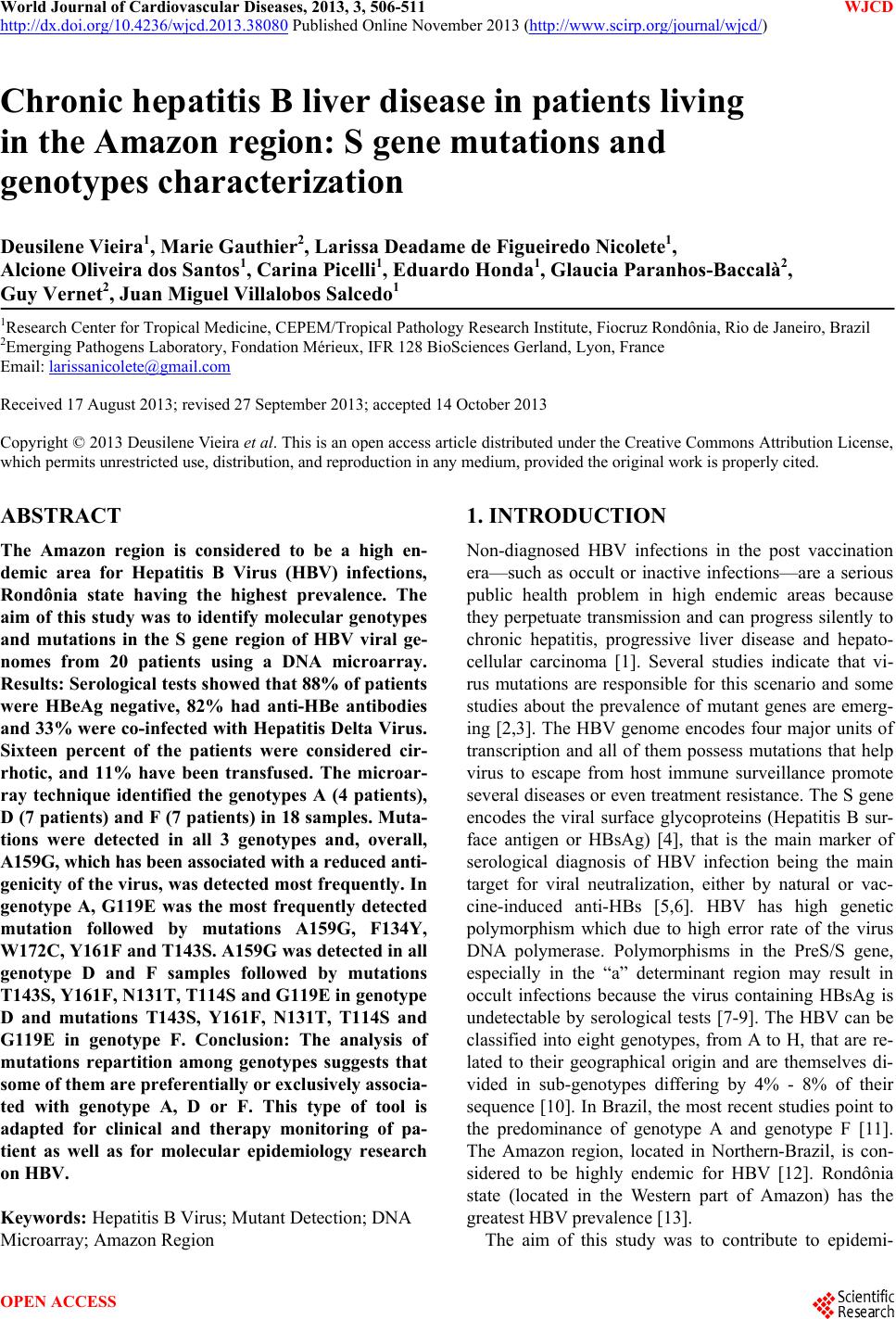
 World Journal of Cardiovascular Diseases, 2013, 3, 506-511 WJCD http://dx.doi.org/10.4236/wjcd.2013.38080 Published Online November 2013 (http://www.scirp.org/journal/wjcd/) Chronic hepatitis B liver disease in patients living in the Amazon region: S gene mutations and genotypes characterization Deusilene Vieira1, Marie Gauthier2, Larissa Deadame de Figueiredo Nicolete1, Alcione Oliveira dos Santos1, Carina Picelli1, Eduardo Honda1, Glaucia Paranhos- B a cc a l à 2, Guy Vernet2, Juan Miguel Villalobos Salcedo1 1Research Center for Tropical Medicine, CEPEM/Tropical Pathology Research Institute, Fiocruz Rondônia, Rio de Janeiro, Brazil 2Emerging Pathogens Laboratory, Fondation Mérieux, IFR 128 BioSciences Gerland, Lyon, France Email: larissanicolete@gmail.com Received 17 August 2013; revised 27 September 2013; accepted 14 October 2013 Copyright © 2013 Deusilene Vieira et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT The Amazon region is considered to be a high en- demic area for Hepatitis B Virus (HBV) infections, Rondônia state having the highest prevalence. The aim of this study was to identify molecular genotypes and mutations in the S gene region of HBV viral ge- nomes from 20 patients using a DNA microarray. Results: Serological tests showed that 88% of patients were HBeAg negative, 82% had anti-HBe antibodies and 33% were co-infected with Hepatitis Delta Virus. Sixteen percent of the patients were considered cir- rhotic, and 11% have been transfused. The microar- ray technique identified the genotypes A (4 patients), D (7 patients) and F (7 patients) in 18 samples. Muta- tions were detected in all 3 genotypes and, overall, A159G, which has been associated with a reduced anti- genicity of the virus, was detected most frequently. In genotype A, G119E was the most frequently detected mutation followed by mutations A159G, F134Y, W172C, Y161F and T143S. A159G was detected in all genotype D and F samples followed by mutations T143S, Y161F, N131T, T114S a nd G119E in genoty pe D and mutations T143S, Y161F, N131T, T114S and G119E in genotype F. Conclusion: The analysis of mutations repartition among genotypes suggests that some of them are preferentially or exclusively associa- ted with genotype A, D or F. This type of tool is adapted for clinical and therapy monitoring of pa- tient as well as for molecular epidemiology research on HBV. Keywords: Hepatitis B Virus; Mutant Detection; DNA Microarray; Amazon Region 1. INTRODUCTION Non-diagnosed HBV infections in the post vaccination era—such as occult or inactive infections—are a serious public health problem in high endemic areas because they perpetuate transmission and can progress silently to chronic hepatitis, progressive liver disease and hepato- cellular carcinoma [1]. Several studies indicate that vi- rus mutations are responsible for this scenario and some studies about the prevalence of mutant genes are emerg- ing [2,3]. The HBV genome encodes four