Pneumothorax Complicating Port-a-Cath and Groshong Catheter Positioning in
Children: Our Experience before Routine Ultrasound-Guided Puncture
348
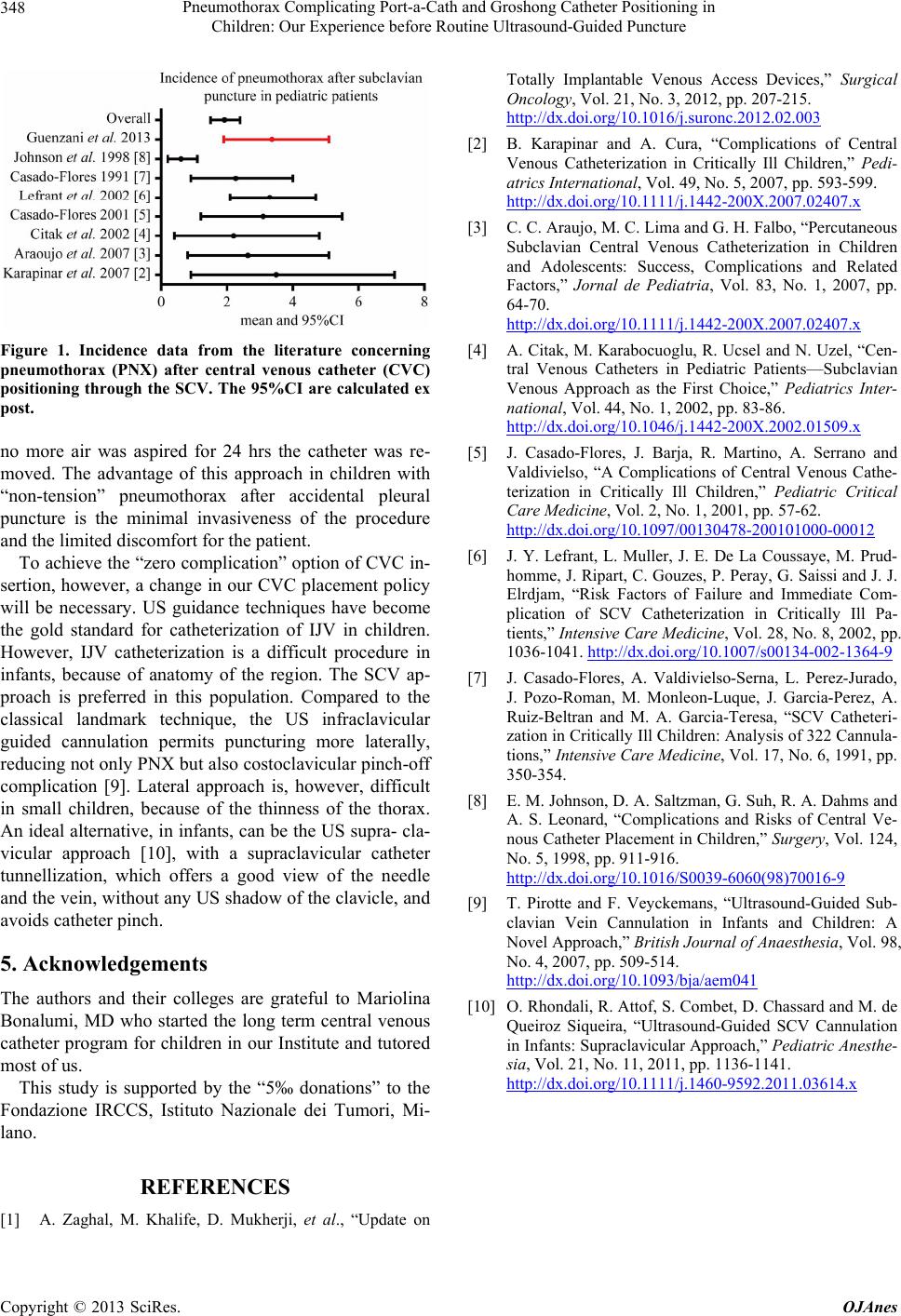
Figure 1. Incidence data from the literature concerning
pneumothorax (PNX) after central venous catheter (CVC)
positioning through the SCV. The 95%CI are calculated ex
post.
no more air was aspired for 24 hrs the catheter was re-
moved. The advantage of this approach in children with
“non-tension” pneumothorax after accidental pleural
puncture is the minimal invasiveness of the procedure
and the limited discomfort for the patient.
To achieve the “zero complication” option of CVC in-
sertion, however, a change in our CVC placement policy
will be necessary. US guidance techniques have become
the gold standard for catheterization of IJV in children.
