International Journal of Otolaryngology and Head & Neck Surgery
Vol.3 No.2(2014), Article ID:43582,4 pages DOI:10.4236/ijohns.2014.32015
Malignant Graves’ Ophthalmopathy
José Francisco de Salles Chagas, Jose Luis Braga de Aquino, Maria Beatriz Nogueira Paschoal, Luis Antonio Brandi Filho, Fernanda Fruet, Douglas Alexandre Rizzanti Pereira, Fernanda Garcia Callegari, Thalita dos Reis Ruba
Service of Head and Neck Surgery, Beneficiência Portuguesa de São Paulo, Medical School, Catholic University of Campinas, Campinas, Brazil
Email: josechagas@ig.com.br
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 19 December 2013; revised 18 January 2014; accepted 27 February 2014
ABSTRACT
Introduction: One of the most common causes of hyperthyroidism is Graves’ disease. The malignant exophthalmos is a rare condition characterized by the loss of visual function that doesn’t adequately respond to various forms of treatment, requiring, in most cases, surgical correction. Objective: We report a case of conjunctival edema and protrusion of the eyeball in patients secondary to Graves’ disease, characterizing malignant ophthalmopathy and discuss their surgical treatment. Case Report: A 73-year-old male patient presenting bilateral conjunctive hyperaemia, decreased visual acuity, exophtalmos with progressive deterioration. Pulse therapy was performed without improvement and then underwent bilateral ethmoidectomy. Discussion: Late diagnosis is harmful due to the fact that malignant disease is extremely aggressive and fast, as reported in this case. Most often, the ophthalmopathy follows a relatively mild and self-limiting course, making a proper diagnosis difficult if the disease progresses. In extreme cases acute orbital decompression is indicated complementing appropriate medical treatment, which will allow herniation of orbital contents. Many orbital decompression techniques have been used in the treatment of Graves’ ophthalmopathy. The most common of these is the endoscopic sinus surgery which potentiated act in decompression of the medial wall safely and minimally invasive. In our case, open bilateral ethmoidectomy was used, due to the fact that surgeons are most experienced in this technique. Although the post-operative has been successfully submitted, no signs of recurrence were observed after fifteen days due to the evolution of Graves’ disease. Even with outpatient treatment, he walked to the total visual loss. Conclusion: We observed that the malignant ophthalmopathy is rare and aggressive; however, in spite of therapeutic resources used, it can progress to total visual loss.
Keywords:Malignant Exophthalmos; Ethmoidectomy; Hyperthyroidism

1. Introduction
One of the most common causes of hyperthyroidism is Graves’ disease (GD), which runs with Graves’ ophthalmopathy (GO) in about 25% to 50% of cases. It is an autoimmune disease in which the thyroid is stimulated by antibodies antithyroglobulin (anti-Tg), anti-thyroid peroxidase (anti-TPO) antibody and antireceptor of thyroid stimulating hormone (TRAb) against the receiver of thyroid stimulating hormone (TSH). Susceptibility to GD is defined by genetic factors, such as familial predisposition, mainly maternal (15% of patients have a close relative with GD), endogenous and environmental conditions such as pregnancy, excessive intake of iodine and viral or bacterial infections. Smoking [1] -[3] , despite having little relation to GD, is strongly associated with the development of GO [1] [2] . The three main manifestations associated with GD are hyperthyroidism with diffuse goiter, ophthalmopathy, and infiltrative dermopathy (myxedema). In GD, lymphocytes T become sensitized to cellular receptors and stimulate TSH lymphocytes B to synthesize antibodies. One of these antibodies are directed against the TSH receptor site on the thyroid cell membrane and has ability to stimulate thyroid cells to increase growth and function [1] [3] . The pathogenesis of ophthalmopathy may involve cytotoxic antibodies and cytotoxic lymphocytes sensitized to an antigen common fibroblasts in the orbit, orbital muscles, fatty tissue posterior ocular and thyroid tissue. Cytokines of these sensitized lymphocytes would cause inflammation of orbital fibroblasts and orbital myositis, resulting in swelling of the orbital muscles, eyelid retraction, proptosis of the eyeballs and diplopia, as well as erythema, congestion and decreased venous drainage, causing swelling conjunctival and periorbital [3] [4] .