major units of transcription and all of them possess mutations that help virus to escape from host immune surveillance promote several diseases or even treatment resistance. The S gene encodes the viral surface glycoproteins (Hepatitis B sur- face antigen or HBsAg) [4], that is the main marker of serological diagnosis of HBV infection being the main target for viral neutralization, either by natural or vac- cine-induced anti-HBs [5,6]. HBV has high genetic polymorphism which due to high error rate of the virus DNA polymerase. Polymorphisms in the PreS/S gene, especially in the “a” determinant region may result in occult infections because the virus containing HBsAg is undetectable by serological tests [7-9]. The HBV can be classified into eight genotypes, from A to H, that are re- lated to their geographical origin and are themselves di- vided in sub-genotypes differing by 4% - 8% of their sequence [10]. In Brazil, the most recent studies point to the predominance of genotype A and genotype F [11]. The Amazon region, located in Northern-Brazil, is con- sidered to be highly endemic for HBV [12]. Rondônia state (located in the Western part of Amazon) has the greatest HBV prevalence [13]. The aim of this study was to contribute to epidemi- OPEN ACCESS 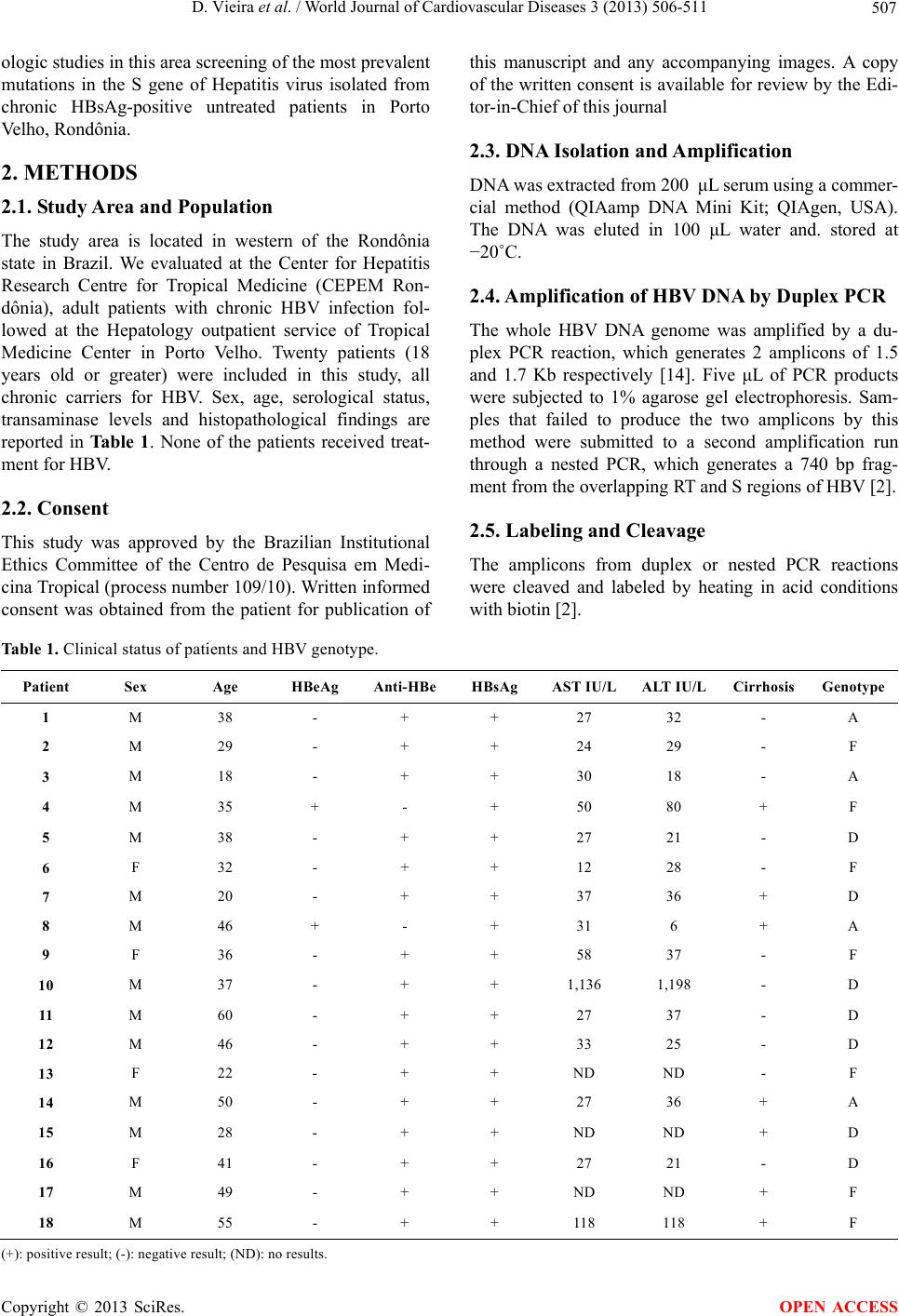 D. Vieira et al. / World Journal of Cardiovascular Diseases 3 (2013) 506-511 507 ologic studies in this area screening of the most prevalent mutations in the S gene of Hepatitis virus isolated from chronic HBsAg-positive untreated patients in Porto Velho, Rondônia. 2. METHODS 2.1. Study Area and Population The study area is located in western of the Rondônia state in Brazil. We evaluated at the Center for Hepatitis Research Centre for Tropical Medicine (CEPEM Ron- dônia), adult patients with chronic HBV infection fol- lowed at the Hepatology outpatient service of Tropical Medicine Center in Porto Velho. Twenty patients (18 years old or greater) were included in this study, all chronic carriers for HBV. Sex, age, serological status, transaminase levels and histopathological findings are reported in Ta b l e 1 . None of the patients received treat- ment for HBV. 2.2. Consent This study was approved by the Brazilian Institutional Ethics Committee of the Centro de Pesquisa em Medi- cina Tropical (process number 109/10). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the Edi- tor-in-Chief of this journal 2.3. DNA Isolation and Amplification DNA was extracted from 200 μL serum using a commer- cial method (QIAamp DNA Mini Kit; QIAgen, USA). The DNA was eluted in 100 μL water and. stored at −20˚C. 2.4. Amplification of HBV DNA by Duplex PCR The whole HBV DNA genome was amplified by a du- plex PCR reaction, which generates 2 amplicons of 1.5 and 1.7 Kb respectively [14]. Five μL of PCR products were subjected to 1% agarose gel electrophoresis. Sam- ples that failed to produce the two amplicons by this method were submitted to a second amplification run through a nested PCR, which generates a 740 bp frag- ment from the overlapping RT and S regions of HBV [2]. 