D. Light et al. / Case Reports in Clinical Medicine 2 (2013) 4 57-459
458
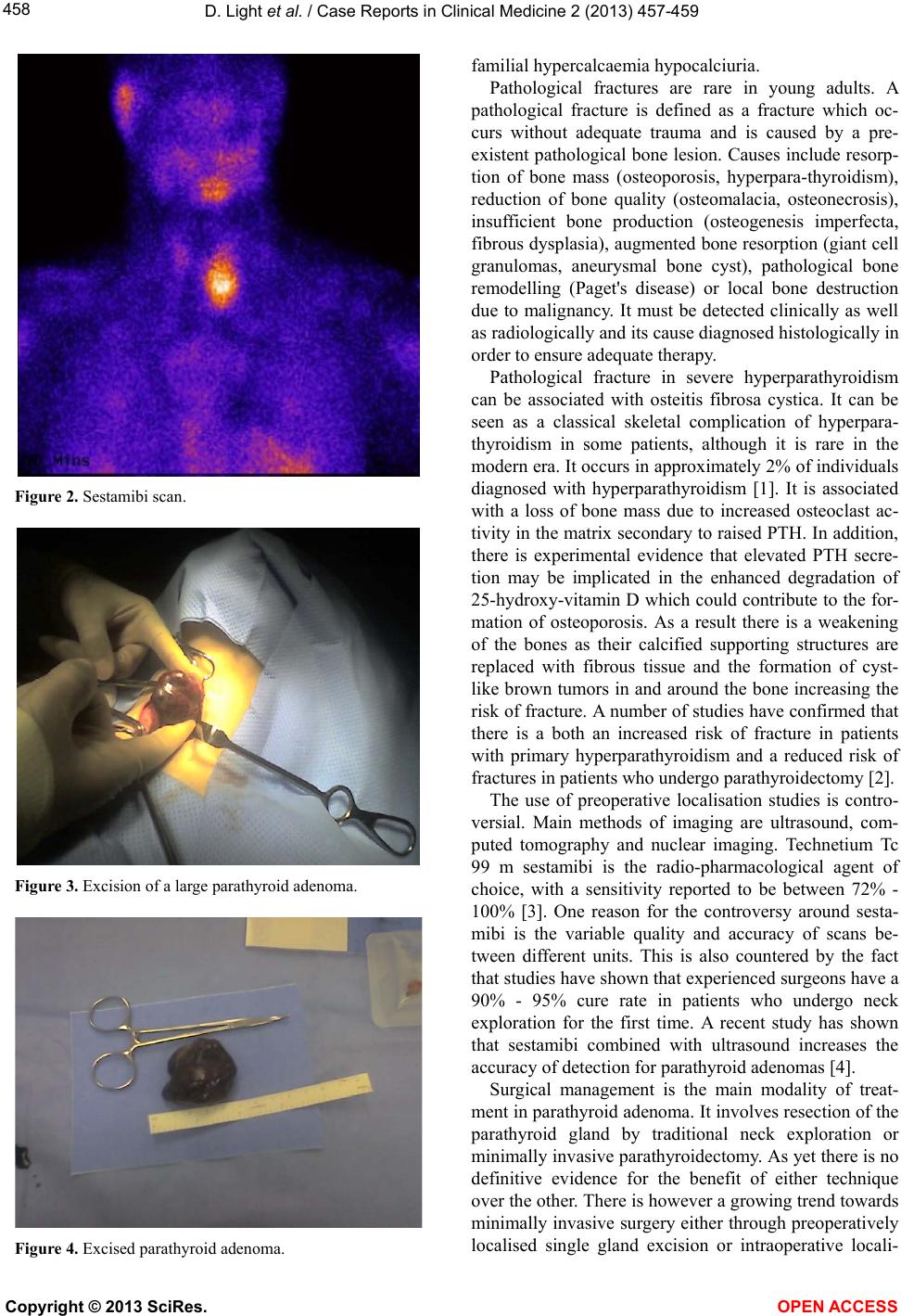
Figure 2. Sestamibi scan.
Figure 3. Excision of a large parathyroid adenoma.
Figure 4. Excised parathyroid adenoma.
familial hypercalcaemia hypocalciuria.
Pathological fractures are rare in young adults. A
pathological fracture is defined as a fracture which oc-
curs without adequate trauma and is caused by a pre-
existent pathological bone lesion. Causes include resorp-
tion of bone mass (osteoporosis, hyperpara-thyroidism),
reduction of bone quality (osteomalacia, osteonecrosis),
insufficient bone production (osteogenesis imperfecta,
fibrous dysplasia), au gmented bone resorption (giant cell
granulomas, aneurysmal bone cyst), pathological bone
remodelling (Paget's disease) or local bone destruction
due to malignancy. It must be detected clinically as well
as radiologically and its cause diagnosed histologically in
order to ensure adequate therapy.
Pathological fracture in severe hyperparathyroidism
can be associated with osteitis fibrosa cystica. It can be
seen as a classical skeletal complication of hyperpara-
thyroidism in some patients, although it is rare in the
modern era. It occurs in approximately 2% of individuals
diagnosed with hyperparathyroidism [1]. It is associated
with a loss of bone mass due to increased osteoclast ac-
tivity in the matrix secondary to raised PTH. In additio n,
there is experimental evidence that elevated PTH secre-
tion may be implicated in the enhanced degradation of
25-hydroxy-vitamin D which could contribute to the for-
mation of osteoporosis. As a result there is a weakening
of the bones as their calcified supporting structures are
replaced with fibrous tissue and the formation of cyst-
like brown tumors in and around the bone increasing the
risk of fracture. A number of studies have confirmed that
there is a both an increased risk of fracture in patients
with primary hyperparathyroidism and a reduced risk of
fractures i n p atients who u nderg o pa ra thyroidecto my [2].
The use of preoperative localisation studies is contro-
versial. Main methods of imaging are ultrasound, com-
puted tomography and nuclear imaging. Technetium Tc
99 m sestamibi is the radio-pharmacological agent of
choice, with a sensitivity reported to be between 72% -
100% [3]. One reason for the controversy around sesta-
mibi is the variable quality and accuracy of scans be-
tween different units. This is also countered by the fact
that studies have shown that experienced surgeons have a
90% - 95% cure rate in patients who undergo neck
exploration for the first time. A recent study has shown
that sestamibi combined with ultrasound increases the
accuracy of detection for parathyroid adenomas [4].
Surgical management is the main modality of treat-
ment in parathyroid adenoma. It involves resection of the
parathyroid gland by traditional neck exploration or
minimally invasive parathyroidectomy. As yet there is no
definitive evidence for the benefit of either technique
over the other. There is however a growing trend towards
minimally invasive surgery either through preoperatively
localised single gland excision or intraoperative locali-
Copyright © 2013 SciRes. OPEN ACCESS