Health
Vol.4 No.12A(2012), Article ID:26061,9 pages DOI:10.4236/health.2012.412A202
Dietary fat intake of Japanese male children and its associated factors: Results of the 1995 National Nutrition Survey in Japan
![]()
1Faculty of Health and Nutrition, Yamanashi Gakuin University, Yamanashi, Japan
2Department of Health Sciences, Interdisciplinary Graduate School of Medicine and Engineering, University of Yamanashi, Yamanashi, Japan; #Corresponding Author: zenymgt@yamanashi.ac.jp
3Department of International Medical Cooperation, National Center for Global Health and Medicine, Tokyo, Japan
4Department of Health Economics and Epidemiology Research, University of Tokyo School of Public Health, Tokyo, Japan
5Faculty of Health and Nutrition, Bunkyo University, Kanagawa, Japan
6Takao-Hospital, Kyoto, Japan
7The First Institute for Health Promotion and Health Care, Japan Anti-Tuberculosis Association [JATA], Tokyo, Japan
8Department of Public Health, Jichi Medical University, Tochigi, Japan
Received 5 October 2012; revised 10 November 2012; accepted 16 November 2012
Keywords: Childhood obesity; Dietary fat intake; National Nutrition Survey; Comprehensive Survey of Living Conditions of the People on Health and Welfare
ABSTRACT
Aim: To clarify the factors associated with reported dietary fat intake by Japanese male children. Methods: This study is based on the data of a nationally representative cross-sectional study in Japan. Three hundred and seventy-seven male children (age, 6 - 11 years) whose households were sampled in the 1995 Comprehensive Survey of Living Conditions of the People on Health and Welfare, and the 1995 National Nutrition Survey and whose parents were identified through record linkage between the 2 survey data sets were enrolled. Results: The final dataset in this study consisted of 377 boys with 329 of their parents. Fifty-two boys were found to be overweight (13.8%). The reported dietary fat intake was higher among the overweight boys than among the non-overweight boys. Maternal obesity was significantly associated with obesity in male children. Boys who frequently consumed foods from the “fats and lipids” group and the “meat” groups, and children from nuclear families rather than 3- generation families reported high dietary fat intake. In addition, parental fat intake was also significantly associated with fat intake of male children. Conclusions: Child and parental dietary habits along with the household status should be considered when implementing nutritional education programmes to control dietary fat intake and reduce the obesity risks of male children.
1. INTRODUCTION
In industrialized countries, overweight and obesity are the most common nutritional disorders [1-3]. Overweight children have a high risk of being overweight in adulthood [4,5], and experience typical obesity-related morbidity, including coronary heart disease, high blood pressure, and adult-onset type 2 diabetes [6]. Moreover, previous studies have demonstrated that childhood obesity, in combination with other lifestyle risk factors, contributes to the development of arteriosclerotic lesions even during childhood [7], and that some obese children develop metabolic syndrome early in life [8].
Although the prevalence of obesity in Japanese adults has been quite low compared with other nations [9,10], the prevalence of overweight and obesity has steadily increased among individuals of both sexes under the age of 50. This indicates the necessity of addressing obesity and overweight in Japan [11]. In addition, Matsushita and co-workers have clearly shown increasing trends in the prevalence of obesity among Japanese children [12]. The prevalence of childhood obesity had been steadily increasing since the 1980s into the early 2000s and the prevalence of obesity in late infancy also had been increasing during this period [13]. Moreover, the prevalence of obesity in male children was found to be higher than in female children. While the prevalence in boys in 2007 was approximately twice (9% - 10%) that of the reference data in 1979-1981, for each age group, the prevalence in girls was less than that of boys, at approximately 8%. Consequently, it is expected to be important to analysis the data related to childhood obesity which was obtained in the 1990s because the analysis could contribute to the establishment of prevention programs to counter childhood obesity or overweight.
Many studies have identified certain risk factors for childhood obesity including eating behaviour and physical activity of children [14]. Regarding dietary habits, previous research has revealed a significant association between dietary fat intake and obesity both in children and in adult populations [15,16]. This suggests a need to control dietary fat intake for preventing and treating obesity. Of note, previous studies have demonstrated that children of obese parents show a strong preference towards a high-fat diet and have higher dietary fat intake [17,18]. Maternal dietary fat intake was also found to have a strong influence on the dietary fat intake of their children [15].
