Paper Menu >>
Journal Menu >>
 Surgical Science, 2011, 2, 5-7 doi:10.4236/ss.2011.21002 Published Online January 2011 (http://www.SciRP.org/journal/ss) Copyright © 2011 SciRes. SS Can Mucosectomy be Always Performed in Complicated Cases of Choledochal Cysts Sezen Özkisacik1, Mesut Yazici1, Canten Tataroglu2, Yelda Ozsunar3, Harun Gürsoy1 1Adnan Menderes University, Medical Faculty, Department of Pediatric Su rgery, Aydin, Turkey 2Adnan Menderes University, Medical Faculty, Depart me nt of Pat h ol o gy, Aydin , T urkey 3Adnan Menderes University, Medical Faculty, Department of Radiodiagnostic, Aydin, Turkey E-mail: sozkisacik@adu.edu.tr Received September 9, 2010; September 18, 201 0; September 25, 2010 Abstract Introduction: If the surgical dissection is too risky in choledochal cyst, mucosectomy is defined as a benefi- cial technical method in the literature. To discuss in this manner, we present this case. Case: 9 y ears old girl was referred to our clinic due to multipl stones in the gallbladder. History and physicial examination could not be performed effectively because of her cerebral palsy. Ultrasonography showed choledochal cyst con- taining multipl stones. MR cholangiography showed multipl stones in the dilated choledochus. During the dissection, the cyst appeared extremely adherent to the adjacent structures and cyst wall was so thin and transparent. The mucosectomy was not thought to be a good option to carry out for this case. For this reason, cyst was totally excised. Discussion: The preferred method for choledochal cyst is total cyst excision and Roux-en Y hepaticoenterostomy. When the dissection is unsafe to perform, posterior wall mucosectomy may be performed. However, like in our case, when the diagnosis is delayed, the cyst wall may become too thin and may be attached very strongly to the adjacent structures. So, mucosectomy is impossible and full layer total cyst excision remains as the only alternative in spite of its high risks. Keywords: Mucosectomy, Choledoch, Cyst 1. Introduction