Paper Menu >>
Journal Menu >>
 Surgical Science, 2011, 2, 22-24 doi:10.4236/ss.2011.21006 Published Online January 2011 (http://www.SciRP.org/journal/ss) Copyright © 2011 SciRes. SS HIV Seropositivity among Paediatric Surgical Patients at the Lagos University Teaching Hospital: What Risk to the Surgeon Christopher Bode, Adesoji Ademuyiwa, Sylvester Ikhisemojie, Olumide Elebute Pediatric Surgery Unit, Depa rt ment of Surgery College of Medicine University of Lagos, Lagos University Teaching Hospital Lagos, Nigeria E-mail: cobode@yahoo.com Received September 10, 2010; revised October 25, 2010; accepted November 10, 201 0 Abstract Background: Although much concern has been expressed about the occupational risk posed to surgeons by the HIV pandemic infection, the paediatric age group is often seen as less likely to harbor the disease. Aim: To determine the HIV infection rate among children presenting for surgical operations at the Lagos Uni- versity Teaching Hospital (LUTH), Lagos. Materials, patients and method: Blood was taken from 1000 consecutive children referred to LUTH for surgical conditions and tested for HIV sero-positivity using the Western blot method. Consenting parents of sero-positive patients were also tested. Result: Five children tested positive for HIV, giving an overall infection rate of 0.5%. Four mothers and three consenting fathers were also positive. In one child, none of the parents was positive and he was suspected to have developed the disease from a previous blood transfusion prior to presentation in LUTH. This possibly resulted from transfusion of infected blood during its window period. Conclusion: Although the HIV infection rate of 0.5% in paediatric surgical group in Lagos is low, surgeons should vigilantly apply universal precautions to prevent needle-stick injuries while the rate of HIV infection should be periodically monitored to deter- mine the trend. Keywords: HIV/AIDS, Risk, Paediatric Surgeon, Blood 1. Introduction The prev alence of HIV/A IDS in the paediatr ic age group has not mirrored what is seen in the adult population. Since this disease was f irst described in Nigeria in 1986, the incidence rose steadily to 5.8 percent of the general population as reported in most studies conducted by 2001 [1,2]. While this figure was a national average, there were inter-regional and intra-regional differences [3]. The prevalence appears to have stabilized at 3.1%, among women attending antenatal clinics in Nigeria [4]. The overall picture has however largely ignored the pae- diatric age group and little has been reported on the prevalence of HIV/AIDS among Nigerian children with surgical problems [5]. The risk posed by this significant disease to the paediatric surgeon in Nigeria has not been quantified hence this study [6-8]. 