2012.03.012
- [63] Benko, W., Ries, M., Wiggs, E.A., Brady, R.O., Schiffmann, R. and Fitzgibbon, E.J. (2011) The saccadic and neurological deficits in type 3 Gaucher disease. PLoS One, 6, e22410. doi:10.1371/journal.pone.0022410
- [64] Wraith, J.E. and Imrie, J. (2009) New therapies in the management of Niemann-Pick type C disease: Clinical utility of miglustat. Journal of Therapeutics and Clinical Risk Management, 5, 877-887. doi:10.2147/TCRM.S5777
- [65] Chien, Y.H., Lee, N.C., Tsai, L.K., Huang, A.C., Peng, S.F, Chen, S.J. and Hwu, W.L. (2007) Treatment of Niemann-Pick disease type C in two children with miglustat: Initial responses and maintenance of effects over 1 year. Journal of Inherited Metabolic Disease, 30, 826. doi:10.1007/s10545-007-0630-y
- [66] Zarowski, M., Steinborn, B., Gurda, B., Dvorakova, L., Vlaskova, H. and Kothare, S.V. (2011) Treatment of cataplexy in Niemann-Pick disease type C with the use of miglustat. European Journal of Paediatric Neurology, 15, 84-87. doi:10.1016/j.ejpn.2010.02.001
- [67] Nietupski, J.B., Pacheco, J.J., Chuang, W.L., Maratea, K., Li, L., Foley, J., Ashe, K.M., Cooper, C.G., Aerts, J.M., Copeland, D.P., Scheule, R.K., Cheng, S.H. and Marshall, J. (2012) Iminosugar-based inhibitors of glucosylceramide synthase prolong survival but paradoxically increase brain glucosylceramide levels in Niemann-Pick C mice. Molecular Genetics and Metabolism, 105, 621-628. doi:10.1016/j.ymgme.2012.01.020
- [68] Davidson, C.D., Ali, N.F., Micsenyi, M.C., Stephney, G., Renault, S., Dobrenis, K., Ory, D.S., Vanier, M.T. and Walkley, S.U. (2009) Chronic cyclodextrin treatment of murine Niemann-Pick C disease ameliorates neuronal cholesterol and glycosphingolipid storage and disease progression. PLoS One, 4, e6951. doi:10.1371/journal.pone.0006951
- [69] Wasserstein, M.P., Desnick, R.J., Schuchman, E.H., Hossain, S., Wallenstein, S., Lamm, C. and McGovern M.M. (2004) The natural history of type B Niemann-Pick disease: Results from a 10-year longitudinal study. Pediatrics, 114, e672-e677. doi:10.1542/peds.2004-0887
- [70] McGovern, M.M., Wasserstein, M.P., Giugliani, R., Bembi, B., Vanier, M.T., Mengel, E., Brodie, S.E., Mendelson, D., Skloot, G., Desnick, R.J., Kuriyama, N. and Cox, G.F. (2008) A prospective, cross-sectional survey study of the natural history of Niemann-Pick disease type B. Pediatrics, 122, e341-e349. doi:10.1542/peds.2007-3016
- [71] Hollak, C.E., de Sonnaville, E.S., Cassiman, D., Linthorst, G.E., Groener, J.E., Morava, E., Wevers, R.A., Mannens, M., Aerts, J.M., Meersseman, W., Akkerman, E., NiezenKoning, K.E., Mulder, M.F., Visser, G., Wijburg, F.A., Lefeber, D. and Poorthuis, B.J. (2012) Acid sphingomyelinase (Asm) deficiency patients in the Netherlands and Belgium: Disease spectrum and natural course in attenuated patients. Molecular Genetics and Metabolism, 107, 526-533. doi:10.1016/j.ymgme.2012.06.015
- [72] Simpson, W.L. Jr, Mendelson, D., Wasserstein, M.P. and McGovern, M.M. (2010) Imaging manifestations of Niemann-Pick disease type B. AJR American Journal of Roentgenology Diagnostic Imaging and Related Sciences, 194, W12-W19. doi:10.2214/AJR.09.2871
- [73] Charrow, J., Andersson, H.C., Kaplan, P., Kolodny, E.H., Mistry, P., Pastores, G., Rosenbloom, B.E., Scott, C.R., Wappner, R.S., Weinreb, N.J. and Zimran, A. (2000) The Gaucher registry: Demographics and disease characteristics of 1698 patients with Gaucher disease. Archives of Internal Medicine, 160, 2835-2843. doi:10.1001/archinte.160.18.2835
- [74] Kaplan, P., Andersson, H.C., Kacena, K.A. and Yee, J.D. (2006) The clinical and demographic characteristics of nonneuronopathic Gaucher disease in 887 children at diagnosis. Archives of Pediatrics & Adolescent Medicine, 160, 603-608. doi:10.1001/archpedi.160.6.603
- [75] Cordeau, M.P., Prosmanne, O. and Robillard, P. (1990) Case of the day. Noncirrhotic idiopathic portal hypertension (Banti syndrome). Radiographics, 10, 114-116.