Choledochal cysts are rare congenital anomalies of the biliary tree [1]. Since every piece of unresected remains of the cystic wall is associated with malignan cies [2], the method of choice for the treatment of choledochal cysts in children is total resection and Roux-en-Y (RY) hepa- ticoenterostomy to prevent carcinogenesis of biliary duckts [3]. If there is inflammation in the cystic wall, if the cyst is excessively inflated and if it is adhered to sur- rounding tissue excessively, total resection may not be possible. Since surgical resection of the posterior wall may cause excessive risk in such cases, excision of the cyst mucosa (mucosectomy), a technique which facili- tates the operation and renders excision more successful, has been descri bed [4,5]. We will present a case of choledochal cyst found to have no specific findings, but difficulty in orientation due to cerebral palsy on history and physical examina- tion and treated with full thickness total resection. 2. Case A nine-year-old girl was referred to our center for multiple calculi in her gallb ladder detected o n abdo minal ultrasonography (USG) and computed tomography (CT). On history, she frequently presented with restlessness to several health centers; however, it turned out that effec- tive examination could not be performed and that history could not be taken because she had cerebral palsy since she was two years old. In our emergency department, physical examination could not be carried out properly. Direct abdominal x-ray taken when the patient was standing showed two air-fluid levels on the right upper quadrant. Therefore, abdominal USG was repeated and then magnetic reso- nance (MR) cholangiography was performed. USG and MR cholangiography demonstrated a choledochal cyst containing multiple calculi (Figure 1). The patient un- derwent operation. On intraoperative USG and cholan- giography, the cyst was about 7-8 cm in length and 5 cm in width and connected to the pancreas via 1.5 cm- 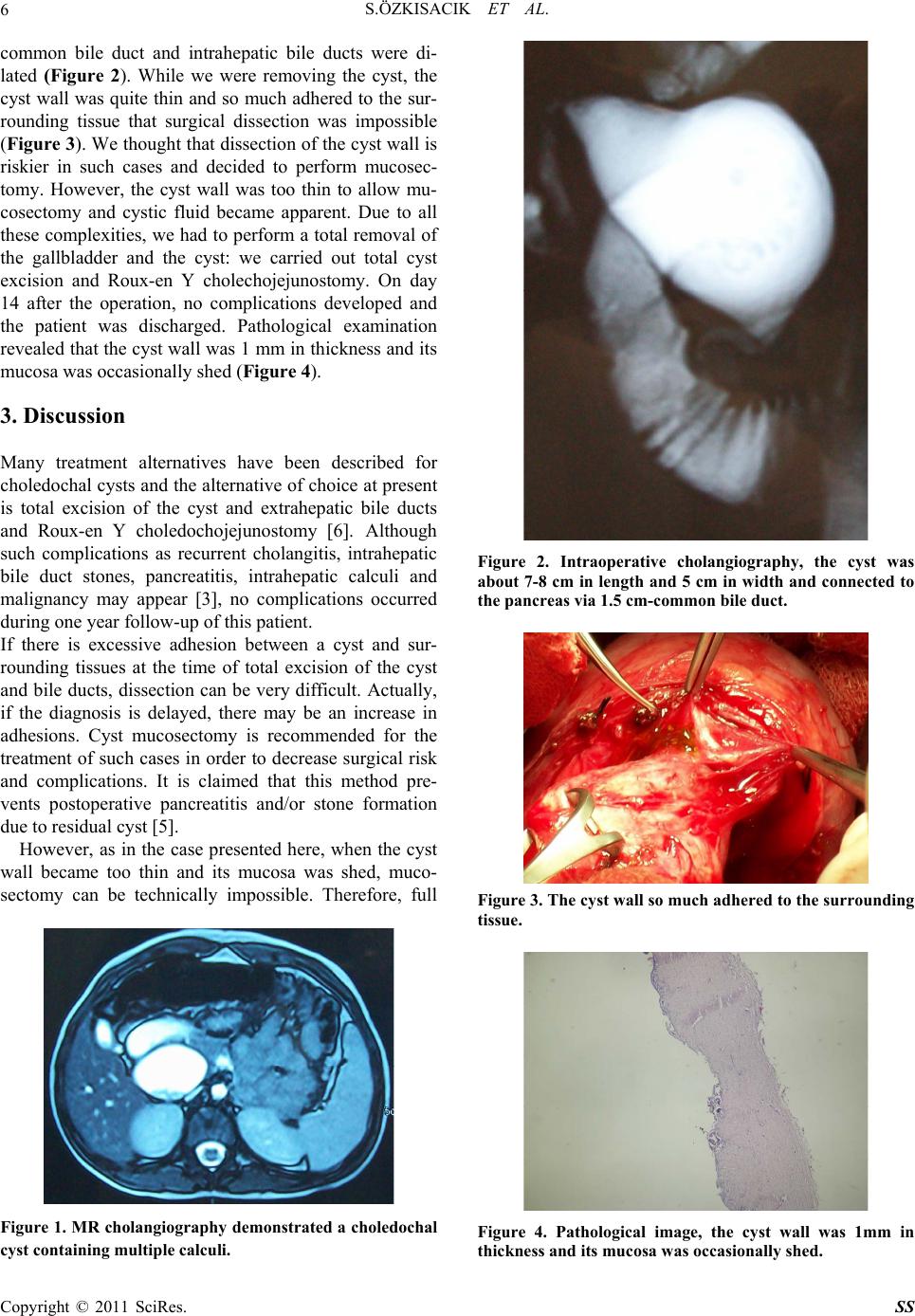 S.