M. BUDRUDDIN ET AL.
150
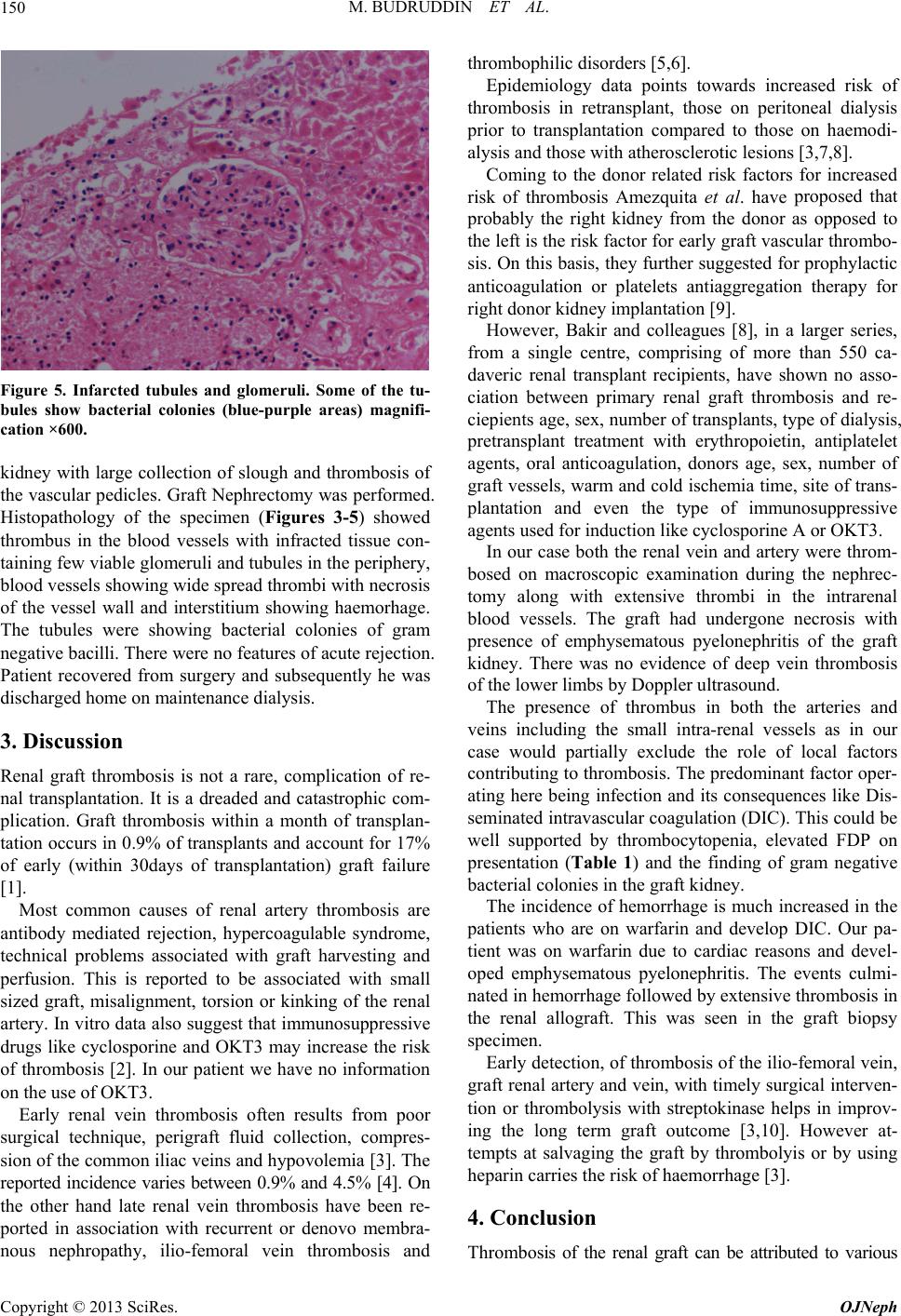
Figure 5. Infarcted tubules and glomeruli. Some of the tu-
bules show bacterial colonies (blue-purple areas) magnifi-
cation ×600.
kidney with large collection of slough and thrombosis of
the vascular pedicles. Graft Nephrectomy was performed.
