Impact of Ocular Compression on Ocular Surface Bacterial Contaminat i on
376
OC (approximately 30 mm Hg) for 15 ± 2 minutes using
a modified Honan’s balloon, and the control group (31
eyes of 31 patients) received retrobulbar anaesthesia
without the preoperative application of OC or digital
massage. In the control group, the patients’ eyes re-
mained closed for 15 ± 2 minutes after the anaesthesia
administration. Approval for accessing the patient health
records was obtained from the local research ethics
committee. Informed consent was obtained from each
patient. The study protocol and the safety and efficacy of
the intervention s were explained to all of the participants
prior to their enrolment.
2.2. Bacteriological Investigation
After the specified period of 15 ± 2 minutes and follow-
ing the device removal (study group only), the eyes were
opened, and bacterial cultures from the conjunctival sac
and lid margin were immediately initiated using sterile
cotton swabs moistened with sterile saline solution. In
addition, swabbing was performed for the lower lid
margin by rolling the swab from the lateral canthus up to
the lacrimal point. The samples from each eye were
placed in separate tubes containing thioglycolate broth
and incubated at 37˚C for 24 h. The bacterial isolation
and identification were performed using standard me-
thods, as described elsewhere [4].
2.3. Statistical Analysis
The chi-squared test was used to compare the studied
variables. A P value less than 0.05 was considered statis-
tically significant.
3. Results
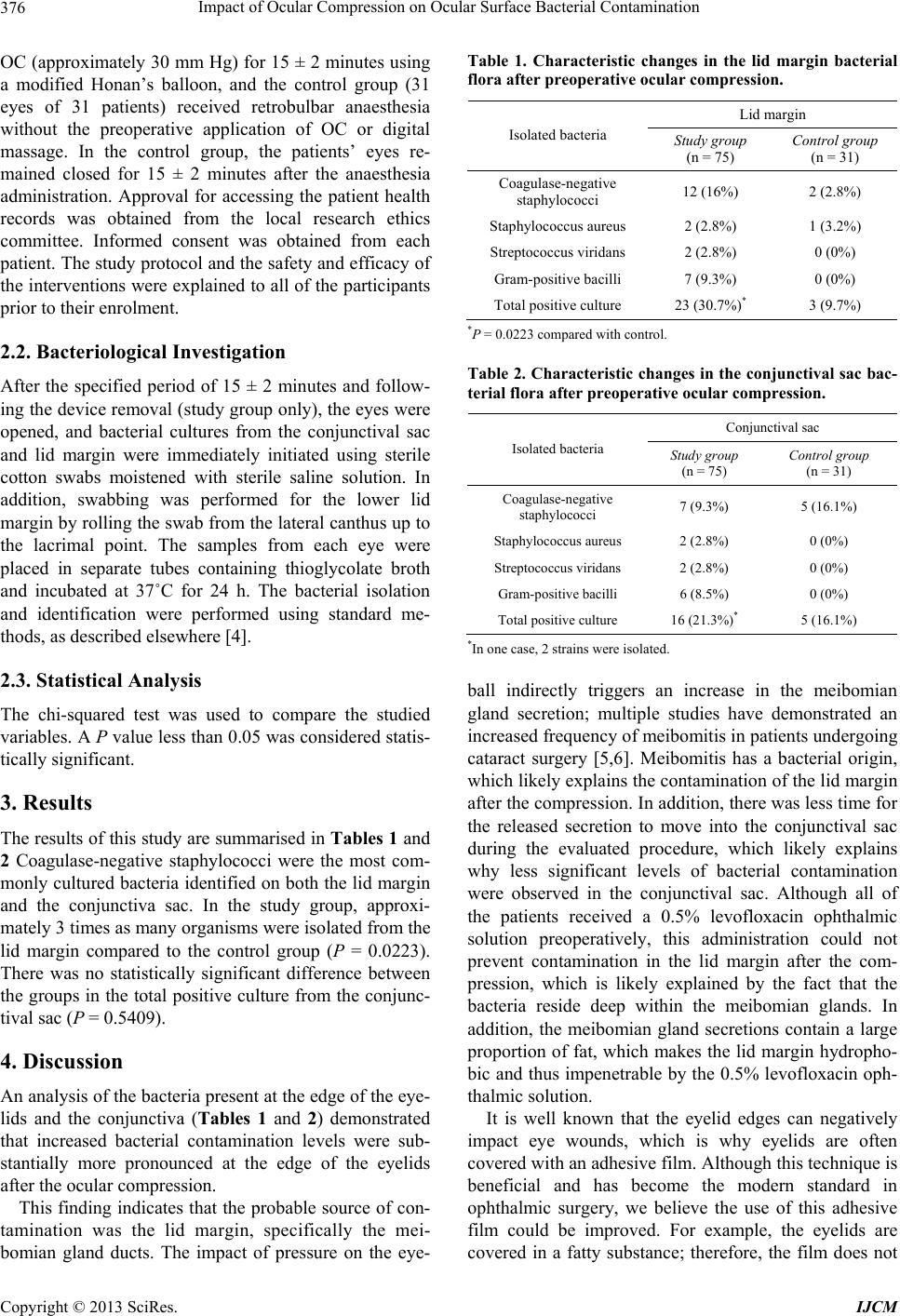
The results of this study are summarised in Tables 1 and
2 Coagulase-negative staphylococci were the most com-
monly cultured bacteria identified on both the lid margin
and the conjunctiva sac. In the study group, approxi-
mately 3 times as many organisms were isolated from the
lid margin compared to the control group (P = 0.0223).
There was no statistically significant difference between
the groups in the total positive culture from the conjunc-
tival sac (P = 0.5409).
4. Discussion
An analysis of the bacteria present at the edge of the eye-
lids and the conjunctiva (Tables 1 and 2) demonstrated
that increased bacterial contamination levels were sub-
stantially more pronounced at the edge of the eyelids
after the ocular compression.
This finding indicates that the probable source of con-