- [76] Vos, B., Moreno, C., Nagy, N., Féry, F., Cnop, M., Vereerstraeten, P., Devière, J. and Adler, M. (2011) Lean non-alcoholic fatty liver disease (Lean-NAFLD): A major cause of cryptogenic liver disease. Acta Gastro-Enterologica Belgica, 74, 389-394.
- [77] Emami, M.H., Hashemi, M., Kouhestani, S., Taheri, H. and Karimi, S. (2012) Should we look for celiac disease among all patients with liver function test abnormalities? International Journal of Preventive Medicine, 3, 167-172.
- [78] Horai, Y., Miyamura, T., Hirata, A., Nakamura, M., Takahama, S., Ando, H., Minami, R., Yamamoto, M. and Suematsu, E. (2010) Idiopathic portal hypertension in a patient with mixed connective tissue disease and protein C deficiency. Internal Medicine Journal, 49, 2013-2016. doi:10.2169/internalmedicine.49.3834
- [79] Castiella, A. (2012) Iron overload and HFE mutations: Are they relevant in cryptogenic cirrhosis? Hepatitis Monthly, 12, 126-127.
- [80] Stathakis, N.E., Papayannis, A.G., Dervenoulas, J., Scliros, P. and Gardikas, C. (1974) Multiple coagulation abnormalities in a case of cryptogenic splenomegaly. BMJ, 4, 142-143. doi:10.1136/bmj.4.5937.142
- [81] Dacie, J.V., Galton, D.A., Gordon-Smith, E.C. and Harrison, C.V. (1978) Non-tropical idiopathic splenomegaly: A follow-up study of ten patients described in 1969. British Journal of Haematology, 38, 185-193. doi:10.1111/j.1365-2141.1978.tb01035.x
- [82] Stahel, R.A., Maurer, R., Cavalli, F. and Fehr, J. (1982) Idiopathic splenomegaly: The preliminary stage of a malignant lymphoma? Report on 2 Cases Schweiz Med Wochenschr, 112, 725-730.
- [83] Letoquart, J.P., Casa, C., Grosbois, B., Pompilio, M., Chaperon, J., Lancien, G., Jacomy, D., Leblay, R. and Mambrini, A. (1990) Diagnostic splenectomy. Apropos of 38 Cases Ann Chir, 44, 342-347.
- [84] Tantravahi, S.K., Williams, L.B., Digre, K.B., Creel, D.J., Smock, K.J., DeAngelis, M.M., Clayton, F.C., Vitale, A.T. and Rodgers, G.M. (2012) An inherited disorder with splenomegaly, cytopenias, and vision loss. American Journal of Medical Genetics Part A, 158A, 475-481. doi:10.1002/ajmg.a.34437
- [85] WHONAMEDIT? (2013) A dictionary of medical eponyms. http://www.whonamedit.com/doctor.cfm/498.html
- [86] Gaucher, P.C.E. (1885) De l’epithelioma primitive de las rate, hypertrophie idiopathique de la rate sans leucemie. Academic Thesis, Paris.