In Japan, although appropriate fat intake (expressed as a percentage relative to the total energy) for individuals aged 6 - 11 years is estimated to be 25% - 30% [19], a recent National Health and Nutrition Survey (NHNS) clarified that the dietary fat intake of children in Japan has not improved significantly because the percentages of fat intake in 2003 and 2008 were found to be 29.0% and 28.3%, respectively [20,21]. The association between dietary fat intake and childhood obesity has not been examined in a Japanese population.
Importantly, there are two difficulties to be considered during the analysis of the National Nutrition Survey (NNS) data among female children. Firstly, girls often exhibit secondary sexual characteristics at an earlier age than boys, so the proportion of girls with such characteristics among the sample population could be higher than that of boys. Hormonal changes associated with this are therefore more likely to affect the girls’ weight status. This introduces a confounding factor that negates the association between dietary fat intake and obesity among girls. Secondly, as suggested in previous studies, girls often begin dieting at an earlier age than boys [22], and dietary interventions to moderate fat intake are implemented even in children in some cases [23]. Also of note, it must be considered that, in Japan, there might be a similar trend exhibited by the studies described above because the total energy intake and intake of protein and fat were found to be similar for subjects 1 - 6 years of age. The total energy intake and intake of protein and fat for boys was found to be higher than in girls after 7 years of age in 2004 [24]. Hence, for the present study, it was decided to include only male children and their parents.
Our research objective was to examine the relationship between dietary fat intake and childhood obesity in male Japanese children. Therefore, we aimed to confirm this association using data from the NNS in Japan. Another objective was to examine the association between child dietary fat intake and determine whether such intake is associated with food group intake, dietary habits, and household status of these individuals.
2. METHODS
The Japanese Government conducts a Comprehensive Survey of the Living Conditions of People on Health and Welfare (CSLCPHW) and a NNS among randomly sampled districts in 3-year intervals and annually, respectively [25,26]. Both surveys include sections on health and socio-economic status (SES). Trained interviewers visit the respondents’ homes. Our study population included the respondents of both surveys, which were conducted in 1995. The 1995 CSLCPHW was administered to 5100 randomly sampled districts nationwide, with a household response rate of 91.0%. The 1995 NNS was carried out independently in 300 districts randomly sampled from the same districts in which the CSLCPHW was conducted. The estimated response rate to the NNS was 94.9%. The Japanese government granted permission to use the data from both surveys. These data were linked at the level of individual respondents because a common unique identifier was used in both surveys. The final number in the linked data set was 13,270. This number was reduced as a result of non-responsive subjects or relocation of correspondents during the 5-month interval between the surveys. Among the NNS participants, 93.2% was linked to their CSLCPHW data [26].
Data on the following survey items were extracted from the 1995 CSLCPHW data: relationship, sex, marital status, and occupation-related information from the household questionnaire; and physical health problems affecting daily life, symptoms or medical conditions, mental health status, health check attendance, lifestyle habits (smoking, drinking, and exercise), daily health habits, family structure, and occupational status from the health questionnaire.
In addition, the following information was collected from the 1995 NNS data: height, weight, and lifestyle habits (smoking, drinking and exercise) from the physical status questionnaire; the frequencies of eating out and skipping meals from the dietary habit questionnaire; and food and nutrient intakes from the dietary intake questionnaire. In the NNS, medical doctors, registered dietitians, and public health nurses measured the height and weight of the participants.
“Dietary Records” were used to collect information about the household meals only on a certain day excluding Sunday or Public Holiday during the survey period. Then, registered dieticians calculated the total household intake from this information. Each individual intake was calculated using each percentage of the household intake [25]. For instance, when the dietician calculated the total calorie content intake of the family as 8000 kcal from the data of dietary records and the percentage of child, mother, and father were reported as 25%, 35%, and 40% in the questionnaire, respectively, the individual calorie intakes of the child, mother, and father were determined as 2000 kcal, 2800 kcal, and 3200 kcal, respectively.
