Open Journal of Urology
Vol. 2 No. 1 (2012) , Article ID: 17791 , 5 pages DOI:10.4236/oju.2012.21003
Urodynamic Findings in Young Women of Less Than Forty Years Old with Lower Urinary Tract Symptoms*
Urology and Nephrology Research Center (UNRC), Shohada Medical Center, Shahid Beheshti University, Tehran, Iran
Email: karami_hosein@yahoo.com
Received November 24, 2011; revised January 15, 2012; accepted January 25, 2012
Keywords: Urge Incontinence; Women; Urodynamics
ABSTRACT
Purpose: The aim of the study was to determine urodynamic findings in young women (<40 years old) with bothersome lower urinary tract symptoms. Materials and Methods: The records of 315 women were reviewed during 2002 to 2010. Those with neurological disease, history of urogenital malignancies, urethral stricture or trauma, acute UTI, unsterile urine analysis, congenital urological disease, pelvic organ prolapse, diabetes mellitus or a primary complaint of stress incontinence were excluded. All completed the American Urological Association Symptom Index (AUASI) and underwent urodynamic studies. Results: Bladder dysfunction was diagnosed in 78.4% of the patients with urge incontinence. Bladder and voiding phase dysfunction were found in 134 (42.5%) and 110 (34.9%) of patients, respectively. Occult neurological disease was later diagnosed in 10 women (3.17%) with urge incontinence and bladder dysfunction. Discussion: Urge incontinence and voiding symptoms are frequently associated with urodynamical abnormalities. Urge incontinence and bladder dysfunction may be a sign of occult neurological disease in this population. The presenting symptoms are useful in determining the advantage of urodynamic study in this population.
1. Introduction
Young women with LUTS are a difficult group of patients to diagnose and treat. Irritative symptoms (frequency, nocturia, urgency, incontinence) and obstructive symptoms (straining, weak stream, intermittency, and hesitancy) have different etiologies in this group. Pregnancy and delivery can initiate the changes that cause LUTS in this population. The prevalence of LUTS in the young women has not been extensively studied yet. Previous studies have paid attention on the prevalence of stress incontinence [1]. The symptom of urge incontinence has not been investigated extensively, unless in studies that the prevalence of incontinence is explained [2-5]. The association of LUTS with urodynamic abnormalities in young women has not been studied before. In this study, we intended to determine urodynamic findings in this group. This information could be useful in selecting patients for urodynamic evaluation.
2. Materials and Methods
The records of 315 young (<40 years) women who underwent urodynamic assessment for LUTS during 2002 to 2010 were reviewed. Those with neurologic diseasehistory of previous incontinence or lower urinary tract reconstructive surgery, and those with urogenital malignancies, urethral stricture or trauma, acute UTI, unsterile urine analysis, congenital urological disease, pelvic organ prolapse, diabetes mellitus or a primary complaint of stress incontinence according to history and/or physical examination were excluded. All patients provided complete urological and gynecological history and underwent complete physical examination. All women completed the American Urological Association Symptom Index (AUASI) before testing [6]. The index was divided into 3 groups:
1) Total score;
2) Obstructive score;
3) Irritative score.
Urodynamic tests were completed in all patients. Methods, units and definitions, conformed to the standards suggested by the International Continence Society [7]. EMG was taken by surface electrodes. Filling cystometery was performed too. The existence of involuntary detrusor contractions or detrusor overactivity (DO), impaired compliance, and sensory urgency during filling were noted. Impaired compliance was defined as <12.5 ml/cm H2O [8]. Impaired contractility was defined as a detrusor contraction of <20 cm H2O, with a flow of <12 ml/s [9,10]. Patients voided in the seating position that detrusor pressure, flow rate, EMG activity, and post void residual were evaluated. Bladder dysfunction was defined as DO and/or impaired compliance. Voiding phase dysfunction was defined as bladder outlet obstruction or impaired contractility. The diagnosis of dysfunctional voiding was proposed when external sphincter activity was increasing during voluntary voiding with accompanying EMG evidence [11].
Patients were divided into 6 groups according to their symptoms (Table 1).