ÖZKISACIK ET AL. Copyright © 2011 SciRes. SS 6 common bile duct and intrahepatic bile ducts were di- lated (Figure 2). While we were removing the cyst, the cyst wall was quite thin and so much adhered to the sur- rounding tissue that surgical dissection was impossible (Figure 3). We thought that dissection of the cyst wall is riskier in such cases and decided to perform mucosec- tomy. However, the cyst wall was too thin to allow mu- cosectomy and cystic fluid became apparent. Due to all these complexities, we had to perform a total removal of the gallbladder and the cyst: we carried out total cyst excision and Roux-en Y cholechojejunostomy. On day 14 after the operation, no complications developed and the patient was discharged. Pathological examination revealed that the cyst wall was 1 mm in thic kness and its mucosa was occasionally shed (Figure 4). 3. Discussion Many treatment alternatives have been described for choledochal cysts and the alternative of choice at present is total excision of the cyst and extrahepatic bile ducts and Roux-en Y choledochojejunostomy [6]. Although such complications as recurrent cholangitis, intrahepatic bile duct stones, pancreatitis, intrahepatic calculi and malignancy may appear [3], no complications occurred during one year fo llow-up of this patient. If there is excessive adhesion between a cyst and sur- rounding tissues at the time of total excision of the cyst and bile ducts, dissection can be very difficult. Actually, if the diagnosis is delayed, there may be an increase in adhesions. Cyst mucosectomy is recommended for the treatment of such cases in order to decrease surgical risk and complications. It is claimed that this method pre- vents postoperative pancreatitis and/or stone formation due to residual cyst [5]. However, as in the case presented here, when the cyst wall became too thin and its mucosa was shed, muco- sectomy can be technically impossible. Therefore, full Figure 1. MR cholangiography demonstrated a choledochal cyst containing multi p