To clarify the Association of the children’s reported dietary fat intake and parental obesity with childhood overweight, childhood overweight was defined according to the body mass index (BMI) such that 85th percentile for age and sex, and the children were classified as overweight (BMI ≥ 85th percentile) and non-overweight (BMI < 85th percentile) groups. The cut-off values were based on the definition provided by the US Center for Disease Control and Prevention (CDC) [27]. The children’s dietary fat intake was assessed according to the Japanese Recommended Dietary Allowance [19], in which appropriate fat intake 8expressed as a percentage relative to the total energy) for individuals aged 6 - 11 years is estimated to be 25% - 30%. By using the maximum recommended fat intake of 30% as the cut-off value, the children were divided into excessive (≥30%) and moderate (<30%) fat intake groups, and the association between the dietary fat intake and overweight was examined using multivariable logistic analysis to adjust for the effect of the age of the participants. The association between overweight among the children and their parents was also determined by multivariable logistic analysis to control for the effect of the age of the participants. The parents were divided into two groups according to their BMI: obesity group (BMI ≥ 25 kg/m2) and non-obesity group (BMI < 25 kg/m2).
We then aimed to determine factors associated with the reported dietary fat intake of the male children. Further analyses were performed for the boys as well as for their fathers and mothers with the aim of determining the associations between the reported dietary fat intake of the children and the following variables: 1) the child’s age-adjusted food group intake calculated for each of the 14 food groups, determined by the dietician from the data of the “Dietary Records”; 2) the dietary habit variables including frequencies of eating out and skipping meals; 3) the physical health variables including physical health problems affecting daily life and symptoms or medical conditions; 4) the variables indicating household status including family structure and parental occupational status; and 5) the parental dietary fat intake. The association of the food group intake of the children with their reported dietary fat intake was determined by covariance analysis to allow for the effect of their age and those of the other variables were assessed using logistic analysis.
All statistical analyses were performed with SAS statistical software version 9.2 (SAS Institute Inc., Cary, NC).
3. ETHICS APPROVAL
This study was based on the National Nutrition Survey and the Comprehensive Survey of the Living Conditions of People on Health and Welfare data which were crosssectional and collected by Japanese Government. Informed consent was obtained by each participant of the national survey and all approvals for using the data were obtained by the Ministry of Health, Labour and Welfare (Former Ministry of Health and Welfare). In addition, this study was conducted in accordance with the Guidelines Concerning Epidemiological Research (the Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health, Labour and Welfare, Japan).
4. RESULTS
From a total of 999 households, 283 households were excluded because of missing data on the height and weight of the child, mother, or father. Taken together, the final data set included 716 male and female children aged 6 - 11 years from 716 households. Of these, 377 boys and 325 of their parents were included in this study.
Table 1 shows the height and weight data of the children. The values were within the average range for the population estimated in the 1995 nationwide statistics on the physical development of schoolchildren. The numbers of overweight children were 56 boys (14.9%).
The subjects were divided into two groups according to fat intake: excessive (>=30%) and moderate (<30%) (n = 183 and 194, respectively) (Table 2). The overweight boys had an increased dietary fat intake relative to their non-overweight counterparts, with an odds ratio (OR) of 1.95 (95% confidence interval (CI) = 1.09 - 3.49) (Table 2). The OR for concordance of overweight between father and child was 1.04 (95% CI = 0.54 - 2.01) and that between mother and son was 3.1 (95% CI = 1.52 - 6.35; Table 3).
As shown in Table 4, male children with increased reported dietary fat intake consumed a greater amount of foods in the “potatoes and taro”, “fats and oils”, “meat”, and “milk and dairy products” groups, along with lower consumption of foods in the “rice and grain”, and “fish and seafood” groups. Children in the high-fat intake group were more likely to skip breakfast than those in the low-

Table 1. The height, weight and body mass index (BMI) of the participating male children and the number.
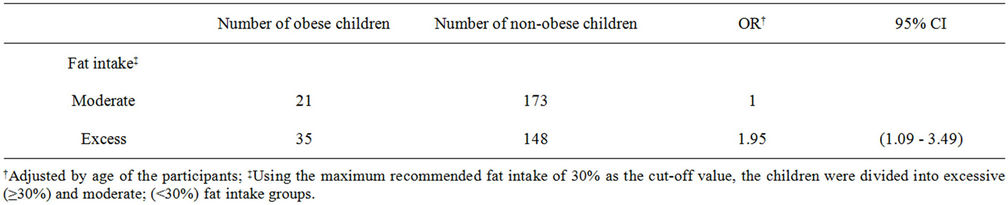
Table 2. Adjusted odds ratio (OR) and 95% confidence interval (CI) of excess reported fat intake for childhood obesity in males by using logistic multivariable regression analysis.
