M. ABEBE ET AL.
118
C4, antineutrophil cytoplasmic antibodies, Anti ds DNA
antibodies were negative. Urinalysis showed large leuko-
cyte esterase, WBC > 182 and protein 100 mg/dL. Urine
culture was negative.
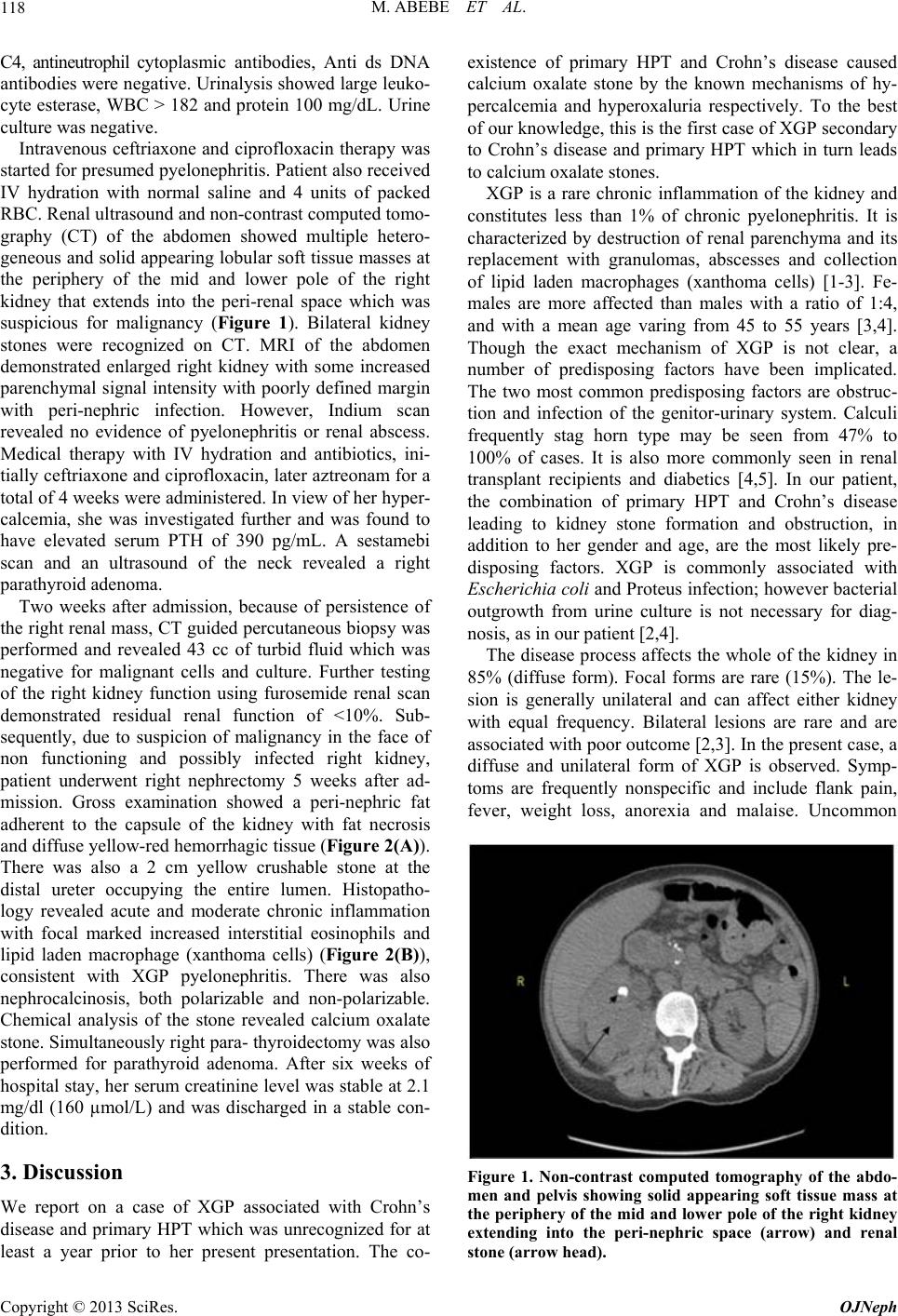
Intravenous ceftriaxone and ciprofloxacin therapy was
started for presumed pyelonephritis. Patient also received
IV hydration with normal saline and 4 units of packed
RBC. Renal ultrasound and non-co ntrast computed tomo-
graphy (CT) of the abdomen showed multiple hetero-
geneous and solid app earing lobular soft tissue masses at
the periphery of the mid and lower pole of the right
kidney that extends into the peri-renal space which was
suspicious for malignancy (Figure 1). Bilateral kidney
stones were recognized on CT. MRI of the abdomen
demonstrated enlarged right kidney with some increased
parenchymal signal intensity with poorly defined margin
with peri-nephric infection. However, Indium scan
revealed no evidence of pyelonephritis or renal abscess.