le ca l c uli. Figure 2. Intraoperative cholangiography, the cyst was about 7-8 cm in length and 5 cm in width and connected to the pancreas via 1.5 cm-common bile duct. Figure 3. The cyst wall so much adhered to the surrounding tissue. Figure 4. Pathological image, the cyst wall was 1mm in thickness and its mucosa was occ a sionally she d. 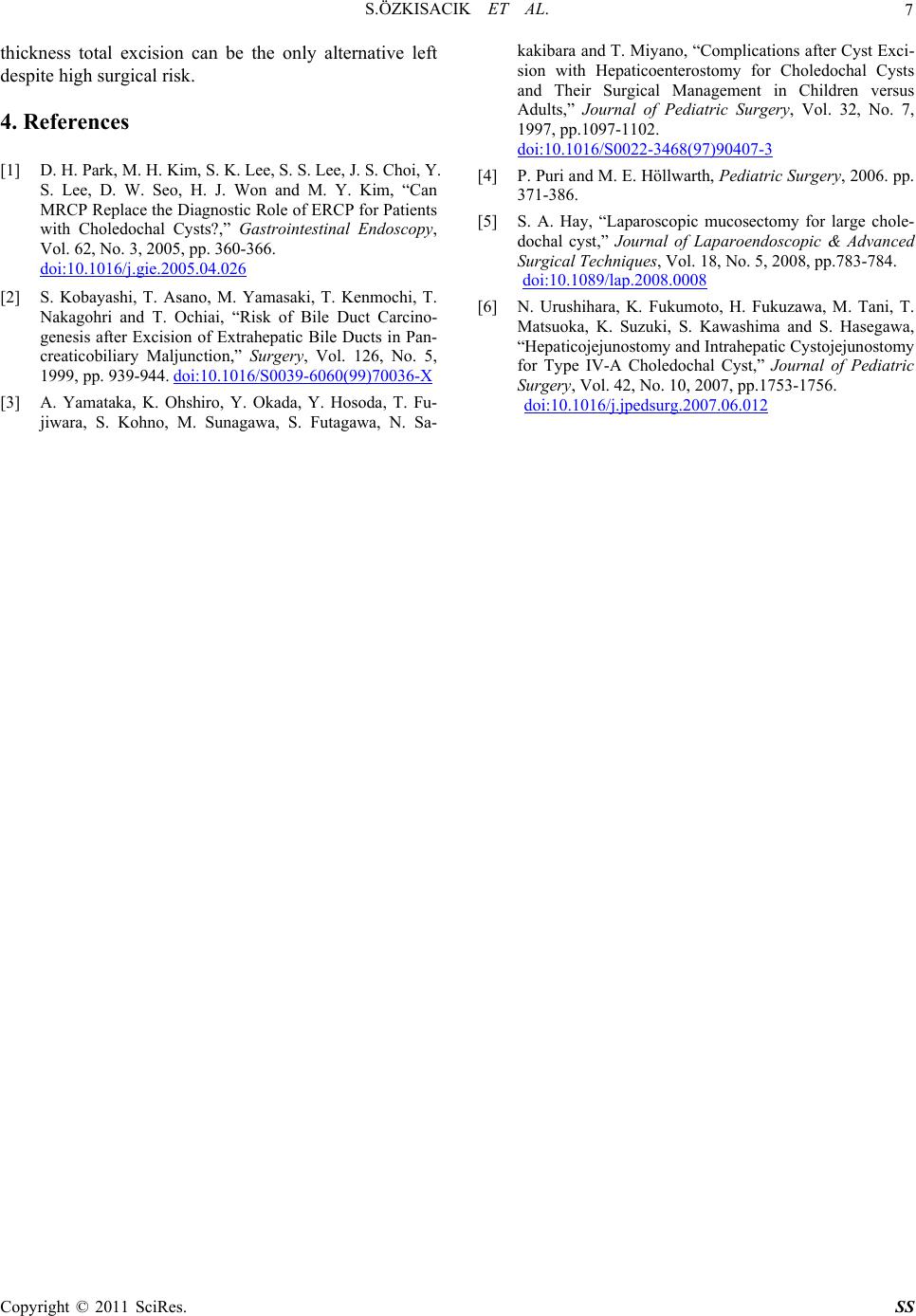 S.ÖZKISACIK ET AL. Copyright © 2011 SciRes. SS 7 thickness total excision can be the only alternative left despite high surgical risk. 4. References [1] D. H. Park, M. H. Kim, S. K. Lee, S. S. Lee, J. S. Choi, Y. S. Lee, D. W. Seo, H. J. Won and M. Y. Kim, “Can MRCP Replace the Diagnostic Role of ERCP for Patients with Choledochal Cysts?,” Gastrointestinal Endoscopy, Vol. 62, No. 3, 2005, pp. 360-366. doi:10.1016/j.gie.2005.04.026 [2] S. Kobayashi, T. Asano, M. Yamasaki, T. Kenmochi, T. Nakagohri and T. Ochiai, “Risk of Bile Duct Carcino- genesis after Excision of Extrahepatic Bile Ducts in Pan- creaticobiliary Maljunction,” Surgery, Vol. 126, No. 5, 1999, pp. 939-944. doi:10.1016/S0039-6060(99)70036-X [3] A. Yamataka, K. Ohshiro, Y. Okada, Y. Hosoda, T. Fu- jiwara, S. Kohno, M. Sunagawa, S. Futagawa, N. Sa- kakibara and T. Miyano, “Complications after Cyst Exci- sion with Hepaticoenterostomy for Choledochal Cysts and Their Surgical Management in Children versus Adults,” Journal of Pediatric Surgery, Vol. 32, No. 7, 1997, pp.1097-1102. doi:10.1016/S0022-3468(97)90407-3 [4] P. Puri and M. E. Höllwarth, Pediatric Surgery, 2006. pp. 371-386. [5] S. A. Hay, “Laparoscopic mucosectomy for large chole- dochal cyst,” Journal of Laparoendoscopic & Advanced Surgical Techniques, Vol. 18, No. 5, 2008, pp.783-784. doi:10.1089/lap.2008.0008 [6] N. Urushihara, K. Fukumoto, H. Fukuzawa, M. Tani, T. Matsuoka, K. Suzuki, S. Kawashima and S. Hasegawa, “Hepaticojejunostomy and Intrahepatic Cystojejunostomy for Type IV-A Choledochal Cyst,” Journal of Pediatric Surgery, Vol. 42, No. 10, 2007, pp.1753-1756. doi:10.1016/j.jpedsurg.2007.06.012 |