2.5. Labeling and Cleavage The amplicons from duplex or nested PCR reactions were cleaved and labeled by heating in acid conditions with biotin [2]. Table 1. Clinical status of patients and HBV genotype. Patient Sex Age HBeAg Anti-HBeHBsAg AST IU/LALT IU/L Cirrhosis Genotype 1 M 38 - + + 27 32 - A 2 M 29 - + + 24 29 - F 3 M 18 - + + 30 18 - A 4 M 35 + - + 50 80 + F 5 M 38 - + + 27 21 - D 6 F 32 - + + 12 28 - F 7 M 20 - + + 37 36 + D 8 M 46 + - + 31 6 + A 9 F 36 - + + 58 37 - F 10 M 37 - + + 1,136 1,198 - D 11 M 60 - + + 27 37 - D 12 M 46 - + + 33 25 - D 13 F 22 - + + ND ND - F 14 M 50 - + + 27 36 + A 15 M 28 - + + ND ND + D 16 F 41 - + + 27 21 - D 17 M 49 - + + ND ND + F 18 M 55 - + + 118 118 + F ( +): positive result; (-): negative result; (ND): no results. Copyright © 2013 SciRes. OPEN ACCESS  D. Vieira et al. / World Journal of Cardiovascular Diseases 3 (2013) 506-511 508 2.6. DNA Microarray Hybridization PCR products were hybridized on a high-density DNA microarray (designed by Fondation Mérieux and manu- factured by Affymetrix, California, USA) which is made of more than 500,000 features (11 µM side length) each containing a specific DNA probe [2]. 2.7. DNA Microarray Analysis The array was analyzed using the DNAEM software (bioMérieux, France). The analysis allows the simulta- neous identification of the HBV genotype (A to H) and the detection of 994 different mutations in S, RT, preC and BCP, Core, X genes as described by Gauthier et al. (2010) [2]. 2.8. Sequencing of PCR Products Samples were sequenced in order to compare with the results obtained with the microarray and confirmation of genotypes, mutations and phylogenetic analysis. Se- quencing was performed by GATC Biotech AG (Kon- stanz, Germany). 2.9. Serology for HBV Serum HBV markers (HBeAg, Anti-HBe, HBsAg, Anti- HBs, Anti-HBc) were analyzed using commercial kits (DiaSorin S.p.A, Italy) according to manufacturer speci- fications. Biochemical tests including levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) were determined using Roche’s Cobas Mira Plus analyzer. HDV-RNA test in house was used in co-in- fected patients to defining specific treatment. 2.10. Statistical Analysis The student t test was used to determine the statistical significance of the difference in the number of mutations and the Fischer exact test to compare the presence of individual mutations in patients with and without cirrho- sis. 3. RESULTS 3.1. Characterization of the Patients The majority (88.8%) of the 20 patients was male and the average age was 37 years. All of them were HBsAg for more than 6 months. The results of serological tests showed that 88% were HBeAg negative and also had anti-HBe antibodies. Patients 5, 10 and 15 are co-in- fected by Hepatitis Delta Virus (HDV). According to the histopathological findings, 16% of the patients were con- sidered cirrhotic (Table 1). Samples from 18 patients could be analyzed with the DNA microarray (90%): 8 after whole genome duplex-PCR and 10 after nested- PCR. DNA could not be amplified in two samples using both protocols and could not be tested on the microarray. 