Advances in Molecular Imaging
Vol.08 No.04(2018), Article ID:87763,10 pages
10.4236/ami.2018.84006
Acute Mesenteric Ischemia: A Challenging Diagnostic Disease―Four Cases Reports and Literature Review (AMI)
Danilo Coco1, Silvana Leanza2
1Augusto Murri Hospital, Fermo, Italy
2Carlo Urbani Hospital, Jesi (Ancona), Italy
Copyright © 2018 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: May 19, 2018; Accepted: October 8, 2018; Published: October 11, 2018
ABSTRACT
Acute Mesenteric Ischemia (A.M.I.) is a potentially life-threatening condition syndrome due to inadequate or completely absent blood supply through superior or inferior mesenteric artery. The etiologies are various. Early diagnosis is essential to improve the clinical outcome. Despite advances in knowledge of pathophysiology, laboratory diagnosis and imaging techniques, acute intestinal ischemia is still associated with mortality rates.
Keywords:
Acute Mesenteric Ischemia, Anatomy, Etiology, Treatment

1. Introduction
Acute Mesenteric Ischemia (A.M.I.) is a potentially life-threatening condition syndrome due to inadequate or completely absent blood supply through superior or inferior mesenteric artery, resulting in hypoperfusion and eventual ischemia/gangrene of the bowel. There are five types of A.M.I. subdivided for anatomic vessels or etiologies: Non occlusive Mesenteric Ischemia (N.O.M.I.) (20% - 30%), Acute Mesenteric Arterial Embolism (A.M.A.E.) (50%), Acute Mesenteric Arterial Thrombosis (A.M.A.T) (15% - 25%) and Mesenteric Venous Thrombosis (M.V.T.) (5%). The fifth type is only 3% and is a clinical entity that occurs as a consequence of mechanical scenarios such as strangulation, intussusception, volvulus, tumor or trauma. A.M.I. accounting for 0.1% of hospital admissions. In large part because of the association with atherosclerosis. AMI is commonly considered a disease of the older population, with the typical age of onset being older than 60 years. The symptoms are non-specific so the diagnosis is very difficult .The radiologic image of choice is angio-TC-Scan. Treatment options include a range of options such as a few invasive management as percutaneous angioplasty plus stenting or thrombolytic therapy until surgical exploration [1] .
2. We Demonstrate Four Clinical Scenarios to Underline the Difficult Way to Join a Diagnosis and Treatment
1) Clinical scenario
A 85 years old Caucasian male presented to the ED with significant periumbilical abdominal pain, vomiting and fever. He presented a medical history of atrial fibrillation and anticoagulant therapy. During the physical examination, the patient was uncomfortable and in severe sepsis. Her vital signs were: blood pressure, 80/77 mm Hg; respiratory rate, 30 breaths/minute; heart rate, 129 beats/minute; and temperature superior of 38˚C. Oxygen saturation was 85% on room air. The abdominal examination revealed a distended abdomen that was severely tender to palpation, with rigidity, guarding, and rebound tenderness. Laboratory evaluation revealed high leukocytosis with a white blood cell (WBC) count of 30 per mm3. Arterial Blood Gases (ABG) demonstrated metabolic acidosis. Computed tomography angiography (CTA) reveled a superior mesenteric artery completely occlused after aorta origin, dilatated ileum and abdominal fluid (Figure 1). The patient was immediately started intravenous (IV) fluids of 2 l in 6 hours, Foley and jugular cathether vein canulation to support main arterial pressure and urine output. The patient was transferred to surgical services. A xifo-pubic incision laparotomy was made. A totally ischemic small and partially large intestine was found. We made only a laparostomy for a second look. The patient died the day after.
2) Clinical scenario
A 74 years old woman was referred to our hospital because of sudden onset of continuous to severe abdominal pain. The pain was associated with nausea and passage of dark, loose stools. His medical history was significant for permanent
Figure 1. Superior Mesenteric Artery completely occluded after its origin from aorta.
atrial fibrillation (AF), Diabetes Mellitus type II and rheumatoid arthritis and an history of sigma resection plus colostomy and then reversal surgery after perforated diverticulitis. On physical examination an irregular rhythm of approximately 120 bpm was found. Electrocardiogram ECG revealed Atrial Fibrillation (AF). His arterial blood pressure was 140/85 mmHg. The abdomen was soft and mildly tender to deep palpation. Laboratory data revealed a raised white cell count (15 × 109/L, normal value 4.0 - 10.0 × 109/L), creatine kinase (300 UL, normal value < 130 UL) and lactate dehydrogenase (260 UL, normal value < 240). Arterial Blood Gas (ABG) was normally. Other laboratory parameters were in the normal range. The plain radiograph of the abdomen showed two air fluid levels. Abdominal ultrasound indicated no abnormalities. The patient underwent contrast enhanced abdominal CT. It showed superior mesenteric artery completely occluded after 6 cm of aorta, small intestine pneumomatosi and abdominal fluid (Figure 2(a) & Figure 2(b)). Treatment with subcutaneous analgesics, oxygen, intravenous broad-spectrum antibiotics and fluid resuscitation with crystalloids (50 - 70 mL/kg daily), according to hemodynamic monitoring,


Figure 2. Inferior Mesenteric Artery (I.M.A.) not perfused after 6 cm at the origin of the aorta.