2. Patients and Methods One thousand consecutive patients referred to the Paedi- atric Surgery Unit of the Lagos University Teaching Hospital, Nigeria were recruited into this study. These patients presented to the Paediatric Surgery Outpatient within the study period - November 2006 to October 2008. Other patients seen within the study period were not included after a sample size of 1000. All patients who had previously been diagnosed with HIV/ AIDS and those who had symptoms associated with AIDS were also excluded from the study. The patients were aged between 2 weeks and 16 years, with a median age of 6months. They were referred to the Unit for various con- ditions as shown in Table 1 . The Male: Female ratio was 4:1. Informed consent was obtained from parents of all patients. As a part of the pre-operative investigations for each patient, 3.5 mls of venous blood was obtained into a  C. BODE ET AL. Copyright © 2011 SciRes. SS 23 sterile universal bottle and sent to the Haematology labo- ratory. All samples were serologically screened for HIV/AIDS using the ELISA technique and those found positive were confirmed using the Western Blot metho d. Table 1. Diagnosis of patients seen at paediatric surgery outpatient recruited into the study. Diagnosis Number Percentage Inguinal hernias 181 18.1 Undescended Testes 84 8.4 Hirschsprung’s disease 72 7.2 Posterior Urethral Valves 66 6.6 Umbilical hernia 64 6.4 Anorectal malformation 62 6.2 Intussusception 47 4.7 Omphalocele 44 4.4 Hydrocele 43 4.3 Appendicitis 42 4.2 Hypospadias 41 4.1 Cystic hygroma 29 2.9 Nephroblastoma 22 2.2 Biliary atresia 18 1.8 Thyroglossal cyst 18 1.8 Urethrocutaneous fistula 18 1.8 Tracheoesophageal fistula with oeso- phageal atresia 18 1.8 IHPS 17 1.7 Labial adhesions 15 1.5 Ambiguous genitalia 10 1.0 Uncircumcised phallus 9 0.9 Lipoma 8 0.8 Prune Belly Syndrome 8 0.8 Epispadias 7 0.7 Ankyloglossia 7 0.7 Enterocutaneous fistula 6 0.6 Retractile testes 6 0.6 Appendix mass 5 0.5 Gastroschisis 5 0.5 Arteriovenous malformation 4 0.4 paraphimosis 4 0.4 Hydronephrosis 4 0.4 Phimosis 3 0.3 Bladder extrohpy 2 0.2 Haemangioma 2 0.2 Meatal stenosis 2 0.2 Necrotizing Enterocolitis 2 0.2 Extraperitoneal bladder rupture 1 0.1 Gluteal abscess 1 0.1 Mesenteric lymphadenitis 1 0.1 Splenic cyst 1 0.1 Testicular torsion 1 0.1 Total 1000 100.0 3. Results Five patients out of the 1000 children screened were confirmed positive, using the ELISA technique. Two others were false-positive but excluded by the Western Blot method. Of the 5 sero-positive patients, four were males and one was female. Two of the males had right inguinal hernias, one had posterior urethral valves, one was referred with a right undescended testis at the age of 6 years while the only female patient was first seen with choledochal cyst as a neonate. Tables 2(a) and 2(b) summarizes the information about these patients. 