Y. Motooka et al. / Case Reports in Clinical Medicine 2 (2013) 335-337
336
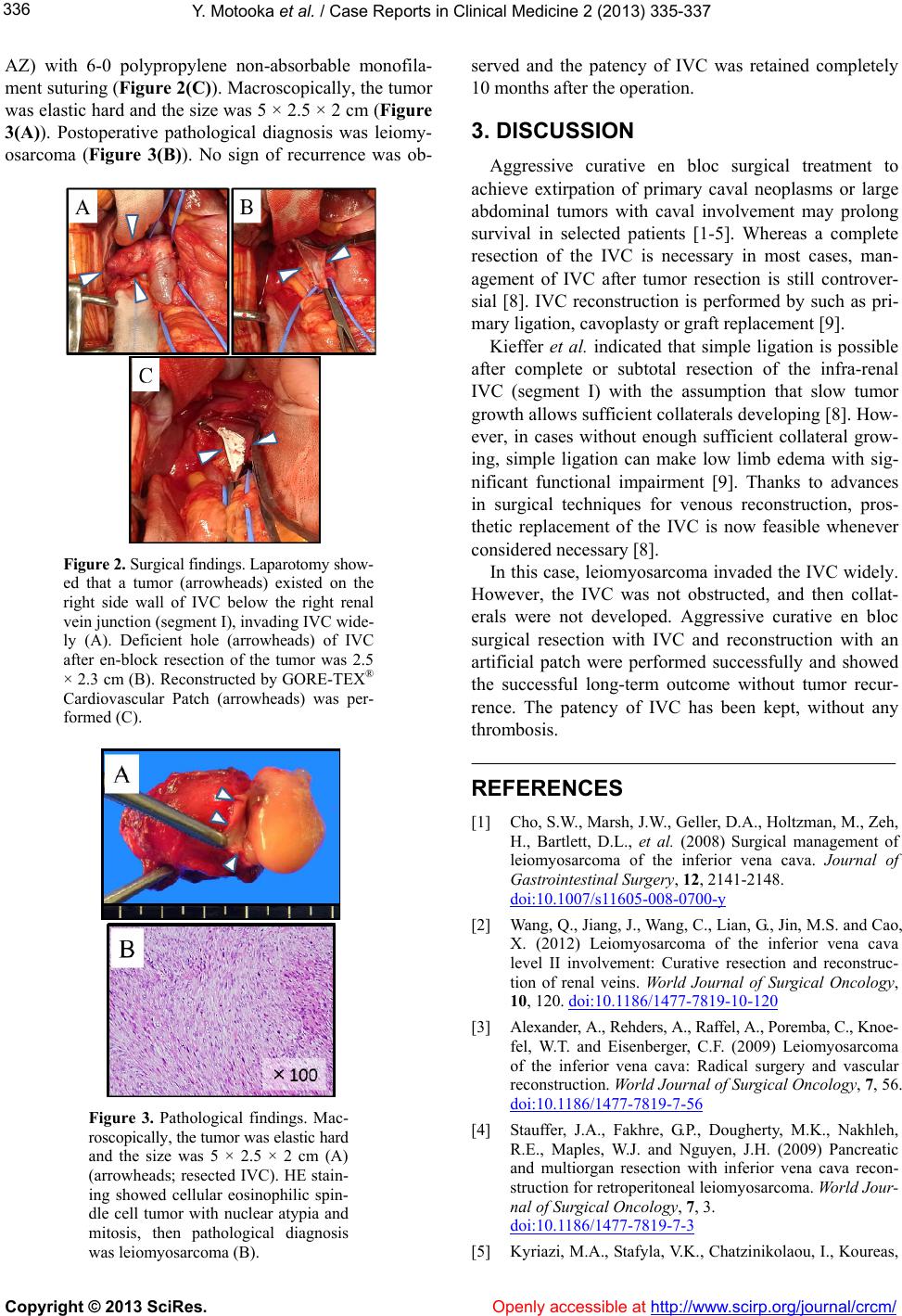
AZ) with 6-0 polypropylene non-absorbable monofila-
ment suturing (Figure 2(C)). Macroscopically, the tumor
was elastic hard and the size was 5 × 2.5 × 2 cm (Figure
3(A)). Postoperative pathological diagnosis was leiomy-
osarcoma (Figure 3(B)). No sign of recurrence was ob-
Figure 2. Surgical findings. Laparotomy show-
ed that a tumor (arrowheads) existed on the
right side wall of IVC below the right renal
vein junction (segment I), invading IVC wide-
ly (A). Deficient hole (arrowheads) of IVC
after en-block resection of the tumor was 2.5
× 2.3 cm (B). Reconstructed by GORE-TEX®
Cardiovascular Patch (arrowheads) was per-
formed (C).