Urodynamic findings, consisting of the prevalence of bladder and voiding phase dysfunction, were evaluated in different symptoms groups. Symptoms (including AUASI and urge incontinence) and age were compared in women with or without bladder dysfunction and with or without voiding phase dysfunction. Analysis of variance (ANOVA) was used for age and AUASI, and for the fixed variable of urge incontinence a Chi-square test was used. A p value of less than 0.05 was considered as statistically significant.
3. Results
In the study, the mean age of all patients was 27 years old (ranging between 18 and 39 years old). The distribution of women for different chief complaints is summarized in Table 1. Some 134 patients (42%) had a complaint of urge incontinence.
1) Frequency and urgency: 5 (9%) had DO, 30 (53%) had sensory urgency, and 22 (38%) had a normal cystometrogram. Some 18 patients with sensory urgency and the other 4 with DO also had dysfunctional voiding.
2) Frequency, urgency, and pain: A number of 52 patients (72.2%) had sensory urgency, 8 (11.11%) had DO, 5 (6.94%) had impaired compliance, and 7 (9.72%) had normal urodynamics. Of those patients with sensory urgency, some 28 had dysfunctional voiding; 3 patients impaired compliance, and 1 patient with DO had dysfunctional voiding.
3) Frequency, urgency, and urge incontinence: 88 patients (65.6%) had DO, 6 (4.4%) impaired compliance, 11 (8.2%) impaired compliance and DO, 17 (12.6%) sensory urgency, and 12 (9%) had a normal CMG, respectively. Of those patients with DO, 15 had dysfunctional voiding, and 5 were later diagnosed as MS. Some 5 patients with DO and impaired compliance had abnormal sphincter activity through voiding and all were later diagnosed with neurological diseases (3 tethered cord and 2 spinal cord hemangioma). Therefore, the total 10 of 134 women (7.46%) with urge incontinence were later diagnosed with neurological disease. Two patients with DO had an obstructing urethral stricture; 11 patients with sensory urgency had dysfunctional voiding; one patient with impaired compliance plus 4 patients with impaired compliance and DO had dysfunctional voiding. Three patients with a normal CMG had primary bladder neck obstruction.
4) Obstructive or voiding symptoms: Some 8 patients (25%) had DO, 3 (9.3%) had impaired compliance, 14 (43.7%) had sensory urgency, and 7 (21.8%) had a normal CMG. A number of 5 patients with DO, 12 patients with sensory urgency, 2 patients with impaired compliance and also 6 patients with normal CMG had dysfunctional voiding. Thus, 25 of 32 patients (78%) had urodynamic evidence of obstruction.
5) True incontinence: Ten patients.
6) Suprapubic pain only: Three had sensory urgency and others had normal CMG.
Table 2 includes the prevalence of urodynamic findings of bladder dysfunction and voiding phase dysfunction among patients with different symptoms.
Some 134 women had bladder dysfunction totally that 105 women (78.35%) of this group had urge incontinence (Table 3). Patients who had urge incontinence had
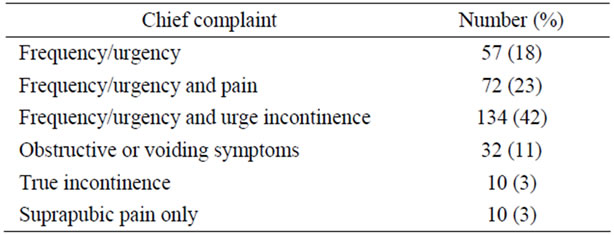
Table 1. Patients were divided into 6 groups according to their symptoms.
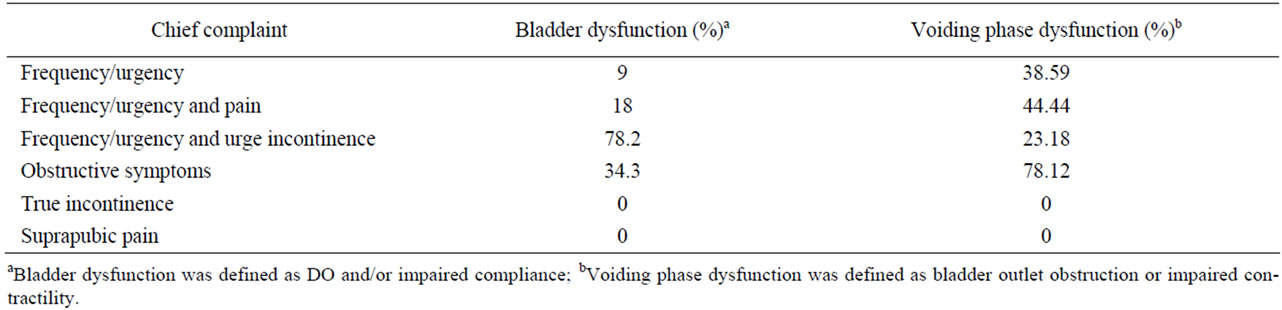
Table 2. Prevalence of bladder and voiding phase dysfunction among patients with different symptoms.