was commenced. A nasogastric tube was inserted to relieve distension. The patient was transferred to surgical services. After laparotomy, we found totally hypoperfused jejunum and ileum without necrosis. For this reason a laparostomy was made. 24 hours later, we performed a second-look surgery but we found a totally necrotic intestine.
3) Clinical scenario
A 63 years old man was admitted in our Emergency Room for acute abdominal pain associate with fever, vomiting, diarrhea and hypotension. His medical history reveled diabetes mellitus type II, hypertension, a history of Hairy Cell Leukemia with splenomegaly and cytopenia and endoprosthesis for thoracic aneurism. Physical examination demonstrated Temperature 37.5˚C, blood pressure 98/60 mmHg with mild orthostatic hypotension. Normal bowel sounds were noted in the abdomen, which was moderately tender in the right lower quadrant with focal rebound tenderness. The rectal exam was normal, with a stool sample negative for occult blood. Pelvic exam was unremarkable. WBC count was 24,300 per mm3. Serum chemistries and arterial blood gases (ABG) were remarkable for a mild anion gap metabolic acidosis. Abdomen TC scan with artery phases was performed, revealing S.M.A. occluded at aorta origin, small bowel dilatation, pneumomatosi, peritoneal fluid (Figure 3(a) & Figure 3(b)). After resuscitation with crystalloid through jugular vein catheterization, we explored the abdomen. We found a 30 cm necrotic ileum and hypoperfusion wall in the other part of small intestine. We performed a 30 cm of small bowel resection and superior mesenteric artery longitudinal arteriotomy, Fogarty exploration with


Figure 3. Superior Mesenteric Artery S.M.A. occluded.
thrombus extraction and a laparostomy. 24 hours later, we performed a second look finding an hypoperfusion small bowel. At third-look surgery we made resection of other 10 cm of small bowel and intestinal anastomosis. The patient was transferred in intensive care unit (ICU) where he died ten days later.
4) Clinical scenario
A 94 years old woman was referred to our hospital because of sudden onset of acute abdominal pain, dark stools and vomiting. She had a medical history of myocardial infarction. On physical examination, the abdomen was soft with moderate pain. Rectal exploration reveled mucorrea. Laboratory exams reveled only leukocytosis 11 per mm3. ABG and abdomen plain was unremarkable. We performed an CT-Scan that demonstrated a distal occluded S.M.A. (Figure 4(a) & Figure 4(b)) Having considered the patient’s age and in agreement with relatives, we treated her only with antithrombotic therapy and fluid resuscitation. She died one day later.
3. Anatomic Reasons for Intestinal Ischemia
Anatomy is crucial for the understanding of the pathophysiology, clinical presentation of intestinal ischemia. The splanchnic circulation is characterized by linking the 3 major vessels together [2] . The major connections are: the junction


Figure 4. Superior Mesenteric Artery S.M.A. occluded distally.
of the superior and inferior pancreaticoduodenal arteries (linking the celiac axis and the superior mesenteric artery SMA), the marginal artery of Drummond and the Riolan’s arch, between the middle colic and the left colic arteries (linking the superior mesenteric artery with the inferior mesenteric artery, IMA) and the collateralization between the inferior mesenteric artery and systemic circulation which occurs in the rectum (superior and middle rectal vessels) (Figure 5) [3] .
4. Etiology
Based on its etiology, acute mesenteric ischemia can be caused by various type of pathology such as Atrial fibrillation/flutter, Myocardial infarction, Infective endocarditis, Mechanical valve prostheses, Cardiomyopathies, Valvular disease for Arterial embolism (A.M.A.E.) which represents 50% of cases. Atherosclerosis, Low cardiac output, Congestive heart failure, Procoagulative status, Vasculitis (including Takayasu arteritis), Aortic/superior mesenteric artery aneurysm/dissection, Cardiac catheterization and angiography for acute mesenteric thrombosis (A.M.A.T.) 15% - 25% cases. Cardiogenic shock, Hypovolemic shock, Septic shock, Cardiac/Major abdominal surgery, Dialysis, Vasoconstricting agents for N.O.M.I 20% - 25% of cases. Causes of Mesenteric venous thrombosis (M.V.T.) include Hypercoagulability, Tumor causing venous compression or hypercoagulability (paraneoplastic syndrome), Infection, usually intra-abdominal (e.g., appendicitis, diverticulitis, or abscess), Venous congestion from cirrhosis (portal hypertension), Venous trauma from accidents or surgery, Increased intra-abdominal pressure from pneumoperitoneum during laparoscopic surgery, Pancreatitis. The fifth type is only 3% and is a clinical entity that occurs as a consequence of mechanical scenarios such as strangling, intussusception, volvulus, tumor or trauma [4] .
