Immediate Total Elbow Arthroplasty Following Olecranon Osteotomy: A Case Report
Copyright © 2013 SciRes. OJO
214
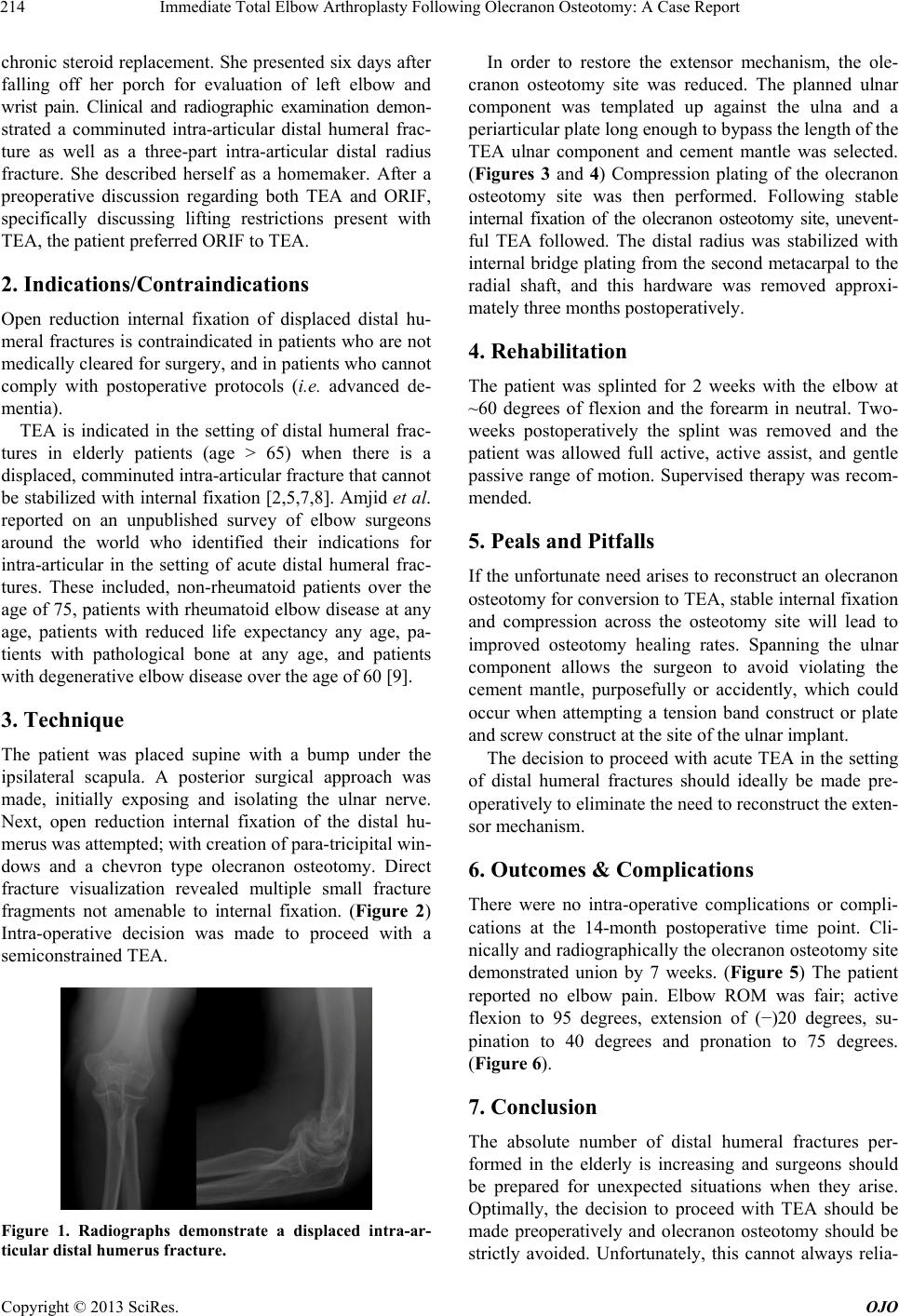
chronic steroid replacement. She presented six days after
falling off her porch for evaluation of left elbow and
wrist pain. Clinical and radiographic examination demon-
strated a comminuted intra-articular distal humeral frac-
ture as well as a three-part intra-articular distal radius
fracture. She described herself as a homemaker. After a
preoperative discussion regarding both TEA and ORIF,
specifically discussing lifting restrictions present with
TEA, the patient preferred ORIF to TEA.