- [87] Brill, N.E., Mandlebaum, F.S. and Libman, E. (1901) Primary splenomegaly-Gaucher type. Mount Sinai Hospital Reports, 4, 35-48.
- [88] Kaplan, P., Baris, H., De Meirleir, L., Di Rocco, M., El-Beshlawy, A., Huemer, M., Martins, A.M., Nascu, I., Rohrbach, M., Steinbach, L. and Cohen, I.J. (2012) Revised recommendations for the management of Gaucher disease in children. European Journal of Pediatrics, July 8. doi:10.1007/s00431-012-1771-z
- [89] Rosenbloom, B., Balwani. M., Bronstein, J.M., Kolodny, E., Sathe, S., Gwosdow, A.R., Taylor, J.S., Cole, J.A., Zimran, A. and Weinreb, N.J. (2011) The incidence of Parkinsonism in patients with type 1 Gaucher disease: Data from the ICGG Gaucher Registry. Blood Cells, Molecules and Diseases, 46, 95-102. doi:10.1016/j.bcmd.2010.10.006
- [90] Biegstraaten, M., Mengel, E., Marodi, L., Petakov, M., Niederau, C., Giraldo, P., Hughes, D., Mrsic, M., Mehta, A., Hollak, C.E. and van Schaik, I.N. (2010) Peripheral neuropathy in adult type 1 Gaucher disease: A 2-year prospective observational study. Brain, 133, 2009-2919. doi:10.1093/brain/awq198
- [91] Grabowski, G.A. (1997) Gaucher disease: Gene frequentcies and genotype/phenotype correlations. Genetic Testing and Molecular Biomarkers, 1, 5-12.
- [92] Lachmann, R.H., Grant, I.R., Halsall, D. and Cox, T.M. (2004) Twin pairs showing discordance of phenotype in adult Gaucher’s disease. QJM, 97, 199-204. doi:10.1093/qjmed/hch036
- [93] Beutler, E. (1977) Gaucher disease in an asymptomatic 72 year old. JAMA, 237, 2529 doi:10.1001/jama.1977.03270500081038
- [94] Allen, M.J., Myer, B.J. Khokher, A.M., Rushton, N. and Cox, T.M. (1997) Pro-inflammatory cytokines and the pathogenesis of Gaucher’s disease: Increased release of interleukin-6 and interleukin-10. QJM, 90, 19-25. doi:10.1093/qjmed/90.1.19
- [95] Hollak, C.E., Evers, L., Aerts, J.M. and van Oers, M.H. (1997) Elevated levels of M-CSF, sCD14 and IL8 in type 1 Gaucher disease. Blood Cells, Molecules and Diseases, 23, 201-212. doi:10.1006/bcmd.1997.0137
- [96] Stein, P., Malhotra, A., Haims, A., Pastores, G.M. and Mistry, P.K. (2010) Focal splenic lesions in type I Gaucher disease are associated with poor platelet and splenic response to macrophage-targeted enzyme replacement therapy. Journal of Inherited Metabolic Disease, 33, 769-774. doi:10.1007/s10545-010-9175-6
- [97] Mistry, P.K., Liu, J., Yang, M., Nottoli, T., McGrath, J., Jain, D., Zhang, K., Keutzer, J., Chuang, W.L., Mehal, W.Z., Zhao, H., Lin, A., Mane, S., Liu, X., Peng, Y.Z., Li, J.H., Agrawal, M., Zhu, L.L., Blair, H.C., Robinson, L.J., Iqbal, J., Sun, L. and Zaidi, M. (2010) Glucocerebrosidase gene-deficient mouse recapitulates Gaucher disease displaying cellular and molecular dysregulation beyond the macrophage. Proceedings of the National Academy of Sciences, 107, 19473-19478. doi:10.1073/pnas.1003308107
- [98] Lecourt, S., Vanneaux, V., Cras, A., Freida, D., Heraoui, D., Herbi, L., Caillaud, C., Chomienne, C., Marolleau, J.P., Belmatoug, N. and Larghero, J. (2012) Bone marrow microenvironment in an in vitro model of Gaucher disease: Consequences of glucocerebrosidase deficiency. Stem Cells and Development, 21, 239-248 doi:10.1089/scd.2011.0365
- [99] Rosenbloom, B.E., Kulke, S., Taylor, J. and Weinreb, N.J. (2011) Thrombocytopenia in the absence of splenomegaly in patients with type 1 Gaucher disease: A preliminary analysis from the ICGG Gaucher Registry. Blood, 118, 1802-1803.
