J. M. LADOWSKI ET AL. 117
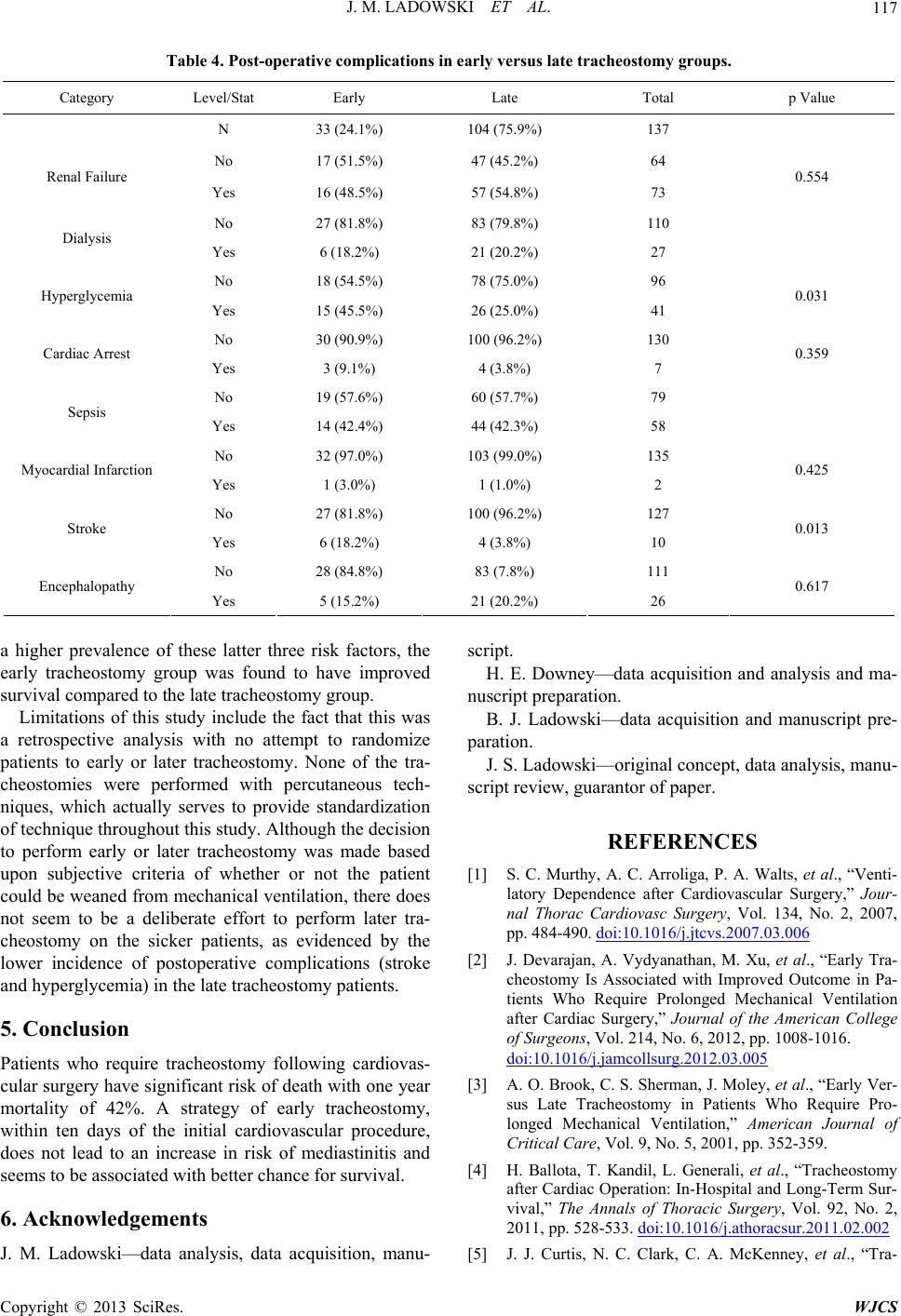
Table st-operatitions inus late tracheostomy groups.