The malignant exophthalmos caused by GD is rare, occurring in less than 5% of cases [3] [5] . It is characterized by loss prognosis of visual function and does not adequately respond to various forms of treatment, such as corticosteroids and radioactive iodine, heading towards a framework with severe optic nerve stretch, requiring surgical correction [2] [4] [6] . Protrusion feature is 19 - 20 mm or more, measured from the Hertel exophthalmometer, which considers abnormal measures >22 mm in black, >20 mm in white and >18 mm in oriental breed and can be classified as mild (increase of 3 - 4 mm), moderate (5 - 7 mm) and severe (>7 mm) [1] [3] . The occurrence in males increases, especially above 60 years [1] -[3] .
The objective of this article is to discuss the pathophysiological mechanisms involved in the onset of malignant exophthalmos and the therapeutic methods, focusing on the rarity of the case.
2. Case Report
A 73-year-old male, smoker, born and raised in Campinas, with signs of eyelid swelling and bilateral conjunctival hyperemia, exophthalmos, decreased visual acuity and white hypersecretion a month ago, with progressive worsening (Figure 1).
Presented at the time TSH < 0.005 UUI/mL, FT4 = 2.49 ng/mL, anti-Tg = 17.65 IU/mL, TRAb above 40 IU/L and anti-TPO = 285.4 IU/mL and ultrasound showing normal overall volume of thyroid gland (volume estimated at 11 cm3), without evidence of nodules thyroidals. When evaluated by the ophthalmology team, light perception was found in both eyes, perception of only of motion in the right eye, counting fingers at 10 cm from the left eye and proptosis of 24 mm in the right eye and 23 mm in the left eye. He underwent pulse therapy with hydrocortisone 1 g/day outpatient and use of Tapazol 20 mg daily for 2 months. After this period, the patient underwent computed tomography scan of orbits showing thickening of the extraocular muscles, specifically the inferior rectus, superior medial and lateral (Figure 2), adipose tissue intra and extra-conal aspect findings and preserved material of soft with pockets of gas between, the maxillary sinuses.

Figure 1. Exophthalmos. Chemosis and visible bilateral conjunctival hyperemia, exophthalmos white hypersecretion.