However, IJV catheterization is a difficult procedure in
infants, because of anatomy of the region. The SCV ap-
proach is preferred in this population. Compared to the
classical landmark technique, the US infraclavicular
guided cannulation permits puncturing more laterally,
reducing not only PNX but also costoclavicular pinch-off
complication [9]. Lateral approach is, however, difficult
in small children, because of the thinness of the thorax.
An ideal alternative, in infants, can be the US supra- cla-
vicular approach [10], with a supraclavicular catheter
tunnellization, which offers a good view of the needle
and the vein, without any US shadow of the clavicle, and
avoids catheter pinch.
5. Acknowledgements
The authors and their colleges are grateful to Mariolina
Bonalumi, MD who started the long term central venous
catheter program for children in our Institute and tutored
most of us.
This study is supported by the “5‰ donations” to the
Fondazione IRCCS, Istituto Nazionale dei Tumori, Mi-
lano.
REFERENCES
[1] A. Zaghal, M. Khalife, D. Mukherji, et al., “Update on
Totally Implantable Venous Access Devices,” Surgical
Oncology, Vol. 21, No. 3, 2012, pp. 207-215.
http://dx.doi.org/10.1016/j.suronc.2012.02.003
[2] B. Karapinar and A. Cura, “Complications of Central
Venous Catheterization in Critically Ill Children,” Pedi-
atrics International, Vol. 49, No. 5, 2007, pp. 593-599.
http://dx.doi.org/10.1111/j.1442-200X.2007.02407.x
[3] C. C. Araujo, M. C. Lima and G. H. Falbo, “Percutaneous
Subclavian Central Venous Catheterization in Children
and Adolescents: Success, Complications and Related
Factors,” Jornal de Pediatria, Vol. 83, No. 1, 2007, pp.
64-70.
http://dx.doi.org/10.1111/j.1442-200X.2007.02407.x
[4] A. Citak, M. Karabocuoglu, R. Ucsel and N. Uzel, “Cen-
tral Venous Catheters in Pediatric Patients—Subclavian
Venous Approach as the First Choice,” Pediatrics Inter-
national, Vol. 44, No. 1, 2002, pp. 83-86.
http://dx.doi.org/10.1046/j.1442-200X.2002.01509.x
[5] J. Casado-Flores, J. Barja, R. Martino, A. Serrano and
Valdivielso, “A Complications of Central Venous Cathe-
terization in Critically Ill Children,” Pediatric Critical
Care Medicine, Vol. 2, No. 1, 2001, pp. 57-62.
http://dx.doi.org/10.1097/00130478-200101000-00012
[6] J. Y. Lefrant, L. Muller, J. E. De La Coussaye, M. Prud-
homme, J. Ripart, C. Gouzes, P. Peray, G. Saissi and J. J.
Elrdjam, “Risk Factors of Failure and Immediate Com-
plication of SCV Catheterization in Critically Ill Pa-
tients,” Intensive Care Medicine, Vol. 28, No. 8, 2002, pp.
1036-1041. http://dx.doi.org/10.1007/s00134-002-1364-9
[7] J. Casado-Flores, A. Valdivielso-Serna, L. Perez-Jurado,
J. Pozo-Roman, M. Monleon-Luque, J. Garcia-Perez, A.
Ruiz-Beltran and M. A. Garcia-Teresa, “SCV Catheteri-
zation in Critically Ill Children: Analysis of 322 Cannula-
tions,” Intensive Care Medicine, Vol. 17, No. 6, 1991, pp.
350-354.
[8] E. M. Johnson, D. A. Saltzman, G. Suh, R. A. Dahms and
A. S. Leonard, “Complications and Risks of Central Ve-
nous Catheter Placement in Children,” Surgery, Vol. 124,
No. 5, 1998, pp. 911-916.
http://dx.doi.org/10.1016/S0039-6060(98)70016-9
[9] T. Pirotte and F. Veyckemans, “Ultrasound-Guided Sub-
clavian Vein Cannulation in Infants and Children: A
Novel Approach,” British Journal of Anaesthesia, Vol. 98,
No. 4, 2007, pp. 509-514.
http://dx.doi.org/10.1093/bja/aem041
[10] O. Rhondali, R. Attof, S. Combet, D. Chassard and M. de
Queiroz Siqueira, “Ultrasound-Guided SCV Cannulation
in Infants: Supraclavicular Approach,” Pediatric Anesthe-
sia, Vol. 21, No. 11, 2011, pp. 1136-1141.
http://dx.doi.org/10.1111/j.1460-9592.2011.03614.x
Copyright © 2013 SciRes. OJAnes