S. S. Bucsa, P. I. Calistru / Case Reports in Clinical Medicine 2 (2013) 370-374 371
diagnosis and treatment is imperative to prevent mor-
tality as well as complications.
The long-standing intrabronchial foreignbody presents
problems of diagnosis and treatment which are very
different from those associated with the recently inhaled
foreign body. There may be no history to suggest the
original incident; the clinical picture is usually clouded
by superadded pathological changes-atelectasis, pneu-
monitis, bronchiectasis, or lung bscess-and the broncho-
scopic appearances are often misleading. The symptoms
of aspiration of FB can simulate different diseases such
as asthma, croup or pneumonia, delaying the correct
diagnosis [2]. The delay in the removal of FB is po-
tentially harmful. Even when correctly diagnosed, the
choice of treatment is not always easy. The treatment of
choice for AW is endoscopic removal [2].
Bronchoscopy may be necessary to make a definitive
diagnosis and to remove the object. Prevention remains
the best treatment, but in case of complications anti-
biotics and resp iratory therapy techniques may b e used if
infection develops. Sometimes, for the removal of highly
difficult and high risk tracheobronchial foreign bodies,
preoperative analysis and discussion should be sufficient,
appropriate surgical skill and surgical instruments may
improve the success rate of the surgery and prevent the
operation complications [3].
2. CASE REPORT
A 77-year-old male, smoker (40 pack-year), living in
villages, presented to the clinic with severe dyspnoea,
fever and cough with purulent sputum for about 6
months. He has a history of Chronic Obstructive Pulmo-
nary Disease (COPD) 5 years ago, with two exacerba-
tions in the past year, diabetes mellitus with oral treat-
ment and chronic use of ethanol. Current disease onset
was 6 months ago with cough with purulent sputum,
intermitent fever and chills, shortness of breath. He was
hospitalized in the village with diagnosis of COPD ex-
acerbations, community acquired pneumonia and receiv-
ed antibiotic treatment with Amoxicilin-Clavulanat and
Gentamicin, then Ceftriaxon, with temporary improve-
ment. Then recurrence the simptoms determined repeated
hospitalizations for which he received different antibiotic
regimens, but they have not helped. A few days before
presenting to hospital , the symptoms worsened, the pa-