- [100] Spectre, G., Roth, B., Ronen, G., Rosengarten, D., Elstein, D., Zimran, A., Varon, D. and Revel-Vilk, S. (2011) Platelet adhesion defect in type 1 Gaucher disease is associated with a risk of mucosal bleeding. British Journal of Haematology, 153, 372-378. doi:10.1111/j.1365-2141.2011.08613.x
- [101] Shitrit, D., Rudensky, B., Zimran, A. and Elstein, D. (2003) D-dimer assay in Gaucher disease: Correlation with severity of bone and lung involvement. American Journal of Hematology, 73, 236-239. doi:10.1002/ajh.10361
- [102] Sherif, E.M., Tantawy, A.A., Adly, A.A., Kader, H.A. and Ismail, E.A. (2011) D-dimer assay in Egyptian patients with Gaucher disease: Correlation with bone and lung involvement. Blood Coagul Fibrinolysis, 22, 176- 184. doi:10.1097/MBC.0b013e3283424809
- [103] Wenstrup, R.J., Roca-Espiau, M., Weinreb, N.J. and Bembi, B. (2002) Skeletal aspects of Gaucher disease: A review. British Journal of Radiology, 75, A2-A12.
- [104] Deegan, P.B., Pavlova, E., Tindall, J., Stein, P.E., Bearcroft, P., Mehta, A., Hughes, D., Wraith, J.E. and Cox, T.M. (2011) Osseous manifestations of adult Gaucher disease in the era of enzyme replacement therapy. Medicine (Baltimore), 90, 52-60. doi:10.1097/MD.0b013e3182057be4
- [105] Khan, A., Hangartner, T., Weinreb, N.J., Taylor, J.S. and Mistry, P.K. (2012) Risk factors for fractures and avascular osteonecrosis in type 1 Gaucher disease—A study from the International Collaborative Gaucher Group (ICGG) Gaucher Registry. Journal of Bone and Mineral Research, 27, 1839-1848. doi:10.1002/jbmr.1680
- [106] Maas, M., van Kuijk, C., Stoker, J., Hollak, C.E., Akkerman, E.M., Aerts, J.F. and den Heeten, G.J. (2003) Quantification of bone involvement in Gaucher disease: MR imaging bone marrow burden score as an alternative to Dixon quantitative chemical shift MR imaging—Initial experience. Radiology, 229, 554-561. doi:10.1148/radiol.2292020296
- [107] Poll, L.W., vom Dahl, S., Koch, J.A., Bӧrner, D., Willes, R., Cohnen, M., Jung, G., Scherer, A., Niederau, C., Haȕssinger, D. and Mȍdder, U. (2001) Gaucher disease: MR evaluation of bone marrow features during treatment with enzyme replacement. ROFO, 173, 931-937. doi:10.1055/s-2001-17593
- [108] Mistry, P.K., Weinreb, N., Kaplan, P., Cole, J.A., Gwosdow, A.R. and Hangartner, T. (2011) Osteopenia in Gaucher disease develops early in life: Response to imiglucerase enzyme therapy in children, adolescents and adults. Blood Cells, Molecules and Diseases, 46, 66-72. doi:10.1016/j.bcmd.2010.10.011
- [109] Kaplan, P., Mazur, A., Manor, O., Charrow, J., Esplin, J., Gribble, T.J., Wappner, R.S., Wisch, J.S. and Weinreb, N.J. (1996) Acceleration of retarded growth in children with Gaucher disease after treatment with alglucerase. Journal of Pediatrics, 129, 149-153. doi:10.1016/S0022-3476(96)70203-2
- [110] Kauli, R., Zaizov, R., Lazar, L., Pertzelan, A., Laron, Z., Galatzer, A., Phillip, M., Yaniv, Y. and Cohen, I.J. (2000) Delayed growth and puberty in patients with Gaucher disease type 1: Natural history and effect of splenectomy and/or enzyme replacement therapy. The Israel Medical Association Journal, 2, 158-163.