3.2. S Gene Mutation Results The genotypes obtained by microarray presented 100% of similarity with all samples sequenced. Genotypes A, D and F were respectively found by the microarray tech- nique in 4 (22.2%), 7 (38.8%) and 7 (38.8%) of the 18 tested samples. There is no indication that one of the three detected genotypes is associated with cirrhosis (da- ta not shown). In this study it was possible to identify genotypes A, D and F of HBV, prevalent in the state of Rondônia. Twenty-three different mutations in the S re- gion of HBV could be detected in the studied patients (Ta ble 2 ). Mutations were detected in all 18 samples at 23 different codons (Table 2). Overall genotype F virus- es were found more frequently mutated (mean number of mutations/patient: 9.9) than non-F genotypes (mean num- ber 4.9). Genotype A viruses has 4.3 mutations on avera- ge and D viruses have 5.3 mutations. The patients with cirrhosis (n = 7) have 7.3 polymor- phisms on average whereas this number is 6.6 in the pa- tients without cirrhosis (n = 11). Patients with elevated transaminases (n = 4) have a slightly higher number of mutations than those with normal levels (8.8 vs 6.3). The 3 patients with HDV-co-infection have a slightly lower number of mutations than those with HBV infection only (5.3 versus 7.1). As shown in Table 2, the most frequent mutation was A159G which was detected in 16 out of 18 patients (88.8%). The two patients with a wild-type amino-acid at that position had a genotype A virus. The G119E and N131T mutations were also detected in the majority of patients (11/18, 61.1%) although the former mutation was more frequent in genotype A (100%) than in geno- types D and F (42.8% and 57.1% respectively). Con- versely, the N131T mutation was less frequent in geno- type A (25%) than in genotype D (57.1%) and, more evidently, in genotype F (85.7%). G119E was the most frequently detected mutation in genotype A, A159G in genotype D and A159G and P178Q in genotype F. Our results are consistent with these studies as all 4 genotype A specimens contain this mutation. In our study, G119E is more often detected in cirrhotic (71.4%) versus non-cirrhotic (55.4%) patients. 4. DISCUSSION 4.1. Genotyping Results These genotypes have been previously characterized as circulating in Brazil [15-18]. However, a high prevalence of genotype F proves to be the predominant characteris- tic of Amerindian populations in the northern region [17]. n our study, genotypes F and D were more prevalent I Copyright © 2013 SciRes. OPEN ACCESS  D. Vieira et al. / World Journal of Cardiovascular Diseases 3 (2013) 506-511 509 Table 2. Detection of genotypes and S gene mutations by microarray technique (Gauthier et al. 2010). Patient Genotype Mutations in HBsAg 1 A G119E 2 F