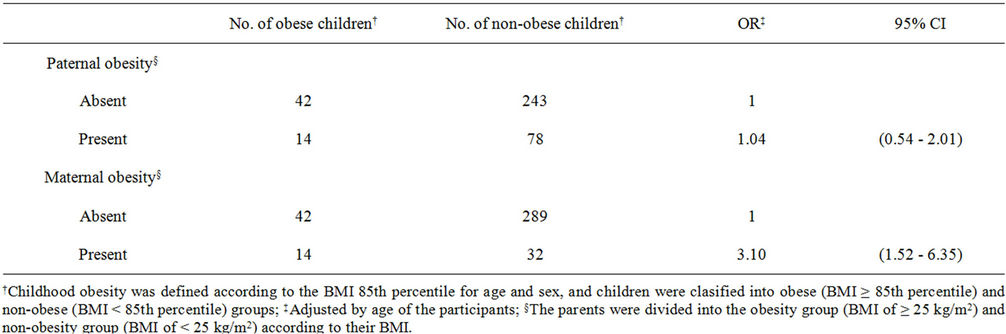
Table 3. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) of both paternal and maternal obesity for childhood obesity in male by using logistic multivariable regression analyses.
fat intake group (Table 5). No significant association was noted between the children’s reported dietary fat intake and any of the physical health variables, but an association was observed with respect to a household variable (family structure). Children in nuclear families had higher dietary fat intake than those in 3-generation families, with an OR of 2.61 (95% CI = 1.17 - 5.82). The other household status variable, parental occupational status, did not affect the children’s dietary fat intake. As for parental dietary fat intake, the parents who consumed a greater amount of dietary fat were likely to have children with high fat intake, with an OR of 2.52 (95% CI = 1.65 - 3.84) for fathers and 3.56 (95% CI = 2.25 - 5.63) for mothers (Table 5).
5. DISCUSSION
Regarding the prevention of childhood obesity, the association between dietary fat intake and childhood overweight should be examined in the Japanese population as such an association has been observed in other countries. This study is the first to clarify this association in Japanese male children. In addition, we have demon-

Table 4. Comparison between the highand low-fat reported intake groups with regard to the mean reported intake of each food group of the participants after controlling for their age.
strated the associations between reported dietary fat intake and food intake patterns, dietary habits, and family structure [nuclear family or extended family] for Japanese children.
Our results demonstrate that overweight male children have higher dietary fat intake than male children withnormal weight. This is consistent with the previous observations regarding a positive association between dietary fat intake and obesity [15].
Having an obese mother but not an obese father was found to be significantly associated with an increased OR for overweight in children although previous research has indicated that obesity in both fathers and mothers is associated with increased risk of obesity in their offspring [28]. The link between child and maternal nutrient intake has been previously demonstrated to be stronger than that between child and paternal nutrient intake [29]. This is likely to be due to the potential impact of the mother’s eating habits on her children as children of obese mothers also tend to consume a larger amount of fat [17,18]. Moreover, Whitaker et al. reported that maternal obesity tracks childhood obesity more strongly than paternal obesity [30].
We also analysed the factors involved in reported dietary fat intake and found that higher dietary fat intake is linked to increased intake of foods from the “fats and oils” group and the “meat” groups by children. This is consistent with the results obtained from a previous US study [31]. Foods in these groups contain abundant fats and thereby contribute to high fat intake as observed in our sample population.
As for the dietary habit variables, skipping breakfast tended to be associated with increased fat intake by children. This is probably due to an uneven distribution of energy intake throughout the day that often leads to increased consumption of energy-laden, high-fat foods in the afternoon and evening. Our results confirm the marked influence of dietary habits on dietary fat intake.