4. Discussion As a developing country, Nigeria’s population is made up mostly of young people, more than 70% of who are under thirty years of age [9]. Nigeria has an estimated population of 140 million with an annual growth rate of 2.38 percent. Thus, about 3 million newborns are added annually [8]. Despite the widespread availability of HIV screening methods in many health-care facilities in this country, ante-natal screening for HIV is not routinely Table 2. Clinical information about seropositive patients. (a) Patient Age (months) Sex Diagnosis Surgery per- formed A 4 M Inguinal hernia Right Inguinal herniotomy B 2.5 M Inguinal hernia Right Inguinal herniotomy C 0.5 M Posterior urethral valves Vesicostomy D 72 M Right un- descended testes Right orchi- dopexy E 1 month Re-presente d at 30 months* F Choledochal cyst Incision and drainage of perinephric abscess (b) Patient Mode of delivery Clinical charac- ter-istics Protective measures during surgery Outcome A SVD Only Mother HIV Positive Universal Precautions alive B SVD Only Mother HIV Positive Universal Precautions alive C SVD Both parents HIV negative Universal Precautions Died D SVD Only Mother HIV Positive Mother died of AIDS Universal Precautions alive E SVD Both parents HIV positive Universal Precautions alive 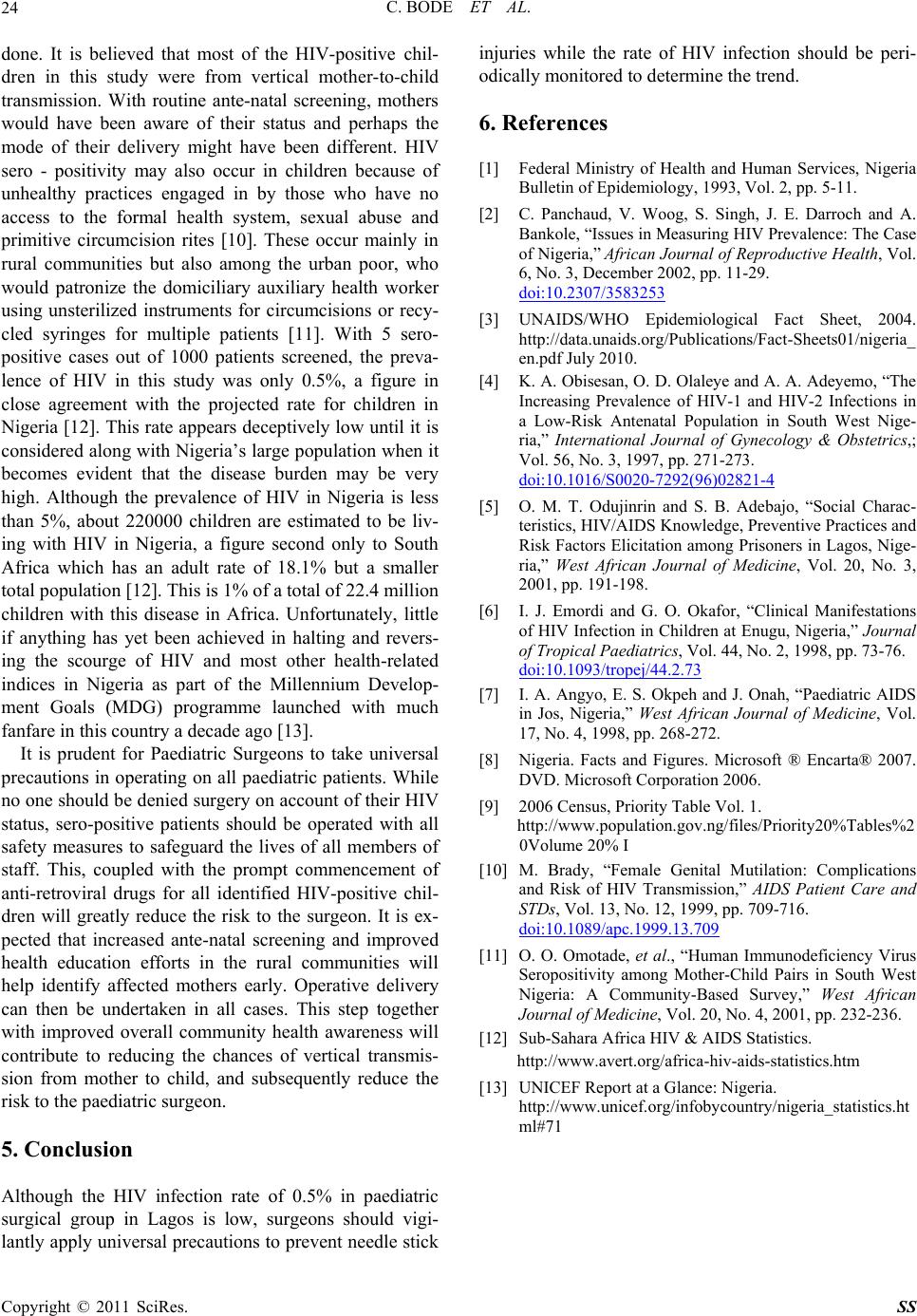 C. BODE ET AL. Copyright © 2011 SciRes. SS 24 done. It is believed that most of the HIV-positive chil- dren in this study were from vertical mother-to-child transmission. With routine ante-natal screening, mothers would have been aware of their status and perhaps the mode of their delivery might have been different. HIV sero - positivity may also occur in children because of unhealthy practices engaged in by those who have no access to the formal health system, sexual abuse and primitive circumcision rites [10]. These occur mainly in rural communities but also among the urban poor, who would patronize the domiciliary auxiliary health worker using unsterilized instruments for circumcisions or recy- cled syringes for multiple patients [11]. With 5 sero- positive cases out of 1000 patients screened, the preva- lence of HIV in this study was only 0.5%, a figure in close agreement with the projected rate for children in Nigeria [12]. This rate appears d eceptively low until it is considered along with Nigeria’s larg e population when it becomes evident that the disease burden may be very high. Although the prevalence of HIV in Nigeria is less than 5%, about 220000 children are estimated to be liv- ing with HIV in Nigeria, a figure second only to South Africa which has an adult rate of 18.1% but a smaller total population [12]. This is 1% of a total of 22.4 million children with this disease in Africa. Unfortunately, little if anything has yet been achieved in halting and revers- ing the scourge of HIV and most other health-related indices in Nigeria as part of the Millennium Develop- ment Goals (MDG) programme launched with much fanfare in this country a decade ago [13]. It is prudent for Paediatric Surgeons to take universal precautions in o perating on all paed iatric patients. While no one should be denied surgery on account of their HIV status, sero-positive patients should be operated with all safety measures to safeguard the lives of all members of staff. This, coupled with the