I110L, G119E, P120T, N131T, F158L, A159G, W172C, P178Q, F183C,S204N 3 A G119E, N131T, F134Y, T143S, A159G, Y161F 4 F I110L, G119E, N131T, T143A, F158L, A159G, K160N, W172C, P178Q, F183C, M198I, S204N 5 D T143S, A159G 6 F I110L, G119E, F134L, T143A, F158L, A159G, K160N, P178Q, F183C, S204N 7 D T143S, A159G 8 A G119E, F134L, A166G, W172C 9 F I110L, N131T, T140S, T143S, F158L, A159G, F183C, P178Q, M198I, S204N 10 D N131T, F134Y, C139S, T143S, A159G, Y161F 11 D T114S, N131T, F134Y, T143S, A159G, Y161F, W172C 12 D T114S, G119E, A159G, Y161F, I195M 13 F C137W, N131T, F134L, G145R, F158L, A159G, K160N, P178Q 14 A G119E, F134Y, T143S, A159G, Y161F, W172C 15 D I110L,T114S, G119E, N131T, T143S, A159G, Y161F, P178Q 16 D G119E, P120T, N131T, T143S, A159G, Y161F, P178Q, 17 F Y100C, I110L, G119E, T143A, N131T, F158L, A159G, K160N, W172C, P178Q, F183C, S204N 18 F P127L, N131T,A159G, K160N, P178Q, F183C, S204N The most frequent mutations are in bold. than genotype A, although in previous studies in this re- gion genotypes A and D were found to have the highest prevalence [16]. Interestingly, the 7 HBV of genotype F are those which contain the highest average number of mutations in HBsAg, confirming the greater genetic variability of this genotype as suggested by the co-cir- culation of the three sub-genotypes F1, F2 and F4 in Brazil [11]. Based on these results, it is necessary further study molecular phylogeny of HBV on a greater number of patients from state of Rondônia. 4.2. Mutations Detection in the S Region and Correlation with the Genotype and Clinical Status In our sample panel we did not find any correlation be- tween genotype and severity (elevated transaminases and/or cirrhosis) as suggested by different authors [19,20]. Some studies demonstrate the importance of investigating amino acid substitutions in HBsAg since HBV replication occurs mainly in regions where there are amino acid substitutions [21]. There were different muta- tions in the S region of HBV genomes from the patients of our study. The percentage of patients harboring these mutations varied between 5.5% and 88.8%. However, we do not know if there is an impact of this high number of mutations on the clinical outcome of the patients. Pa- tients with elevated transaminases or with cirrhosis do not have more mutations than others and patients with genotype F viruses, which show more mutations than vi- ruses of other genotypes, do not show more frequent ele- vated transaminases or cirrhosis. The most prevalent mutation in our study was A159G which has been detected in all genotypes D and F sam- ples, irrespective of the clinical status of the patients. The mutation has been detected in 2 out of 4 genotype A sam- ples. A159G has been shown to be more common in symptomatic patients [22]. In our study it is present in both cirrhotic and non-cirrhotic patients. The G119E mutation, which is also frequently en- countered in our study, affects the secretion of virion and also the recognition of HBsAg by monoclonal antibody used