Medical therapy with IV hydration and antibiotics, ini-
tially ceftriaxone and ciprofloxacin, later aztreonam for a
total of 4 weeks were administered. In view of her hyper-
calcemia, she was investigated further and was found to
have elevated serum PTH of 390 pg/mL. A sestamebi
scan and an ultrasound of the neck revealed a right
parathyroid adenoma.
Two weeks after admission, because of persistence of
the right renal mass, CT guided percutaneous biopsy was
performed and revealed 43 cc of turbid fluid which was
negative for malignant cells and culture. Further testing
of the right kidney function using furosemide renal scan
demonstrated residual renal function of <10%. Sub-
sequently, due to suspicion of malignancy in the face of
non functioning and possibly infected right kidney,
patient underwent right nephrectomy 5 weeks after ad-
mission. Gross examination showed a peri-nephric fat
adherent to the capsule of the kidney with fat necrosis
and diffuse yellow-red hemorrhagic tissue (Figure 2(A)).
There was also a 2 cm yellow crushable stone at the
distal ureter occupying the entire lumen. Histopatho-
logy revealed acute and moderate chronic inflammation
with focal marked increased interstitial eosinophils and
lipid laden macrophage (xanthoma cells) (Figure 2(B)),
consistent with XGP pyelonephritis. There was also
nephrocalcinosis, both polarizable and non-polarizable.
Chemical analysis of the stone revealed calcium oxalate
stone. Simultaneously right para- thyroidectomy was also
performed for parathyroid adenoma. After six weeks of
hospital stay, her serum creatinine level was stable at 2.1
mg/dl (160 µmol/L) and was discharged in a stable con-
dition.
3. Discussion
We report on a case of XGP associated with Crohn’s
disease and primary HPT which was unrecognized for at
least a year prior to her present presentation. The co-
existence of primary HPT and Crohn’s disease caused
calcium oxalate stone by the known mechanisms of hy-
percalcemia and hyperoxaluria respectively. To the best
of our knowledg e, this is the first case of XGP secondary
to Crohn’s disease and primary HPT which in turn leads
to calcium oxalate stones.
XGP is a rare chronic inflammation of the kidney and
constitutes less than 1% of chronic pyelonephritis. It is
characterized by destruction of renal parenchyma and its
replacement with granulomas, abscesses and collection
of lipid laden macrophages (xanthoma cells) [1-3]. Fe-
males are more affected than males with a ratio of 1:4,
and with a mean age varing from 45 to 55 years [3,4].
Though the exact mechanism of XGP is not clear, a
number of predisposing factors have been implicated.
The two most common predisposing factors are obstruc-
tion and infection of the genitor-urinary system. Calculi
frequently stag horn type may be seen from 47% to
100% of cases. It is also more commonly seen in renal
transplant recipients and diabetics [4,5]. In our patient,
the combination of primary HPT and Crohn’s disease
leading to kidney stone formation and obstruction, in
addition to her gender and age, are the most likely pre-
disposing factors. XGP is commonly associated with
Escherichia coli and Proteus infection; however bacterial
outgrowth from urine culture is not necessary for diag-
nosis, as in our patient [2,4].
The disease process affects the whole of the kidney in
85% (diffuse form). Focal forms are rare (15%). The le-
sion is generally unilateral and can affect either kidney
with equal frequency. Bilateral lesions are rare and are
associated with poor outcome [2,3]. In the present case, a
diffuse and unilateral form of XGP is observed. Symp-
toms are frequently nonspecific and include flank pain,
fever, weight loss, anorexia and malaise. Uncommon
Figure 1. Non-contrast computed tomography of the abdo-
men and pelvis showing solid appearing soft tissue mass at
the periphery of the mid and lower pole of the right kidney
extending into the peri-nephric space (arrow) and renal
stone (arrow head).
Copyright © 2013 SciRes. OJNeph