2. Indications/Contraindications
Open reduction internal fixation of displaced distal hu-
meral fractures is contraindicated in patients who are not
medically cleared for surgery, and in patients who cannot
comply with postoperative protocols (i.e. advanced de-
mentia).
TEA is indicated in the setting of distal humeral frac-
tures in elderly patients (age > 65) when there is a
displaced, comminuted intra-articular fracture that cannot
be stabilized with internal fixation [2,5,7,8]. Amjid et al.
reported on an unpublished survey of elbow surgeons
around the world who identified their indications for
intra-articular in the setting of acute distal humeral frac-
tures. These included, non-rheumatoid patients over the
age of 75, patients with rheumatoid elbow disease at any
age, patients with reduced life expectancy any age, pa-
tients with pathological bone at any age, and patients
with degenerative elbow disease over the age of 60 [9].
3. Technique
The patient was placed supine with a bump under the
ipsilateral scapula. A posterior surgical approach was
made, initially exposing and isolating the ulnar nerve.
Next, open reduction internal fixation of the distal hu-
merus was attempted; with creation of para-tricipital win-
dows and a chevron type olecranon osteotomy. Direct
fracture visualization revealed multiple small fracture
fragments not amenable to internal fixation. (Figure 2)
Intra-operative decision was made to proceed with a
semiconstrained TEA.
Figure 1. Radiographs demonstrate a displaced intra-ar-
ticular distal humerus fracture.
In order to restore the extensor mechanism, the ole-
cranon osteotomy site was reduced. The planned ulnar
component was templated up against the ulna and a
periarticular plate long enough to bypass the length of the
TEA ulnar component and cement mantle was selected.
(Figures 3 and 4) Compression plating of the olecranon
osteotomy site was then performed. Following stable
internal fixation of the olecranon osteotomy site, unevent-
ful TEA followed. The distal radius was stabilized with
internal bridge plating from the second metacarpal to the
radial shaft, and this hardware was removed approxi-
mately three months postoperatively.
4. Rehabilitation
The patient was splinted for 2 weeks with the elbow at
~60 degrees of flexion and the forearm in neutral. Two-
weeks postoperatively the splint was removed and the
patient was allowed full active, active assist, and gentle
passive range of motion. Supervised therapy was recom-
mended.
5. Peals and Pitfalls
If the unfortunate need arises to reconstruct an olecranon
osteotomy for conversion to TEA, stable internal fixation
and compression across the osteotomy site will lead to
improved osteotomy healing rates. Spanning the ulnar
component allows the surgeon to avoid violating the
cement mantle, purposefully or accidently, which could
occur when attempting a tension band construct or plate
and screw construct at the site of the ulnar implant.
The decision to proceed with acute TEA in the setting
of distal humeral fractures should ideally be made pre-
operatively to eliminate the need to reconstruct the exten-
sor mechanism.
6. Outcomes & Complications
There were no intra-operative complications or compli-
cations at the 14-month postoperative time point. Cli-
nically and radiographically the olecranon osteotomy site
demonstrated union by 7 weeks. (Figure 5) The patient
reported no elbow pain. Elbow ROM was fair; active
flexion to 95 degrees, extension of (−)20 degrees, su-
pination to 40 degrees and pronation to 75 degrees.
(Figure 6).
7. Conclusion
The absolute number of distal humeral fractures per-
formed in the elderly is increasing and surgeons should
be prepared for unexpected situations when they arise.
Optimally, the decision to proceed with TEA should be
made preoperatively and olecranon osteotomy should be
strictly avoided. Unfortunately, this cannot always relia-