This study has some advantages. A nationally representative dietary survey clarifying the dietary patterns of British children was recently conducted in Great Britain [32]. However, the analyses of this survey did not include parents. We analysed the nutritional data of both children and their parents and we believe that this is one of the strengths of our study. The present analyses were based on the data sets obtained from two nationwide

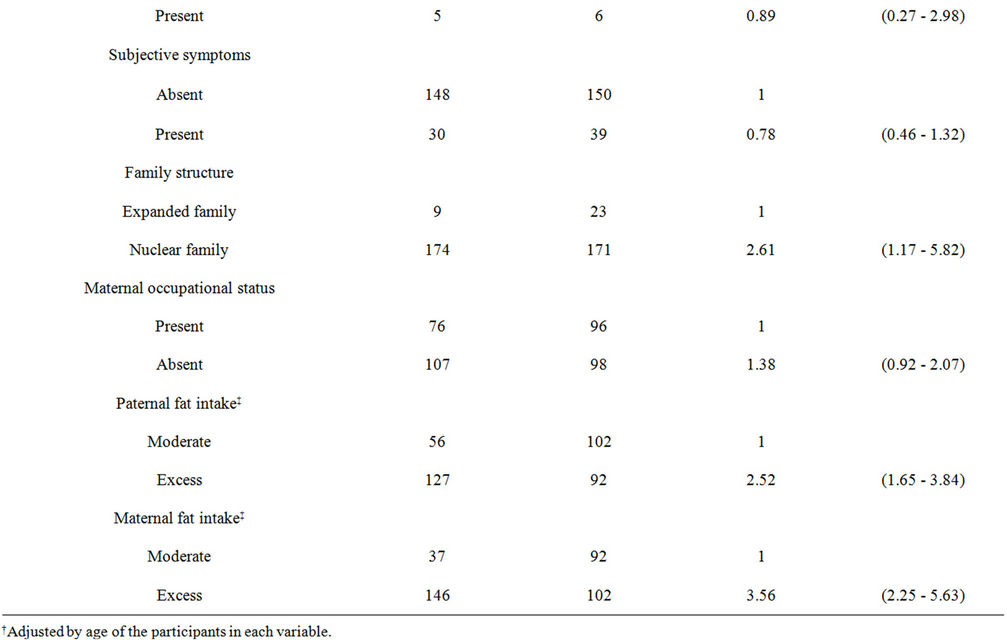
Table 5. Adjusted odds ratio (OR) and 95% confidence interval (CI) of dietary habits, health status, lifestyle factor and parental fat intake by using logistic multivariable regression analysis to control for the effect of the participants’ age.
health surveys, the CSLCPHW and the NNS, conducted under the authority of the Statistics Act of Japan. In the CSLCPHW, participating households were randomly selected from census blocks [33], and those in the NNS were randomly chosen from the census blocks sampled for the CSLCPHW [34], to provide nationally representative samples of households and individuals that were sufficient to ensure the external validity of the survey results. Furthermore, the study items used in the surveys were thoroughly revised for increased reliability.
Moreover, since 1995, the NNS has collected data regarding food and nutrient intake on an individual basis rather than the conventional household basis, thus enabling the analysis of individual dietary intake, which was not possible before 1995. In this study, the 2 data sets from the CSLCPHW and the NNS were matched through a record linkage system and analysed at the individual level, which is the major strength of the present research. This study provides an analysis of the first record linkage study using nationwide data that specifically targeted children.
However, this study also has some limitations. First, the causality between the children’s dietary fat intake and each of the associated factors could not be established due to the cross-sectional study design. Second, as the 2 nationwide surveys covered all age groups and did not specifically focus on children, the survey data provided insufficient information on the children’s lifestyle habits to assess the association of dietary fat intake with their daily activities, physical condition, and exercise habits. Given that physical activities and exercise reduce obesity risks [35], the physical activity variables may have a significant impact on the children’s dietary fat intake. In addition, it was impossible to survey directly the nutrition intake of children because we were able to use only the data that was calculated by using the amount of household intake and the percentage of each family member. However, our data are sufficient to be considered valid because the results are highly similar to other results obtained in a survey using the direct survey method in Japan [36].
Additionally, the sample size is not large enough to detect precise factors associated with the reported male children’s dietary fat intake. Although the statistical power is relatively low, there were some factors that were found to be associated with excess dietary fat intake in male children. It is suggested that addressing these factors may be useful for improving childhood dietary fat intake when intervention is considered. Finally, it was impossible to examine the effect of each variable which might be related to excess fat intake because it was difficult to create a multivariate model due to the small sample size.
Despite these limitations, our analyses will provide a useful basis for implementing comprehensive lifestyle intervention strategies to prevent and treat childhood overweight on a whole-family basis.
In conclusion, we have clarified the association between reported dietary fat intake of Japanese male children and childhood overweight. Moreover, we have clarified the associations between the children’s dietary fat intake and their food intake patterns, dietary habits and family structure. These results indicate that both child and parental dietary habits along with the household status should be considered when implementing nutritional education programmes to control dietary fat intake and reduce obesity risks for children.
6. ACKNOWLEDGEMENTS
This study was supported by Grant No. H11-Toukei-002 (Principal investigator of the national research group: Prof. Hiroshi Yanagawa) from the Ministry of Health, Labour and Welfare, Japan.