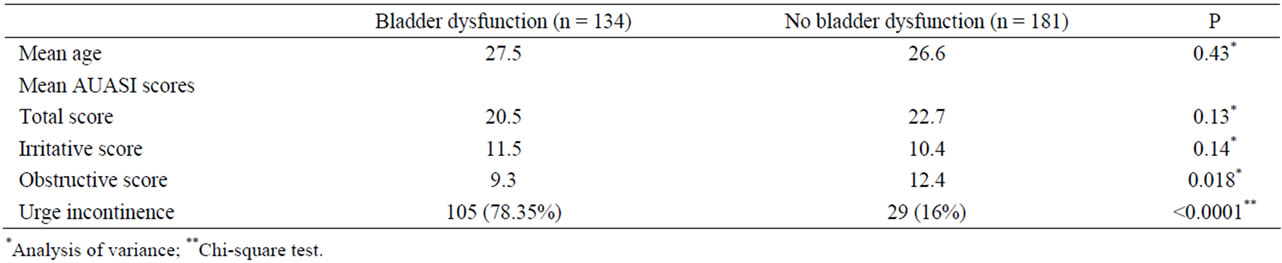
Table 3. Patients with or without bladder dysfunction characteristics and scores.
a significantly higher incidence of bladder dysfunction than those without it, 78.2% vs 14.3% (p < 0.0001). Patients with or without bladder dysfunction had similar total and Irritative AUASI scores, but obstructive scores were higher in patients without bladder dysfunction (Table 3).
Some 110 women had voiding phase dysfunction. Only 32 of those (22.7%) had a chief complaint of obstructive symptoms. Of the total of 32 patients with a chief complaint of voiding symptoms, some 25 patients (78%) had urodynamical voiding phase dysfunction. There was a significant difference between the incidence of the urge incontinence in the patients with voiding phase dysfunction (28%) and those without it (50%). Patients with voiding phase dysfunction had significantly higher obstructive and total AUASI scores, but similar irritative scores if compared with those without it (Table 4).
4. Discussion
The prevalence of urinary incontinence has been reported to be 5% - 20% in the prior studies that stress incontinence was the most prevalent type in many studies [1,2,4, 5,12,13]. Few studies have focused on urge incontinence in young women. A French study reported the prevalence of isolated urge incontinence to be zero in women with the age of less than 25 years old and 1.5% in those between 25 and 39 years old [14]. A study in central Sweden reported the rise in incontinence prevalence with age and parity, and that prevalence of pure urge incontinence was only 2.1% in 20 - 59 years old women [15].
The urodynamic study before LUTS treatment enables us to diagnose problems created by dangerous conditions such as occult neurological diseases. Since urodynamics has low morbidity, it is better for young women to undergo urodynamics before starting the treatment.
Our study showed that urge incontinence was highly suggestive of urodynamic abnormalities. In our study, 82.8% of women with urge incontinence presented DO, voiding phase dysfunction, or both in urodynamic study, however, 73.8% of them had DO only. Ten women in this group (7.46%) were considered as occult neurological disease after neurological workup. Of those patients with the chief complaint of obstructive symptoms, 78% had voiding phase dysfunction.
Urge incontinence and obstructive symptoms are good predictors of a diagnostic urodynamic study. The complete neurological evaluation must be done for the young women with significant urodynamic abnormalities that can not be justified by other conditions. In this study, neurological evaluation was performed for 30 patients. The diagnosis of neurological disease was proposed in 10 of them, 5 with detrusor overactivity, and 5 with both detrusor overactivity and impaired compliance.
