Open Journal of Ophthalmology, 2013, 3, 51-53
http://dx.doi.org/10.4236/ojoph.2013.33013 Published Online August 2013 (http://www.scirp.org/journal/ojoph) 51
MRI Findings in Post-Operative Bilateral Posterior
Ischemic Optic Neuropathy
Nirali P. Bhatt1*, Robert E. Morales2, Michaela K. Mathews1
1Department of Ophthalmology and Visual Sciences, University of Maryland School of Medicine, Baltimore, USA; 2Department of
Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, USA.
Email: *niralipbhatt@gmail.com
Received April 19th, 2013; revised May 20th, 2013; accepted June 15th, 2013
Copyright © 2013 Nirali P. Bhatt et al. This is an open access article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
A 62-year-old female complained of vision loss following multiple abdominal surgeries for mesenteric ischemia. The
patient’s visual acuity was no light perceptio n (NLP) in the right eye and hand motion (HM) at 1’ in the left eye. Both
pupils were unreactive and no relative afferent pupillary defect was noted. Anterior segment and fundus examination
were unremarkable. T1 and T2 weighted MRI imaging of the brain was normal but diffusion weighted imaging (DWI)
revealed areas of bright signal within both intraorbital optic nerves, confirming the diagnosis of posterior ischemic optic
neuropathy.
Keywords: Optic Nerve; Post-Operative Posterior Ischemic Optic Neuropathy; MRI; DWI
1. Case Report
A 62-year-old Hispanic female with a previou s history of
diabetes, hypertension, and glaucoma underwent re-
peated laparotomies and bowel resections for mesenteric
ischemia. During the procedures, several hypotensive
episodes were recorded. After the last surgery, the patien t
complained of having difficulty seeing objects in front of
her. The patient’s visual acuity was found to be reduced
to no light perception (NLP) in the right eye and hand
motion (HM) at 1’ in the left eye. Both pupils were un-
reactive to light. No relative afferent pupillary defect was
present. The patient had normal ocular motility and
alignment. Confrontational visual fields could not be
obtained reliably. Anterior segment examination showed
moderate cataracts in both eyes. Both optic nerves
showed a cup-to-disc ratio of 0.4, without pallor or
edema. The retina, macula, periphery and retinal vessels
were unremarkable. Histopathology of the surgical
specimen as well as laboratory studies revealed no evi-
dence of vasculitis. The patient underwent MRI and
magnetic resonan ce angiography ( MRA) of the brain. No
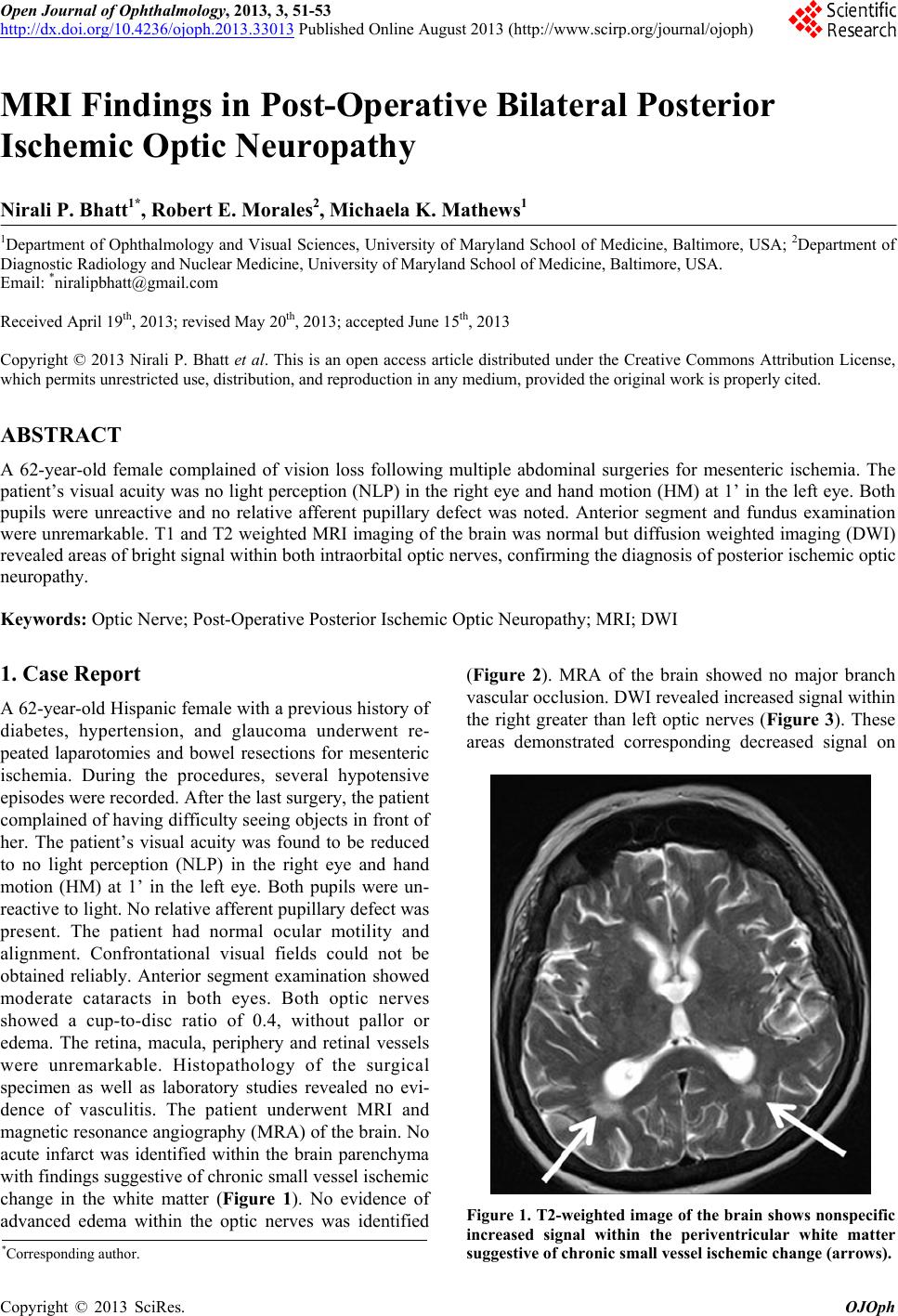
acute infarct was identified within the brain parenchyma
with findings suggestive of chronic small vessel ischemic
change in the white matter (Figure 1). No evidence of
advanced edema within the optic nerves was identified
(Figure 2). MRA of the brain showed no major branch
vascular occlusion. DWI revealed increased signal within
the right greater than left optic nerves (Figure 3). These
areas demonstrated corresponding decreased signal on
Figure 1. T2-weighted image of the brain shows nonspecific
increased signal within the periventricular white matter
suggestive of chronic small vessel ischemic change (arrows).
*Corresponding a uthor.
Copyright © 2013 SciRes. OJOph