REFERENCES
- Ogden, C.L., Troiano, R.P., Briefel, R.R., Kuczmarski, R.J., Flegal, K.M. and Johnson, C.L. (1997) Prevalence of overweight among preschool children in the United States, 1971 through 1994. Pediatrics, 99, E1. doi:10.1542/peds.99.4.e1
- Bundred, P., Kitchiner, D. and Buchan, I. (2001) Prevalence of overweight and obese children between 1989 and 1998: population based series of cross sectional studies. BMJ, 322, 326-328. doi:10.1136/bmj.322.7282.326
- Kalies, H., Lenz, J. and von Kries, R. (2002) Prevalence of overweight and obesity and trends in body mass index in German pre-school children, 1982-1997. International Journal of Obesity and Related Metabolic Disorders, 26, 1211-1217. doi:10.1038/sj.ijo.0802013
- Abraham, S., Collins, G. and Nordsieck, M. (1971) Relationship of childhood weight status to morbidity in adults. HSMHA Health Reports, 86, 273-284. doi:10.2307/4594149
- Charney, E., Goodman, H.C., McBride, M., Lyon, B. and Pratt, R. (1976) Childhood antecedents of adults obesity. Do chubby infants become obese adults? New England Journal of Medicine, 95, 6-9. doi:10.1056/NEJM197607012950102
- Dietz, W.H. (1998) Childhood weight affects adult morbidity and mortality. Journal of Nutrition, 128, 411S- 414S.
- Berenson, G.S., Srinivasan, S.R., Bao, W., Newman III, W.P., Tracy, R.E. and Wattigney, W.A. (1998) Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. New England Journal of Medicine, 338, 1650-1656. doi:10.1056/NEJM199806043382302
- Cook, S., Weitzman, M., Auinger, P., Nguyen, M. and Dietz, W.H. (2003) Prevalence of metabolic syndrome phenotype in adolescents. Archives of Pediatrics & Adolescent Medicine, 157, 821-827. doi:10.1001/archpedi.157.8.821
- World Health Organization. (1998) A world health organization consultation on obesity—Preventing and managing the global epidemic. WHO, Geneva.
- Popkin, B.M. and Doak, C.M. (1998) The obesity epidemic is a worldwide phenomenon. Nutrition Reviews, 56, 106-114. doi:10.1111/j.1753-4887.1998.tb01722.x
- Matsushita, Y., Takahashi, Y., Mizoue, T., Inoue, M., Noda, M., Tsugane, S. and JPHC Study Group (2008) Overweight and obesity trends among Japanese adults: A 10-year follow-up of the JPHC Study. International Journal of Obesity, 32, 1861-1867. doi:10.1038/ijo.2008.188
- Matsushita, Y., Yoshiike, N., Kaneda, F., Yoshita, K. and Takimoto, H. (2004) Trends in childhood obesity in Japan over the last 25 years from the national nutrition survey. Obesity Research, 12, 205-214. doi:10.1038/oby.2004.27
- Yoshinaga, M., Ichiki, T., Tanaka, Y., et al. (2010) Prevalence of childhood obesity from 1978 to 2007 in Japan. Pediatrics International, 52, 213-217. doi:10.1111/j.1442-200X.2009.02930.x
- Agras, W.S. and Mascola, A.J. (2005) Risk factors for childhood overweight. Current Opinion in Pediatrics, 17, 648-652. doi:10.1097/01.mop.0000172818.87261.ab
- Nguyen, V.T., Larson, D.E., Johnson, R.K. and Goran M.I. (1996) Fat intake and adiposity in children of lean and obese parents. American Journal of Clinical Nutrition, 63, 507-513.
- Tucker, L.A., Seljaas, G.T. and Hager, R.L. (1997) Body fat percentage of children varies according to their diet composition. Journal of the Academy of Nutrition and Dietetics, 97, 981-986.
- Eck, L.H., Klesges, R.C., Hanson, C.L. and Slawson, D. (1992) Children at familial risk for obesity: An examination of dietary intake, physical activity and weight states. International Journal of Obesity, 16, 71-78.