tient presenting malaise, severe dyspnoea with weezing,
fever and cough with purulent sputum. Physical exami-
nation on admission: General appearance: underweight;
Respirator stetacustic. prolonged expiration, weezing,
bronchial rales crackles in lower right lung, SaO2 = 91%
- 93%; Febrile, T = 38 .5˚C; Vital signs: in normal limits;
No other significant signs revealed. Blood tests showed:
leucocytes 17.800/mm3, with neutrophils 9.900/mm3;
VSH = 68/105 mm/h/2h; CRP = 8.68 mg/dl; Fibrinogen
= 785 mg/dl; TGP, TGO, Glycemia, BUN within normal
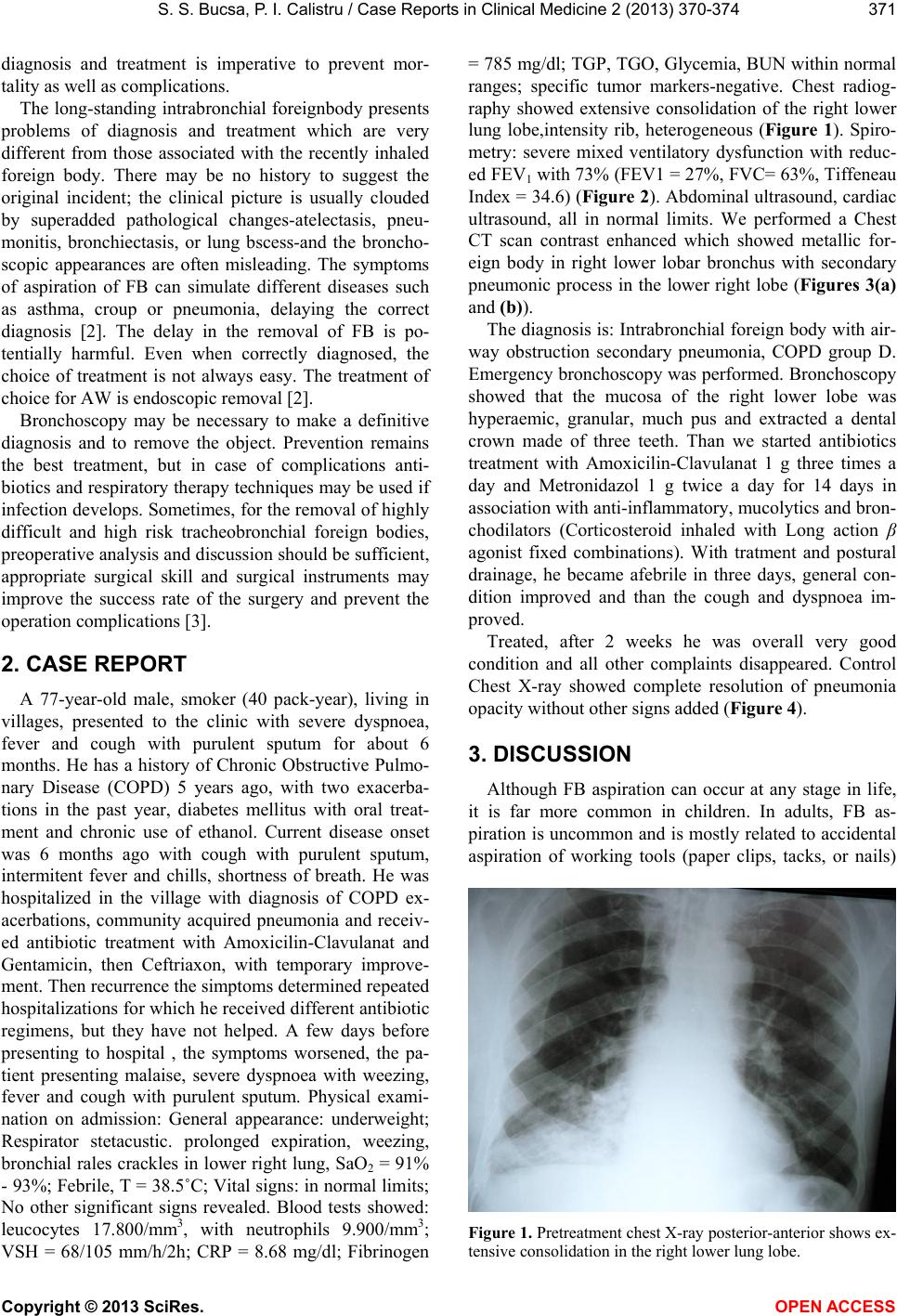
ranges; specific tumor markers-negative. Chest radiog-
raphy showed extensive consolidation of the right lower
lung lobe,intensity rib, heterogeneous (Figure 1). Spiro-
metry: severe mixed ventilatory dysfunction with reduc-
ed FEV1 with 73% (FEV1 = 27%, FVC= 63%, Tiffeneau
Index = 34.6) (Figure 2). Abdominal ultrasound, cardiac
ultrasound, all in normal limits. We performed a Chest
CT scan contrast enhanced which showed metallic for-
eign body in right lower lobar bronchus with secondary
pneumonic process in the lower right lobe (Figures 3(a)
and (b)).
The diagnosis is: Intrabron chial foreign body with air-
way obstruction secondary pneumonia, COPD group D.
Emergency bronchoscopy was performed. Bronchoscopy
showed that the mucosa of the right lower lobe was
hyperaemic, granular, much pus and extracted a dental
crown made of three teeth. Than we started antibiotics
treatment with Amoxicilin-Clavulanat 1 g three times a
day and Metronidazol 1 g twice a day for 14 days in
association with anti-inflammatory, mucolyti cs and bron-
chodilators (Corticosteroid inhaled with Long action β
agonist fixed combinations). With tratment and postural
drainage, he became afebrile in three days, general con-
dition improved and than the cough and dyspnoea im-
proved.
Treated, after 2 weeks he was overall very good
condition and all other complaints disappeared. Control
Chest X-ray showed complete resolution of pneumonia
opacity without other signs added (Figure 4).
3. DISCUSSION
Although FB aspiration can occur at any stage in life,
it is far more common in children. In adults, FB as-
piration is uncommon and is mostly related to accidental
aspiration of working tools (paper clips, tacks, or nails)
Figure 1. Pretreatment chest X-ray posterior-anterior shows ex-
ensive consolidation in the right lower lung lobe. t
Copyright © 2013 SciRes. OPEN ACCESS