AUASI is a helpful score for explaining LUTS in women. AUASI has been used to evaluate LUTS in women [16,17], and has shown the degree of bother from symptoms and quality of life in both men and women [18]. Women with voiding phase dysfunction had higher total and obstructive scores than those without it. Irritative scores were similar to each other. Thus, in women without obstructive symptoms, the AUASI could be useful in deciding to perform urodynamics. This shows the benefit of voiding phase evaluation when perform urodynamic study [16]. The total and irritative scores in the
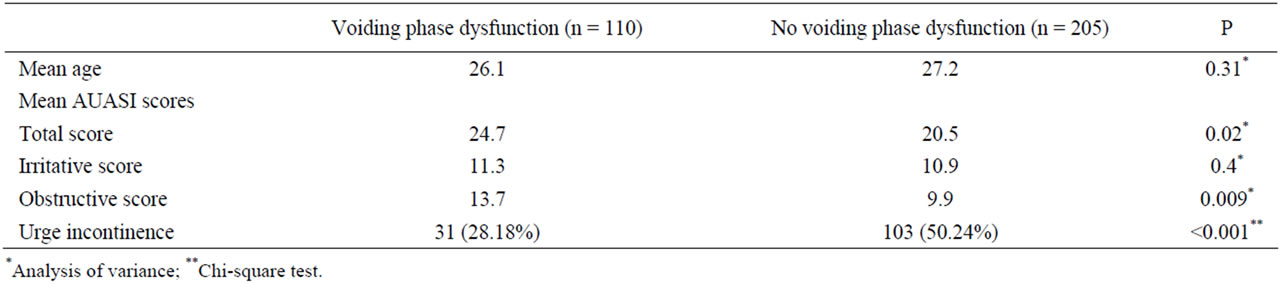
Table 4. Patients with or without voiding phase dysfunction characteristics and scores.
women with or without bladder dysfunction are similar to each other. Voiding scores were higher in women without bladder dysfunction than those with it. Therefore, the AUASI is a useful instrument in selecting young women for urodynamic performance.
Other indexes evaluated in our study were voiding diaries, intake diaries, uroflowmetery, and postvoid residual volume. Diaries were especially useful in diagnosis of excessive fluid intake as a cause of high urine output in young women. The urodynamic study was not helpful in those patients. When uroflowmetery or PVR are abnormal, it may show voiding phase dysfunction. Therefore, urodynamic study could be useful in such patients.
It may be concluded that when young women have only overactive bladder symptoms, without any obstructive complaints or neurological signs and symptoms, with normal emptying, normal urine analysis, and normal physical examination, could be treated empirically. We can also perform empiric therapy when uroflowmetery is normal.
5. Conclusion
Young women present different symptoms of lower urinary tract. Urodynamic study may be helpful in the evaluation of this group. In particular, patients with urge incontinence and voiding symptoms may have urodynamic abnormalities. Urge incontinence and bladder dysfunction can predict an occult neurologic disease. A neurological assessment is recommended for the patients that show significant urodynamic abnormalities that cannot be justified otherwise. When young women have only overactive bladder symptoms, without any obstructive and neurological signs and symptoms, with normal emptying, urine analysis, and physical examination, could be treated empirically.
REFERENCES
- S. A. E. Hunskaar, K. Burgio, et al., “Epidemiology and Natural History of Urinary Incontinence,” In: P. K. S. Abrams and A. Wein Eds., Incontinence: First International Consultation on Incontinence, Plymbridge, Plymouth, 1999, pp. 199-226.
- L. H. Wolin, “Stress Incontinence in Young, Healthy Nulliparous Female Subjects,” Journal of Urology, Vol. 101, No. 4, 1969, pp. 545-549.
- Z. Simeonova and C. Bengtsson, “Prevalence of Urinary Incontinence among Women at a Swedish Primary Health Care Centre,” Scandinavian Journal of Primary Health Care, 1990, Vol. 8, No. 4, pp. 203-206. doi:10.3109/02813439008994959
- H. Sandvik, S. Hunskaar, A. Seim, R. Hermstad, A. Vanvik and H. Bratt, “Validation of a Severity Index in Female Urinary Incontinence and Its Implementation in an Epidemiological Survey,” Journal of Epidemiology & Community Health, Vol. 47, No. 6, 1993, pp. 497-499. doi:10.1136/jech.47.6.497
- D. Hagglund, H. Olsson and J. Leppert, “Urinary Incontinence: An Unexpected Large Problem among Young Females. Results from a Population-Based Study.” Family Practice, Vol. 16, No. 5, 1999, pp. 506-509. doi:10.1093/fampra/16.5.506
- M. J. Barry, F. J. Fowler Jr., M. P. O’Leary, et al., “The American Urological Association Symptom Index for Benign Prostatic Hyperplasia,” Journal of Urology, Vol. 148, No. 5, 1992, pp. 1549-1557.