Figure 5. S.M.A. anatomy from Int. J. Morphol.
1) Clinical presentation
Symptoms and signs of mesenteric ischemia vary according to the etiology and the time of onset. They can be non diagnostic or non specific in almost 80% of cases. An abdominal pain was present in 95% (median of 24 hours duration). Other symptoms are nausea in 44%, vomiting in 35%, diarrhea in 35%, heart rate > 100 in 33%, “blood per rectum” and mucorrea in 16%, constipation in 7% [5] .
2) Diagnosis
Laboratory studies are nonspecific. The most common laboratory abnormalities are hemoconcentration, leukocytosis, and metabolic acidosis, with high anion gap and lactate concentrations [6] . High levels of serum amylase, aspartate aminotransferase, lactate dehydrogenase, and creatine phosphokinase are frequently observed at presentation, but none is sufficiently sensitive or specific to be diagnostic In these four cases we found an altered Blood Test Count with WBC ranging from 10 to major 20 mmc in 90% of cases associated of increased lactic acidosis with arterial blood gases evidences metabolic acidosis but only in the advanced disease. In one cases a part of altered WBC the laboratory studies were normal. Normal laboratory values do not exclude this diagnosis and do not justify delaying angiography when clinical suspicion exists. MDCT (multidetector CT) scan angiography is first line diagnostic images to discover acute intestinal ischemia with sensitivity 83%, specificity 93%, positive predictive value (at prevalence of 62%) 93%, negative predictive value (at prevalence of 62%) 61%. Findings on CT scan include: Mesenteric edema, Bowel dilatation, Bowel wall thickening, Intramural gas, Mesenteric stranding, portal vein gas, abdominal fluid [7] . Angiography is a diagnostic and therapeutic method and it is considered the gold standard for the diagnosis of acute mesenteric ischemia associated with MDCT scan [8] . Its sensitivities in five of six studies have ranged between 90% and 100%; specificity was reported in two of these studies to be 100%. Although it has serious risks, angiography provides the possibility of direct infusion of vasodilators in the setting of non-occlusive ischemia [9] .
4) Treatment
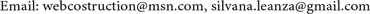
In the setting of suspected acute mesenteric ischemia, aggressive hemodynamic monitoring along with active resuscitation represents the first therapy. It should also include parenteral broad spectrum antibiotics to prevent bacterial translocation generated by ischemia associated with analgesia therapy. If there are no contraindications to anticoagulation, therapeutic intravenous heparin sodium should be administrated. The treatment of mesenteric ischemia depends on the causes and can be medical or surgical. In non-occlusive mesenteric ischemia, where there is no blockage of the arteries supplying the bowel, the treatment is medical. Thrombolytic medical treatment and vascular interventional radiological techniques have a growing role. When angiography is used to establish the diagnosis, the angiographic catheter should be left in the SMA for infusions of papaverine or other vasodilators. If the ischemia has progressed to the point that the affected intestinal segments are gangrenous, a bowel resection
Algorithm 1. Managment for the diagnosis and treatment of patients at risk of acute mesenteric ischemia (by “Acute Mesenteric Ischemia A Clinical Review” W. Andrew Oldenburg).
of those segments is called for [10] . Surgical revascularisation remains the treatment of choice for mesenteric ischaemia using longitudinal arteriotomy to perform embolectomy using a Fogarty catheter or distal bypass graft anastomosis. In most of cases multiple re-laparotomies are needed to obtain that news dead segments are removed after first operation and a second-look or even a third-look operation allows assessing segments that are borderline and that may be savable after revascularization [11] .
5) Prognosis
Acute Mesenteric Ischemia (A.M.I.) is a potentially life-threatening condition syndrome. Prognosis is very poor and account for a mortality range from 50% to 90% for A.M.A.E, A.M.A.T and N.O.M.I and account of 30% for M.V.T. [12] .