- [111] Ross, D.J., Spira, S. and Buchbinder, N.A. (1997) Gaucher cells in pulmonary—Capillary blood in association with pulmonary hypertension. The New England Journal of Medicine, 336, 379-381. doi:10.1056/NEJM199701303360516
- [112] Kim, J.H., Park, C.H., Pai, M.S., Hahn, M.H. and Kim, H.J. (1999) Hepatopulmonary syndrome in Gaucher disease with right-to-left shunt: Evaluation and measurement using Tc-99m MAA. Clinical Nuclear Medicine, 24, 164-166. doi:10.1097/00003072-199903000-00005
- [113] Lo, S.M., Liu, J., Chen, F., Pastores, G.M., Knowles, J., Boxer, M., Aleck, K. and Mistry, P.K. (2011) Pulmonary vascular disease in Gaucher disease: Clinical spectrum, determinants of phenotype and long-term outcomes of therapy. Journal of Inherited Metabolic Disease, 34, 643- 650.
- [114] Anheim, M., Elbaz, A., Lesage, S., Durr, A., Condroyer, C., Viallet, F., Pollak, P., Bonaïti, B., Bonaïti-Pellié, C., Brice, A. (2012) French Parkinson disease genetic group. Penetrance of Parkinson disease in glucocerebrosidase gene mutation carriers. Neurology, 78, 417-420. doi:10.1212/WNL.0b013e318245f476
- [115] Rosenbloom, B.E., Weinreb, N.J., Zimran, A., Kacena, K.A., Charrow, J. and Ward, E. (2005) Gaucher disease and cancer incidence: A study from the Gaucher registry. Blood, 105, 4569-4572. doi:10.1182/blood-2004-12-4672
- [116] de Fost, M., vom Dahl, S., Weverling, G.J., Brill, N., Brett, S., Haȕssinger, D. and Hollak, C.E. (2006) Increased incidence of cancer in adult Gaucher disease in Western Europe. Blood Cells, Molecules and Diseases, 36, 53-58. doi:10.1016/j.bcmd.2005.08.004
- [117] Lo, S.M., Stein, P., Mullaly, S., Bar, M., Jain, D., Pastores, G.M. and Mistry, P.K. (2010) Expanding spectrum of the association between Type 1 Gaucher disease and cancers: a series of patients with up to 3 sequential cancers of multiple types—Correlation with genotype and phenotype. American Journal of Hematology, 85, 340- 345.
- [118] Choy, F.Y. and Campbell, T.N. (2011) Gaucher disease and cancer: Concept and controversy. International Journal of Cell Biology, 150450.
- [119] Weinreb, N.J., Deegan, P., Kacina, K.A., Mistry, P., Pastores, G.M., Velentgas, P. and Vom Dahl, S. (2008) Life expectancy in Gaucher disease type 1. American Journal of Hematology, 83, 896-900. doi:10.1002/ajh.21305
- [120] Weinreb, N.J., Barbouth, D. and Lee, R.E. (2011) Causes of death in 184 patients with type 1 Gaucher disease from the United States who were never treated with enzyme replacement therapy. Blood, 118, 1351-3152.