in commercial assays [23,24]. Some studies consi- der this mutation as linked to genotype A. The N131T mutation was detected in all genotypes but was more prevalent in genotype F. This conservative mu- tation is frequently found in gibbon and other primate- derived HBV sequences [24]. Several mutations have been found in the majority of genotype F specimen but were never detected in other genotypes (F158L, K160N, F183C, S204N). The G145R mutation in the major hy- Copyright © 2013 SciRes. OPEN ACCESS  D. Vieira et al. / World Journal of Cardiovascular Diseases 3 (2013) 506-511 510 drophilic region has been detected in only one sample (genotype F). Several studies have demonstrated the high prevalence of this mutation in Italy, the United Kingdom, the United States, Singapore, Taiwan, Senegal, India, In- donesia and Japan [8,25,26]. Studies conducted in Brazil with samples from southwestern Paraná did not find this mutation [25] which is coherent with our own results. The I110L, T143S and F134Y polymorphisms which were detected in our study have been already described (Simmonds & Midgley 2005). We detected mutations, G119E, G145R, A159G and F183C, which were pre- viously characterized as reducing immune response to HBsAg [9,21,27]. However, all samples from our study, including several samples which harbor 2 of the above mutations, were properly diagnosed for HBsAg as shown in Table 1, probably due to the use of kits containing polyclonal antibodies. Our study on HBsAg-positive pa- tients demonstrates that polymorphisms in S gene occur not only in occult HBV infections and patients with more severe disease. Furthermore, this is the first study to de- scribe S gene mutations in the Amazon region and that possible will helps in molecular epidemiology of HBV. 5. ACKNOWLEDGEMENTS We would like to thank Kelly Régia Vieira de Oliveira (CEPEM/ IPEPATRO) for sorologic results. REFERENCES [1] Lavanchy, D. (2004) Hepatitis B virus epidemiology, di- sease burden, treatment, and current and emerging pre- vention and control measures. Journal of Viral Hepatitis, 11, 97-107. http://dx.doi.org/10.1046/j.1365-2893.2003.00487.x [2] Gauthier, M., Bonnaud, B., Arsac, M., Lavocat, F., Mai- setti, J., Kay, A., et al. (2010) Microarray for hepatitis B virus genotyping and detection of 994 mutations along the genome. Journal of Clinical Microbiology, 48, 4207- 4215. http://dx.doi.org/10.1128/JCM.00344-10 [3] Sticchi, L., Caligiuri, P., Cacciani, R., Alicino, C. and Bruzzone, B. (2013) Epidemiology of HBV S-gene mu- tants in the Liguria Region, Italy: Implications for sur- veillance and detection of new escape variants. Human Vaccines & Immunotherapeutics, 9, 568-571. http://dx.doi.org/10.4161/hv.23236 [4] Kao, J.-H., Liu, C.-J. and Chen, D.-S. (2002) Hepatitis B viral genotypes and lamivudine resistance. Journal of He- patology, 36, 303-304. http://dx.doi.org/10.1016/S0168-8278(01)00246-X [5] Lai, C.L., Ratziu, V., Yuen, M.