prompt commencement of anti-retroviral drugs for all identified HIV-positive chil- dren will greatly reduce the risk to the surgeon. It is ex- pected that increased ante-natal screening and improved health education efforts in the rural communities will help identify affected mothers early. Operative delivery can then be undertaken in all cases. This step together with improved overall community health awareness will contribute to reducing the chances of vertical transmis- sion from mother to child, and subsequently reduce the risk to the paediatric surgeon. 5. Conclusion Although the HIV infection rate of 0.5% in paediatric surgical group in Lagos is low, surgeons should vigi- lantly apply universal precautions to prevent needle stick injuries while the rate of HIV infection should be peri- odically monitored to determine th e trend. 6. References [1] Federal Ministry of Health and Human Services, Nigeria Bulletin of Epidemiology, 1993, Vol. 2, pp. 5-11. [2] C. Panchaud, V. Woog, S. Singh, J. E. Darroch and A. Bankole, “Issues in Measuring HIV Prevalence: The Case of Nigeria,” African Journal of Reproductive Health, Vol. 6, No. 3, December 2002, pp. 11-29. doi:10.2307/3583253 [3] UNAIDS/WHO Epidemiological Fact Sheet, 2004. http://data.unaids.org/Publications/Fact-Sheets01/nigeria_ en.pdf July 2010. [4] K. A. Obisesan, O. D. Olaleye and A. A. Adeyemo, “The Increasing Prevalence of HIV-1 and HIV-2 Infections in a Low-Risk Antenatal Population in South West Nige- ria,” International Journal of Gynecology & Obstetrics,; Vol. 56, No. 3, 1997, pp. 271-273. doi:10.1016/S0020-7292(96)02821-4 [5] O. M. T. Odujinrin and S. B. Adebajo, “Social Charac- teristics, HIV/AIDS Knowledge, Preventive Practices and Risk Factors Elicitation among Prisoners in Lagos, Nige- ria,” West African Journal of Medicine, Vol. 20, No. 3, 2001, pp. 191-198. [6] I. J. Emordi and G. O. Okafor, “Clinical Manifestations of HIV Infection in Children at Enugu, Nigeria,” Journal of Tropical Paediatrics, Vol. 44, No. 2, 1998, pp. 73-76. doi:10.1093/tropej/44.2.73 [7] I. A. Angyo, E. S. Okpeh and J. Onah, “Paediatric AIDS in Jos, Nigeria,” West African Journal of Medicine, Vol. 17, No. 4, 1998, pp. 268-272. [8] Nigeria. Facts and Figures. Microsoft ® Encarta® 2007. DVD. Microsoft Corporation 2006. [9] 2006 Census, Priority Table Vol. 1. http://www.population.gov.ng/files/Priority20%Tables%2 0Volume 20% I [10] M. Brady, “Female Genital Mutilation: Complications and Risk of HIV Transmission,” AIDS Patient Care and STDs, Vol. 13, No. 12, 1999, pp. 709-716. doi:10.1089/apc.1999.13.709 [11] O. O. Omotade, et al., “Human Immunodeficiency Virus Seropositivity among Mother-Child Pairs in South West Nigeria: A Community-Based Survey,” West African Journal of Medicine, Vol. 20, No. 4, 2001, pp. 232-236. [12] Sub-Sahara Africa HIV & AIDS Statistics. http://www.avert.org/africa-hiv-aids-statistics.htm [13] UNICEF Report at a Glance: Nigeria. http://www.unicef.org/infobycountry/ nigeria_statistics.ht ml#71 |