- W. Schafer, P. Abrams, L. Liao, A. Mattiasson, F. Pesce, A. Spangberg, A. M. Sterling, N. R. Zinner and P. van Kerrebroeck, “Good Urodynamic Practices: Uroflowmetry, Filling Cystometry, and Pressure-Flow Studies,” Neurourology and Urodynamics, Vol. 21, No. 3, 2002, pp. 261-274.doi:10.1002/nau.10066
- E. Gary, M. D. Leach and K. Y. Scott, “Post-Prostatectomy Incontinence: Part I. The Urodynamic Findings in 107 Men,” Neurourology and Urodynamic, Vol. 11, No. 2, 1992, pp. 91-97. doi:10.1002/nau.1930110203
- V. W. Nitti, L. M. Tu and J. Gitlin, “Diagnosing Bladder Outlet Obstruction in Women,” Journal of Urology, Vol. 161, No. 5, 1999, pp. 1535-1540. doi:10.1016/S0022-5347(05)68947-1
- J. G. Blaivas and A. Groutz, “Bladder Outlet Obstruction Nomogram for Women with lower Urinary Tract Symptomatology,” Neurourology and Urodynamic, Vol. 19, No. 5, 2000, pp. 553-564. doi:10.1002/1520-6777(2000)19:5<553::AID-NAU2>3.0.CO;2-B
- K. V. Carlson, S. Rome and V. W. Nitti, “Dysfunctional Voiding in Women,” Journal of Urology, Vol. 165, No. 1, 2001, pp. 143-147. doi:10.1097/00005392-200101000-00035
- T. Crist, H. M. Singleton and G. G. Koch, “Stress Incontinence and the Nulliparous Patient,” Obstetrics & Gynecology, Vol. 40, No. 1, 1972, pp. 13-17.
- K. Bo, R. Stien, S. Kulseng-Hanssen and M. Kristofferson, “Clinical and Urodynamic Assessment of Nulliparous Young Women with and without Stress Incontinence Symptoms: A Case-Control Study,” Obstetrics & Gynecology, Vol. 84, No. 6, 1994, pp. 1028-1032.
- L. Peyrat, O. Haillot, F. Bruyere, J. M. Boutin, P. Bertrand and Y. Lanson, “Prevalence and Risk Factors of Urinary Incontinence in Young and Middle-Aged Women,” British Journal of Urology International, Vol. 89, No. 1, 2002, pp. 61-66. doi:10.1046/j.1464-410X.2002.02546.x
- E. Samuelsson, A. Victor and K. Svardsudd, “Determinants of Urinary Incontinence in a Population of Young and Middle-Aged Women,” Acta Obstetricia et Gynecologica Scandinavica, Vol. 79, No. 3, 2000, pp. 208-215. doi:10.1080/j.1600-0412.2000.079003208.x
- K. V. Carlson, J. Fiske and V. W. Nitti, “Value of Routine Evaluation of the Voiding Phase When Performing Urodynamic Testing in Women with Lower Urinary Tract Symptoms,” Journal of Urology, Vol. 164, No. 5, 2000, pp. 1614-1618. doi:10.1097/00005392-200011000-00036
- A. Groutz, J. G. Blaivas, G. Fait, A. M. Sassone, D. C. Chaikin and D. Gordon, “The Significance of the American Urological Association Symptom Index Score in the Evaluation of Women with Bladder Outlet Obstruction,” Journal of Urology, Vol. 163, No. 1, 2000, pp. 207-211. doi:10.1016/S0022-5347(05)68007-X
- H. M. Scarpero, J. Fiske, X. Xue and V. W. Nitti, “American Urological Association Symptom Index for Lower Urinary Tract Symptoms in Women: Correlation with Degree of Bother and Impact on Quality of Life,” Urology, Vol. 61, No. 6, 2003, pp. 1118-1122. doi:10.1016/S0090-4295(03)00037-2
NOTES
*The authors declare that they have no conflict of interest.