5. Discussion
Despite advances in knowledge of pathophysiology, laboratory diagnosis and imaging techniques, acute intestinal ischemia is still associated with mortality rates of more than 80%. Atrial fibrillation, myocardial disease or vascular disease and advanced age are the most common etiology. Differentiation between viable and nonviable, necrotic bowel tissue is done by exploratory laparotomy. A second-look laparotomy (after 24 - 48 hours) is recommended, even after successful primary intervention, because the intraoperative assessment of bowel viability [13] . Early diagnosis is the only best change but acute intestinal ischemia still remains a challenging diagnostic disease [14] . An algorithm management for the diagnosis and treatment of patients at risk of acute mesenteric ischemia is necessary to following the right steps (Algorithm 1) [15] .
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this paper.
Cite this paper
Coco, D. and Leanza, S. (2018) Acute Mesenteric Ischemia: A Challenging Diagnostic Disease―Four Cases Reports and Literature Review (AMI). Advances in Molecular Imaging, 8, 59-68. https://doi.org/10.4236/ami.2018.84006
References
- 1. Panes, J. and Pique, J.M. (2009) Intestinal Ischemia. In: Yamada, T., Ed., Textbook of Gastroenterology, 5 th Edition, Blackwell Publishing, Hoboken, 2811-2831. https://doi.org/10.1002/9781444303414.ch83
- 2. Tendler, D.A. and Lamont J.T. (2009) Acute Mesenteric Ischemia. UpToDate. https://www.uptodate.com
- 3. Rosenblum, J.D., Boyle, C.M. and Schwartz, L.B. (1997) The Mesenteric Circulation. Anatomy and Physiology. Surgical Clinics of North America, 77, 289. https://doi.org/10.1016/S0039-6109(05)70549-1
- 4. Boley, S.J., Brandt, L.J. and Veith, F.J. (1978) Ischemic Disorders of the Intestines. Current Problems in Surgery, 15, 1-85. https://doi.org/10.1016/S0011-3840(78)80018-5
- 5. Hunter, G.C. and Guernsey, J.M. (1988) Mesenteric Ischemia. Medical Clinics of North America, 72, 1091-115. https://doi.org/10.1016/S0025-7125(16)30731-3
- 6. Alpern, M., Glazer, G. and Francis, I. (1988) Ischemic or Infarcted Bowel: CT Findings. Radiology, 166, 149-152. https://doi.org/10.1148/radiology.166.1.3336673
- 7. Kao, L.S. and Lee, T. (2009) PreTest Surgery: PreTest Self-Assessment and Review. McGraw-Hill Medical, New York.
- 8. Meng, X., Liu, L. and Jiang, H. (2010) Indications and Procedures for Second-Look Surgery in Acute Mesenteric Ischemia. Surgery Today, 40, 700-705. https://doi.org/10.1007/s00595-009-4140-4
- 9. Brandt, L.J. and Boley, S.J. (2000) AGA Technical Review on Intestinal Ischemia. American Gastrointestinal Association. Gastroenterology, 118, 954-968. https://doi.org/10.1016/S0016-5085(00)70183-1
- 10. Florian, A., Jurcut, R., Lupescu, I., Grasu, M., Croitoru, M. and Ginghina, C. (2010) Mesenteric Ischemia—A Complex Disease Requiring an Interdisciplinary Approach. A Review of the Current Literature. Romanian Journal of Internal Medicine, 48, 207-222.
- 11. Andrew Oldenburg, W., Louis Lau, L., Rodenberg, T.J., Edmonds, H.J. and Burger, C.D. (2004) Acute Mesenteric Ischemia A Clinical Review (REPRINTED). Archives of Internal Medicine, 164, 1054-1062. https://doi.org/10.1001/archinte.164.10.1054
- 12. Christensen, M.G., Lorentzen, J.E. and Schroeder, T.V. (1994) Revascularisation of Atherosclerotic Mesenteric Arteries: Experience in 90 Consecutive Patients. European Journal of Vascular Surgery, 8, 297-302. https://doi.org/10.1016/S0950-821X(05)80145-8
- 13. Endean, E.D., Barnes, S.L., Kwolek, C.J., Minion, D.J., Schwarcz, T.H. and Mentzer Jr., R.M. (2001) Surgical Management of Thrombotic Acute Intestinal Ischemia. Annals of Surgery, 233, 801-808. https://doi.org/10.1097/00000658-200106000-00010
- 14. Tola, M., Portoghese, A. and Maniga, A.M. (1997) Laparoscopic Second-Look in Acute Intestinal Ischemia [In Italian]. Minerva Chirurgica, 52, 527-530.
- 15. Seshadri, P.A., Poulin, E.C., Mamazza, J. and Schlachta, C.M. (1999) Simplified Laparoscopic Approach to “Secondlook” Laparotomy: A Review. Surgical Laparoscopy Endoscopy & Percutaneous Techniques, 9, 286-289. https://doi.org/10.1097/00129689-199908000-00012