-F. and Poynard, T. (2003) Viral hepatitis B. The Lancet, 362, 2089-2094. http://dx.doi.org/10.1016/S0140-6736(03)15108-2 [6] Schaefer, S. (2007) Hepatitis B virus taxonomy and hepa- titis B virus genotypes. World Journal of Gastroenterolo- gy , 13, 14-21. [7] Datta, S., Banerjee, A., Chandra, P.K., Chowdhury, A. and Chakravarty, R. (2006) Genotype, phylogenetic ana- lysis, and transmission pattern of occult hepatitis B virus (HBV) infection in families of asymptomatic HBsAg car- riers. Journal of Medical Virology, 78, 53-59. http://dx.doi.org/10.1002/jmv.20503 [8] Weber, B. (2005) Genetic variability of the S gene of he- patitis B virus: clinical and diagnostic impact. Journal of Clinical Virology : The Official Publication of the Pan American Society for Clinical Virology, 32, 102-112. http://dx.doi.org/10.1016/j.jcv.2004.10.008 [9] François, G., Kew, M., Damme, Van P., Mphahlele, M.J. and Meheus, A. (2001) Mutant hepatitis B viruses: A matter of academic interest only or a problem with far- reaching implications? Vaccine, 19, 3799-3815. http://dx.doi.org/10.1016/S0264-410X(01)00108-6 [10] Norder, H., Couroucé, A.-M., Coursaget, P., Echevarria, J.M., Lee, S.-D., Mushahwar, I.K., et al. (2004) Genetic diversity of hepatitis B virus strains derived worldwide: Genotypes, subgenotypes, and HBsAg subtypes. Intervir- ology, 47, 289-309. http://dx.doi.org/10.1159/000080872 [11] Mello, F.C.A., Souto, F.J.D., Nabuco, L.C., Villela-No- gueira, C.A., Coelho, H.S.M., Franz, H.C.F., et al. (2007) Hepatitis B virus genotypes circulating in Brazil: Mole- cular characterization of genotype F isolates. BMC Mi- crobiology, 7, 103. http://dx.doi.org/10.1186/1471-2180-7-103 [12] Ferreira, C.T. and Silveira, T.R. (2004) Hepatites virais: Aspectos da epidemiologia e da prevenção. Revista Bra- sileira de Epidemiologia, 7, 473-487. http://dx.doi.org/10.1590/S1415-790X2004000400010 [13] Katsuragawa, T.H., Cunha, R.P.A., Salcedo, J.M.V., Souza, D.C.A., Oliveira, K.R.V., Gil, L.H.S., et al. (2010) Alta soroprevalência de infecção pelos vírus das hepatites B e C na região do alto rio Madeira, Porto Velho, Rondô- nia, Brasil. Revista Pan-Amazônica de Saúde, 1, 91-106. http://dx.doi.org/10.5123/S2176-62232010000200011 [14] Tran, N., Berne, R., Chann, R., Gauthier, M., Martin, D., Armand, M.-A., et al. (2006) European multicenter eva- luation of high-density DNA probe arrays for detection of hepatitis B virus resistance mutations and identification of genotypes. Journal of Clinical Microbiology, 44, 2792-2800. http://dx.doi.org/10.1128/JCM.00295-06 [15] Ferreira, R.C., Teles, S.A., Dias, M.A., Tavares, V.R., Silva, S.A., Gomes, S.A., et al. (2006) Hepatitis B virus infection profile in hemodialysis patients in Central Bra- zil: prevalence, risk factors, and genotypes. Memórias Do Instituto Oswaldo Cruz, 101, 689-692. http://dx.doi.org/10.1590/S0074-02762006000600019 [16] Oliveira, L.C.M. and Pontes, J.P.J. (2010) Frequency of hepatitis B immunity and occupational exposures to body fluids among Brazilian medical students at a public