tamination was the lid margin, specifically the mei-
bomian gland ducts. The impact of pressure on the eye-
Table 1. Characteristic changes in the lid margin bacterial
flora after preoperative ocular compression.
Lid margin
Isolated bacteria Study group
(n = 75) Control group
(n = 31)
Coagulase-negative
staphylococci 12 (16%) 2 (2.8%)
Staphylococcus aureus 2 (2.8%) 1 (3.2%)
Streptococcus viridans 2 (2.8%) 0 (0%)
Gram-positive bacilli 7 (9.3%) 0 (0%)
Total positive culture 23 (30.7%)* 3 (9.7%)
*P = 0.0223 compared with control.
Table 2. Characteristic changes in the conjunctival sac bac-
terial flora after preoperative ocular compression.
Conjunctival sac
Isolated bacteria Stu dy group
(n = 75) Control group
(n = 31)
Coagulase-negative
staphylococci 7 (9.3%) 5 (16.1%)
Staphylococcus aureus 2 (2.8%) 0 (0%)
Streptococcus viridans 2 (2.8%) 0 (0%)
Gram-posi t iv e bacilli 6 (8.5%) 0 (0%)
Total positive culture 16 (21.3%)* 5 (16.1%)
*In one cas e, 2 strains were isolated.
ball indirectly triggers an increase in the meibomian
gland secretion; multiple studies have demonstrated an
increased frequency of meibomitis in patients undergoing
cataract surgery [5,6]. Meibomitis has a bacterial origin,
which likely exp lains the contamination o f the lid margin
after the compression. In addition, there was less time for
the released secretion to move into the conjunctival sac
during the evaluated procedure, which likely explains
why less significant levels of bacterial contamination
were observed in the conjunctival sac. Although all of
the patients received a 0.5% levofloxacin ophthalmic
solution preoperatively, this administration could not
prevent contamination in the lid margin after the com-
pression, which is likely explained by the fact that the
bacteria reside deep within the meibomian glands. In
addition, the meibomian gland secretions contain a large
proportion of fat, which makes the lid margin hydropho-
bic and thus impenetrable by the 0.5% levofloxacin oph-
thalmic solution.
It is well known that the eyelid edges can negatively
impact eye wounds, which is why eyelids are often
covered with an adhesive film. Although this technique is
beneficial and has become the modern standard in
ophthalmic surgery, we believe the use of this adhesive
film could be improved. For example, the eyelids are
covered in a fatty substance; therefore, the film does not
Copyright © 2013 SciRes. IJCM