- Fisher, J.O. and Birch, L.L. (1995) Fat preferences and consumption of 3- to 5-year-old children are related to parental adiposity. Journal of the American Dietetic Association, 95, 759-764. doi:10.1016/S0002-8223(95)00212-X
- Fisher, J.O. and Birch, L.L. (1995) Fat preferences and consumption of 3- to 5-year-old children are related to parental adiposity. Journal of the American Dietetic Association, 95, 759-764. doi:10.1016/S0002-8223(95)00212-X
- Ministry of Health, Labour and Welfare, Japan (2003) The National Health and Nutrition Survey in Japan. http://www.maff.go.jp/j/balance_guide/b_food/4/pdf/sankouhaifu.pdf [in Japanese] Accessed May 25, 2012.
- Ministry of Health, Labour and Welfare, Japan (2008) The National Health and Nutrition Survey in Japan. http://www.mhlw.go.jp/houdou/2009/11/dl/h1109-1b.pdf [in Japanese] Accessed May 25, 2012.
- Robert, S.J., McGuiness, P.J., Bilton, R.F. and Maxwell, S.M. (1999) Dieting behavior among 11- to 15-year-old girls in Merseyside and Northwest of England. Journal of Adolescent Health, 25, 62-67. doi:10.1016/S1054-139X(98)00129-3
- Van Horn, L., Obarzanek, E., Friedman, L.A., Gernhofer, N. and Barton, B. (2005) Children’s adaptations to a fatreduced diet: The Dietary Intervention Study in Children (DISC). Pediatrics, 115, 1723-1733. doi:10.1542/peds.2004-2392
- National Health and Nutrition Survey in Japan (2008) Nutrition and eating habits. In: Yanagisawa, M., Ed., Almanac of Data on Japanese Children from 2006-2008, Chuoh Publishing, Tokyo, 157-169.
- Ministry of Health, Labour and Welfare, Japan, Health Service Bureau (1995) The 1995 National Nutrition Survey (NNS).
- Ministry of Health, Labour and Welfare, Japan, Statistics and Information Department (1995) The 1995 Comprehensive Survey of the Living Conditions of People on Health and Welfare (CSLCPHW).
- Kuczmarski, R.J., Ogden, C.L., Grummer-Strawn, L.M., et al. (2000) CDC growth charts: United States. Advanced Data, 8, 1-27.
- Duran-Tauleria, E., Rona, R.J. and Chinn, S. (1995) Factors associated with weight for height and skinfold thickness in British children. Journal of Epidemiology & Community Health, 49, 466-473. doi:10.1136/jech.49.5.466
- Oliveria, S.A., Ellison, R.C., Moore, L.L., Gillman, M.W., Garrahie, E.J. and Singer, M.R. (1992) Parent-child relationship in nutrient intake: The Framingham Children’s Study. American Journal of Clinical Nutrition, 56, 593- 598.
- Whitaker, K.L., Jarvis, M.J., Beeken, R.J., Boniface, D. and Wardle J. (2010) Comparing maternal and paternal intergenerational transmission of obesity risk in a large population-based sample. American Journal of Clinical Nutrition, 91, 1560-1567. doi:10.3945/ajcn.2009.28838
- Subar, A.F., Ziegler, R.G., Patterson, B.H., Ursin, G. and Graubard, B. (1994) US dietary patterns associated with fat intake: The 1987 National Health Interview Survey. American Journal of Public Health, 84, 359-366. doi:10.2105/AJPH.84.3.359
- Pryer, J.A. and Rogers, S. (2009) Dietary patterns among a national sample of British children aged 1 1/2-4 1/2 years. Public Health Nutrition, 12, 957-966. doi:10.1017/S1368980008003364
- Ministry Health and Welfare (1997) Comprehensive Survey of the Living Conditions of People on Health and Welfare in 1995. Ministry Health and Welfare, Tokyo.
- Ministry Health and Welfare (1997) Status of national nutrition: Results of the national survey in 1995. Ministry Health and Welfare, Tokyo.
- Carrel, A.L., Clark, R.R., Peterson, S.E., Nemeth, B.A., Sullivan, J. and Allen, D.B. (2005) Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: A randomized, control study. Archives of Pediatrics & Adolescent Medicine, 159, 963-968. doi:10.1001/archpedi.159.10.963
- Nagai, J., Yoshimoto, S., Matsuura, T. and Katsuno, S. (2006) A community-based study on dietary intake among school-age children: Goshiki Health Study— Trend in dietary intake of the fifth grade school children over 13 years (1986-1999) in Goshiki Town of Hyogo Prefecture Jpn. School Health, 48, 3-17.
NOTES
*Denotes equal contribution/co-first author.