Figure 3. Pathological findings. Mac-
roscopically, the tumor was elastic hard
and the size was 5 × 2.5 × 2 cm (A)
(arrowheads; resected IVC). HE stain-
ing showed cellular eosinophilic spin-
dle cell tumor with nuclear atypia and
mitosis, then pathological diagnosis
was leiomyosarcoma (B).
served and the patency of IVC was retained completely
10 months after the operation.
3. DISCUSSION
Aggressive curative en bloc surgical treatment to
achieve extirpation of primary caval neoplasms or large
abdominal tumors with caval involvement may prolong
survival in selected patients [1-5]. Whereas a complete
resection of the IVC is necessary in most cases, man-
agement of IVC after tumor resection is still controver-
sial [8]. IVC reconstruction is performed by such as pri-
mary ligation, cavoplasty or graft replacement [9].
Kieffer et al. indicated that simple ligation is possible
after complete or subtotal resection of the infra-renal
IVC (segment I) with the assumption that slow tumor
growth allows sufficient collaterals developing [8]. How-
ever, in cases without enough sufficient collateral grow-
ing, simple ligation can make low limb edema with sig-
nificant functional impairment [9]. Thanks to advances
in surgical techniques for venous reconstruction, pros-
thetic replacement of the IVC is now feasible whenever
considered necessary [8].
In this case, leiomyosarcoma invaded the IVC widely.
However, the IVC was not obstructed, and then collat-
erals were not developed. Aggressive curative en bloc
surgical resection with IVC and reconstruction with an
artificial patch were performed successfully and showed
the successful long-term outcome without tumor recur-
rence. The patency of IVC has been kept, without any
thrombosis.
REFERENCES
[1] Cho, S.W., Marsh, J.W., Geller, D.A., Holtzman, M., Zeh,
H., Bartlett, D.L., et al. (2008) Surgical management of
leiomyosarcoma of the inferior vena cava. Journal of
Gastrointestinal Surger y, 12, 2141-2148.
doi:10.1007/s11605-008-0700-y
[2] Wang, Q., Jiang, J., Wang, C., Lian, G., Jin, M.S. and Cao,
X. (2012) Leiomyosarcoma of the inferior vena cava
level II involvement: Curative resection and reconstruc-
tion of renal veins. World Journal of Surgical Oncology,
10, 120. doi:10.1186/1477-7819-10-120
[3] Alexander, A., Rehders, A., Raffel, A., Poremba, C., Knoe-
fel, W.T. and Eisenberger, C.F. (2009) Leiomyosarcoma
of the inferior vena cava: Radical surgery and vascular
reconstruction. World Journal of Surgical Oncology, 7, 56.
doi:10.1186/1477-7819-7-56
[4] Stauffer, J.A., Fakhre, G.P., Dougherty, M.K., Nakhleh,
R.E., Maples, W.J. and Nguyen, J.H. (2009) Pancreatic
and multiorgan resection with inferior vena cava recon-
struction for retroperitoneal leiomyosarcoma. World Jour-
nal of Surgical Oncology, 7, 3.
doi:10.1186/1477-7819-7-3
[5] Kyriazi, M.A., Stafyla, V.K., Chatzinikolaou, I., Koureas,
Copyright © 2013 SciRes. Openly accessible at http://www.sc irp.or g/journal/crcm/