Histopathology of the specimen (Figures 3-5) showed
thrombus in the blood vessels with infracted tissue con-
taining few viable glomeruli and tubules in th e periphery,
blood vessels sh owing wide sp read th ro mbi with ne cros is
of the vessel wall and interstitium showing haemorhage.
The tubules were showing bacterial colonies of gram
negative bacilli. Th ere were no features of acu te rejection .
Patient recovered from surgery and subsequently he was
discharged home on maintenance dialysis.
3. Discussion
Renal graft thrombosis is not a rare, complication of re-
nal transplantation. It is a dreaded and catastrophic com-
plication. Graft thrombosis within a month of transplan-
tation occurs in 0.9% of transplants and account for 17%
of early (within 30days of transplantation) graft failure
[1].
Most common causes of renal artery thrombosis are
antibody mediated rejection, hypercoagulable syndrome,
technical problems associated with graft harvesting and
perfusion. This is reported to be associated with small
sized graft, misalignment, torsion or kinking of the renal
artery. In vitro data also suggest that immunosuppressive
drugs like cyclosporine and OKT3 may increase the risk
of thrombosis [2]. In our patient we have no information
on the use of OKT3.
Early renal vein thrombosis often results from poor
surgical technique, perigraft fluid collection, compres-
sion of the common iliac veins and hypovolemia [3]. The
reported incidence varies between 0.9% and 4.5% [4]. On
the other hand late renal vein thrombosis have been re-
ported in association with recurrent or denovo membra-
nous nephropathy, ilio-femoral vein thrombosis and
thrombophilic disorders [5,6].
Epidemiology data points towards increased risk of
thrombosis in retransplant, those on peritoneal dialysis
prior to transplantation compared to those on haemodi-
alysis and those with atherosclerotic lesions [3,7,8].
Coming to the donor related risk factors for increased
risk of thrombosis Amezquita et al. have proposed that
probably the right kidney from the donor as opposed to
the left is the risk factor for early graft vascular thrombo-
sis. On this basis, they further sugge sted for prophylactic
anticoagulation or platelets antiaggregation therapy for
right donor kidney implantation [9].
However, Bakir and colleagues [8], in a larger series,
from a single centre, comprising of more than 550 ca-
daveric renal transplant recipients, have shown no asso-
ciation between primary renal graft thrombosis and re-
ciepients age, sex, number of transplants, type of dialysis,
pretransplant treatment with erythropoietin, antiplatelet
agents, oral anticoagulation, donors age, sex, number of
graft vessels, warm and cold ischemia time, site of trans-
plantation and even the type of immunosuppressive
agents used for in duction like cyclosporine A or OKT3 .
In our case both the renal vein and artery were throm-
bosed on macroscopic examination during the nephrec-
tomy along with extensive thrombi in the intrarenal
blood vessels. The graft had undergone necrosis with
presence of emphysematous pyelonephritis of the graft
kidney. There was no evidence of deep vein thrombosis
of the lower limbs by Doppler ultrasound.
The presence of thrombus in both the arteries and
veins including the small intra-renal vessels as in our
case would partially exclude the role of local factors
contributing to thrombo sis. The predominant factor oper-
ating here being infection and its consequences like Dis-
seminated intravascular coagu lation (DIC). This could be
well supported by thrombocytopenia, elevated FDP on
presentation (Table 1) and the finding of gram negative
bacterial colonies in the graft kidney.
The incidence of hemorrhage is much increased in the
patients who are on warfarin and develop DIC. Our pa-
tient was on warfarin due to cardiac reasons and devel-
oped emphysematous pyelonephritis. The events culmi-
nated in hemorrhage followed by extensive thrombosis in
the renal allograft. This was seen in the graft biopsy
specimen.
Early detection, of thrombos is of the ilio-femoral vein,
graft renal artery and vein, with timely surgical interven -
tion or thrombolysis with streptokinase helps in improv-
ing the long term graft outcome [3,10]. However at-
tempts at salvaging the graft by thrombolyis or by using
heparin carries the ri sk of haemorrhage [3].
4. Conclusion
Thrombosis of the renal graft can be attributed to various
Copyright © 2013 SciRes. OJNeph