Category p Value
4. Pove complica earl y ve r s
Level/Stat Early Late Total
N 33) 104%) (24.1% (75.9137
No 17 (51.5%) 47 (45.2%) 64
Renal Failure 0.554
Dialysis
Hyperglycemia 0.031
Cardiac Arrest 0.359
1 6
Sepsis
Myocardial Infarction 0.425
21 127
Stroke 0.013
Encephalopathy 0.617
Yes 16 (48.5%) 57 (54.8%) 73
No 27 (81.8%) 83 (79.8%) 110
Yes 6 (18.2%) 21 (20.2%) 27
No 18 (54.5%) 78 (75.0%) 96
Yes 15 (45.5%) 26 (25.0%) 41
No 30 (90.9%) 100 (96.2%) 130
Yes 3 (9.1%) 4 (3.8%) 7
No 9 (57.6%) 0 (57.7%) 79
Yes 14 (42.4%) 44 (42.3%) 58
No 32 (97.0%) 103 (99.0%) 135
Yes 1 (3.0%) 1 (1.0%) 2
No 7 (81.8%) 00 (96.2%)
Yes 6 (18.2%) 4 (3.8%) 10
No 28 (84.8%) 83 (7.8%) 111
Yes 5 (15.2%) 21 (20.2%) 26
a higher prevalence of these latter three risk factors, the
ire tracheostomy following cardiovas-
sis, data acquisition, manu-
script.
ES
[1] S. C. Murthy, A. C. Arroliga, P. A. Walts, et al., “Venti-
latory Dependar Surgery,” Jour-
early tracheostomy group was found to have improved
survival compared to the late tracheostomy group.
Limitations of this study include the fact that this was
a retrospective analysis with no attempt to randomize
patients to early or later tracheostomy. None of the tra-
cheostomies were performed with percutaneous tech-
niques, which actually serves to provide standardization
of technique throughout this study. Although the decision
to perform early or later tracheostomy was made based
upon subjective criteria of whether or not the patient
could be weaned from mechanical ventilation, there does
not seem to be a deliberate effort to perform later tra-
cheostomy on the sicker patients, as evidenced by the
lower incidence of postoperative complications (stroke
and hyperglycemia) in the late tracheostomy patients.
5. Conclusion
Patients who requ
cular surgery have significant risk of death with one year
mortality of 42%. A strategy of early tracheostomy,
within ten days of the initial cardiovascular procedure,
does not lead to an increase in risk of mediastinitis and
seems to be associated with better chance for survival.
6. Acknowledgements
J. M. Ladowski—data analy
H. E. Downey—data acquisition and analysis and ma-
nuscript preparation.
B. J. Ladowski—data acquisition and manuscript pre-
paration.
J. S. Ladowski—original concept, data analysis, manu-
script review, guarantor of paper.
REFERENC
ence after Cardiovascul
nal Thorac Cardiovasc Surgery, Vol. 134, No. 2, 2007,
pp. 484-490. doi:10.1016/j.jtcvs.2007.03.006
[2] J. Devarajan, A. Vydyanathan, M. Xu, et al., “Early Tra-
cheostomy Is Associated with Improved Outcome in Pa-
tients Who Require Prolonged Mechanical Ventilation
after Cardiac Surgery,” Journal of the American College
of Surgeons, Vol. 214, No. 6, 2012, pp. 1008-1016.
doi:10.1016/j.jamcollsurg.2012.03.005
[3] A. O. Brook, C. S. Sherman, J. Moley, et al., “Early Ver-
sus Late Tracheostomy in Patients Who Require Pro-
longed Mechanical Ventilation,” American Journal of
Critical Care, Vol. 9, No. 5, 2001, pp. 352-359.
[4] H. Ballota, T. Kandil, L. Generali, et al., “Tracheostomy
after Cardiac Operation: In-Hospital and Long-Term Sur-
vival,” The Annals of Thoracic Surgery, Vol. 92, No. 2,
2011, pp. 528-533. doi:10.1016/j.athoracsur.2011.02.002
[5] J. J. Curtis, N. C. Clark, C. A. McKenney, et al., “Tra-
Copyright © 2013 SciRes. WJCS