- [121] Smid, B.E., Aerts, J.M., Boot, R.G., Linthorst, G.E. and Hollak, C.E. (2010) Pharmacological small molecules for the treatment of lysosomal storage disorders. Expert Opinion on Investigational Drugs, 19, 1367-1379. doi:10.1517/13543784.2010.524205
- [122] Lukina, E., Watman, N., Arreguin, E.A., Dragosky, M., Iastrebner, M., Rosenbaum, H., Phillips, M., Pastores, G.M., Kamath, R.S., Rosenthal, D.I., Kaper, M., Singh, T., Puga, A.C. and Peterschmitt, M.J. (2010) Improvement in hematological, visceral, and skeletal manifestations of Gaucher disease type 1 with oral eliglustat tartrate (Genz-112638) treatment—2 years results of a phase 2 study. Blood, 116, 4095-4098. doi:10.1182/blood-2010-06-293902
- [123] Weinreb, N.J. and Minsky, N. (1971) Serious Reaction After Konyne. The New England Journal of Medicine, 285, 1151-1152. doi:10.1056/NEJM197111112852027
- [124] Weinreb, N.J. (2008) Imiglucerase and its use for the treatment of Gaucher’s disease. Expert Opinion on Pharmacotherapy, 9, 1987-2000. doi:10.1517/14656566.9.11.1987
- [125] Andersson, H.C., Kaplan, P., Kacena, K. and Yee, J. (2008) Eight-year clinical outcomes of long-term enzyme replacement therapy for 884 children with Gaucher disease type 1. Pediatrics, 122, 1182-1190. doi:10.1542/peds.2007-2144
- [126] Weinreb, N.J., Goldblatt, J., Villalobos, J., Charrow, J., Cole, J.A., Kerstenetzky, M., vom Dahl, S. and Hollak, C.E.M. (2012) Long term clinical outcomes in Type 1 Gaucher disease following 10 years of imiglucerase treatment. Journal of Inherited Metabolic Disease. doi:10.1007/s10545-012-9528-4
- [127] Webb, B.D., Weinreb, N.J., Botti, A.C., Kirmse, B.M. and Balwani, M. (2011) JAK2V617F mutation and myeloproliferative malignancy in a patient with Type 1 Gaucher disease. Blood Cells, Molecules and Diseases, 46, 103-104. doi:10.1016/j.bcmd.2010.09.007
- [128] Srinoun, K., Svasti, S., Chumworathayee, W., Vadolas, J., Vattanaviboon, P., Fucharoen, S. and Winichagoon, P. (2009) Imbalanced globin chain synthesis determines erythroid cell pathology in thalassemic mice. Haematologica, 94, 1211-1219. doi:10.3324/haematol.2009.005827
- [129] Piga, A., Serra, M., Longo, F., Forni, G., Quarta, G., Cappellini, M.D. and Galanello, R. (2011) Changing patterns of splenectomy in transfusion-dependent thalassemia patients. American Journal of Hematology, 86, 808- 810. doi:10.1002/ajh.22102
- [130] Moshtaghi-Kashanian, G.R., Gholamhoseinian, A., Hoseinimoghadam, A. and Rajabalian, S. (2006) Splenectomy changes the pattern of cytokine production in beta-thalassemic patients. Cytokine, 35, 253-257. doi:10.1016/j.cyto.2006.09.003
- [131] Rodeghiero, F. and Ruggeri, M. (2012) Shortand longterm risks of splenectomy for benign haematological disorders: Should we revisit the indications? British Journal of Haematology, 158, 16-29. doi:10.1111/j.1365-2141.2012.09146.x
- [132] Sheikha, A.K., Salih, Z.T., Kasnazan, K.H., Khoshnaw, M.K., Al-Maliki, T., Al-Azraqi, T.A. and Zafer, M.H. (2007) Prevention of overwhelming postsplenectomy infection in thalassemia patients by partial rather than total splenectomy. Canadian Journal of Surgery, 50, 382-386.