uni- versity. Revista Do Instituto de Medicina Tropical de São Paulo no date, 52, 247-252. [17] Moraes, M.T., Niel, C. and Gomes, S.A. (1999) A poly- merase chain reaction-based assay to identify genotype F of hepatitis B virus. Brazilian Journal of Medical and Bi- ological Research, 32, 45-49. [18] Araujo, N.M., Mello, F.C.A., Yoshida, C.F.T., Niel, C. Copyright © 2013 SciRes. OPEN ACCESS  D. Vieira et al. / World Journal of Cardiovascular Diseases 3 (2013) 506-511 Copyright © 2013 SciRes. 511 OPEN ACCESS and Gomes, S.A. (2004) High proportion of subgroup A’ (genotype A) among Brazilian isolates of Hepatitis B vi- rus. Archives of Virology, 149, 1383-1395. http://dx.doi.org/10.1007/s00705-003-0269-4 [19] Kay, A. and Zoulim, F. (2007) Hepatitis B virus genetic variability and evolution. Virus Research, 127, 164-176. http://dx.doi.org/10.1016/j.virusres.2007.02.021 [20] Schaefer, S. (2005) Hepatitis B virus: Significance of ge- notypes. Journal of Viral Hepatitis, 12, 111-124. http://dx.doi.org/10.1111/j.1365-2893.2005.00584.x [21] Wu, C., Zhang, X., Tian, Y., Song, J., Yang, D., Roggen- dorf, M., et al. (2010) Biological significance of amino acid substitutions in hepatitis B surface antigen (HBsAg) for glycosylation, secretion, antigenicity and immunoge- nicity of HBsAg and hepatitis B virus replication. The Journal of General Virology, 91, 483-492. http://dx.doi.org/10.1099/vir.0.012740-0 [22] Ruiz-Tachiquín, M.-E., Valdez-Salazar, H.-A., Juárez- Barreto, V., Dehesa-Violante, M., Torres, J., Muñoz-Her- nández, O., et al. (2007) Molecular analysis of hepatitis B virus “a” determinant in asymptomatic and symptomatic Mexican carriers. Virology Journal, 4, 6. http://dx.doi.org/10.1186/1743-422X-4-6 [23] Khan, N., Guarnieri, M., Ahn, S.H., Li, J., Zhou, Y., Bang, G., et al. (2004) Modulation of hepatitis B virus secretion by naturally occurring mutations in the S gene. Journal of Virology, 78, 3262-3270. http://dx.doi.org/10.1128/JVI.78.7.3262-3270.2004 [24] Tong, S., Kim, K.-H., Chante, C., Wands, J. and Li, J. (2005) Hepatitis B Virus e Antigen Variants. Internation- al Journal of Medical Sciences, 2, 2-7. http://dx.doi.org/10.7150/ijms.2.2 [25] Araujo, N.M., Vianna, C.O.A., Soares, C.C. and Gomes, S.A. (2008) A unique amino acid substitution, L215Q, in the hepatitis B virus small envelope protein of a genotype F isolate that inhibits secretion of hepatitis B virus subvi- ral particles. Intervirology, 51, 81-86. http://dx.doi.org/10.1159/000127430 [26] Oon, C.J., Lim, G.K., Ye, Z., Goh, K.T., Tan, K.L., Yo, S.L., et al. (1995) Molecular epidemiology of hepatitis B virus vaccine variants in Singapore. Vaccine, 13, 699-702. http://dx.doi.org/10.1016/0264-410X(94)00080-7 [27] Ito, K., Qin, Y., Guarnieri, M., Garcia, T., Kwei, K., Mi- zokami, M., et al. (2005) Impairment of Hepatitis B Virus Virion Secretion by Single-Amino-Acid Substitutions in the Small Envelope Protein and Rescue by a Novel Gly- cosylation Site. Journal of Virology, 79, 14404-14410.
|