- [133] Rasekhi, A.R., Naderifar, M., Bagheri, M.H., Shahriari, M., Foroutan, H., Karimi, M. and Nabavizadeh, S.A. (2009) Radiofrequency ablation of the spleen in patients with thalassemia intermedia: a pilot study. AJR American Journal of Roentgenology Diagnostic Imaging and Related Sciences, 192, 1425-1429. doi:10.2214/AJR.08.1382
- [134] Perotta, S., Gallagher, P.G. and Mohandas, N. (2008) Hereditary spherocytosis. Lancet, 372, 1411-1426. doi:10.1016/S0140-6736(08)61588-3
- [135] Schrier, S.L. (2012) What does the spleen see? Blood, 120, 242-243. doi:10.1182/blood-2012-05-425991
- [136] Safeukui, I., Buffet, P.A., Deplaine, G., Perrot, S., Brousse, V., Ndour, A., Nguyen, M., Mercereau-Puijalon, O., David, P.H., Milon, G. and Mohandas, N. (2012) Quantitative assessment of sensing and sequestration of spherocytic erythrocytes by the human spleen. Blood, 120, 424-430. doi:10.1182/blood-2012-01-404103
- [137] Schilling, R.F. (2009) Risks and benefits of splenectomy versus no splenectomy for hereditary spherocytosis—A personal view. British Journal of Haematology, 145, 728- 732. doi:10.1111/j.1365-2141.2009.07694.x
- [138] Casale, M. and Perrotta, S. (2011) Splenectomy for hereditary spherocytosis: complete, partial, or not at all? Expert Review of Hematology, 4, 627-635. doi:10.1586/ehm.11.51
- [139] Crary, S.E., Ramaciotti, C. and Buchanan, G.R. (2011) Prevalence of pulmonary hypertension in hereditary spherocytosis. American Journal of Hematology, 86, E73- E76. doi:10.1002/ajh.22182
- [140] Buesing, K.L., Tracy, E.T., Kiernan, C., Pastor. A.C., Cassidy, L.D., Scott, J.P., Ware, R.E., Davidoff, A.M., Rescorla, F.J., Langer, J.C., Rice, H.E. and Oldham, K.T. (2011) Partial splenectomy for hereditary spherocytosis: A multi-institutional review. Journal of Pediatric Surgery, 46, 178-183. doi:10.1016/j.jpedsurg.2010.09.090
- [141] Mistry, P.K., Sirrs, S., Chan, A., Pritzker, M.R., Duffy, T.P., Grace, M.E., Meeker, D.P. and Goldman, M.E. (2002) Pulmonary hypertension in type 1 Gaucher’s disease: Genetic and epigenetic determinants of phenotype and response to therapy. Molecular Genetics and Metabolism, 77, 91-98. doi:10.1016/S1096-7192(02)00122-1
- [142] Mistry, P.K., Deegan, P., Vellodi, A., Cole, J.A., Yeh, M., Weinreb, N.J. (2009) Timing of initiation of enzyme replacement therapy after diagnosis of type 1 Gaucher disease: effect on incidence of avascular necrosis. British Journal of Haematology, 147, 561-570. doi:10.1111/j.1365-2141.2009.07872.x
- [143] Cox, T.M., Aerts. J.M., Belmatoug, N., Cappellini, M.D., vom Dahl, S., Goldblatt, J., Grabowski, G.A., Hollak, C.E., Hwu, P., Maas, M., Martins, A.M., Mistry, P.K., Pastores, G.M., Tylki-Szymanska, A., Yee, J. and Weinreb, N. (2008) Management of non-neuronopathic Gaucher disease with special reference to pregnancy, splenectomy, bisphosphonate therapy, use of biomarkers and bone disease monitoring. Journal of Inherited Metabolic Disease, 31, 319-337. doi:10.1007/s10545-008-0779-z
- [144] Okano, K., Kakinoki, K., Suto, H., Oshima, M., Akamoto, S., Hagiike, M., Usuki, H. and Suzuki, Y. (2011) Handassisted laparoscopic partial splenectomy using an endopath monopolar sealer. Surgical Laparoscopy Endoscopy & Percutaneous Techniques, 21, e291-e294. doi:10.1097/SLE.0b013e3182311ee4
- [145] Zimran, A., Elstein, D., Schiffmann, R., Abrahamov, A., Goldberg, M., Bar-Maor, J.A., Brady, R.O., Guzzetta, P.C. and Barton, N.W. (1995) Outcome of partial splenectomy for type I Gaucher disease. The Journal of Pediatrics, 126, 596-597. doi:10.1016/S0022-3476(95)70358-6