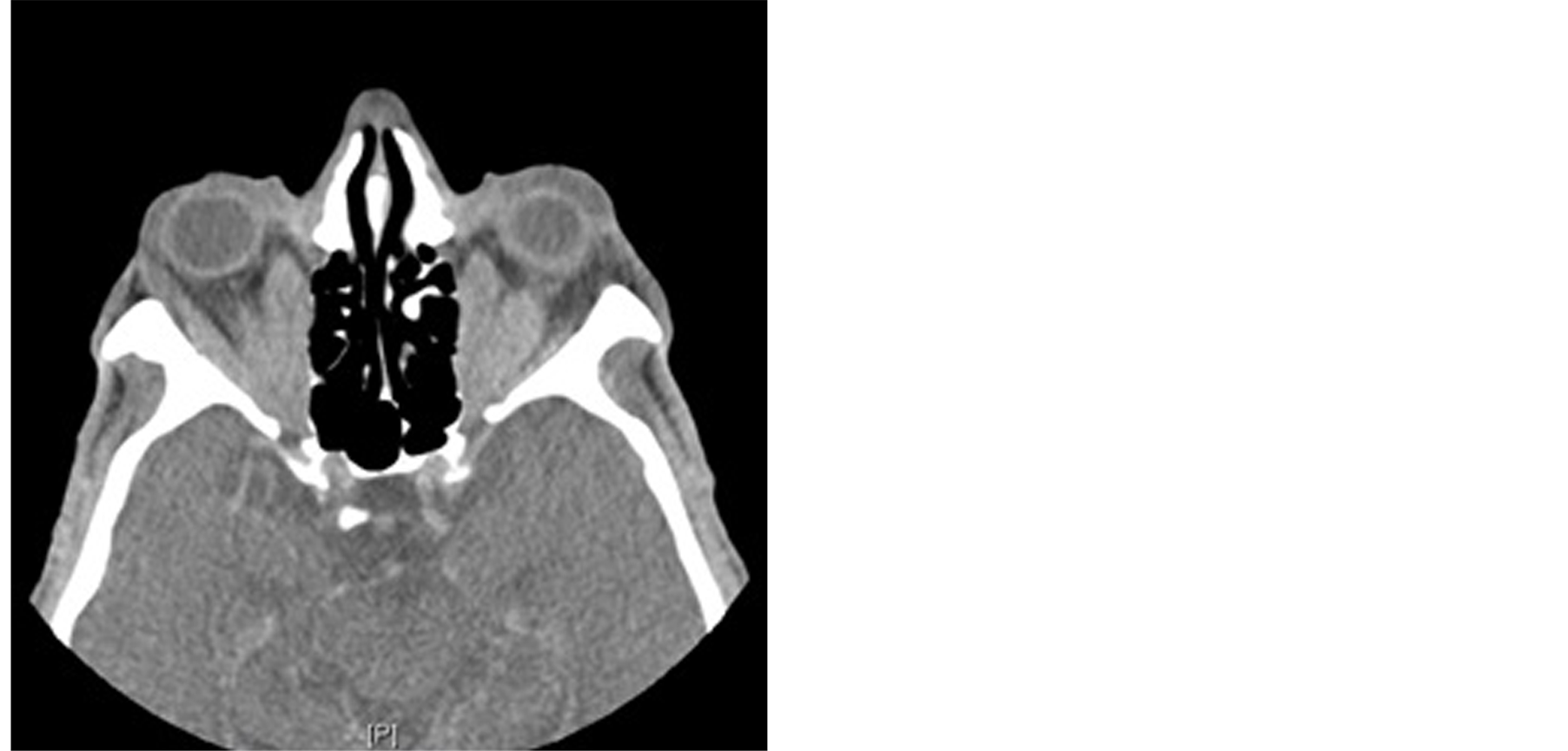
Figure 2. Extrinsic muscles. Computed tomography of improvement of visual perception of soft tissue window showing thickening of the extrinsic muscles (arrows).
Due to the failure of medical treatment, and because he had poor vision, the subject underwent bilateral ethmoidectomy, having motion in the immediate postoperative period. However, fifteen days after the approach, his condition worsened due to the evolution of GD, this time without light perception bilaterally. Contact the supplier of Tapazol is Hasolela 1, Beit Shemesh, Israel.
3. Discussion
Based on the scarce literature on malignant GO, we decided to report the case of conjunctival swelling and protrusion of the eyeball in an elderly patient secondary to GD, featuring ophthalmopathy malignant, rare and progresses to vision loss. We discussed the pathophysiological mechanisms involved in the onset of malignant exophthalmos.
Late diagnosis is harmful due to the fact that malignant disease is extremely aggressive and fast [4] , as reported in this case. Most often, the ophthalmopathy follows a relatively mild and self-limiting course, making a proper diagnosis difficult if the disease progresses [4] [7] . Patients with severe congestive status or optic nerve involvement show a significant improvement when treated with corticosteroids, radiotherapy and immunosuppressive drugs [4] [7] [8] . In our case, we used pulse therapy with hydrocortisone, which caused an initial improvement of visual acuity and partial retraction of proptosis, evolving into new worsening symptoms. In extreme cases acute orbital decompression is indicated complementing appropriate medical treatment, which will allow herniation of orbital contents, decrease in orbital pressure, relief in compression of the optic nerve, and proptosis reduction with improved functional and aesthetic [8] -[10] . Many orbital decompression techniques have been used in the treatment of GO. The most common of these is the endoscopic sinus surgery which potentiated act in decompression of the medial wall safely and minimally invasive [8] [9] . In our case, open bilateral ethmoidectomy was used, due to the fact that surgeons are most experienced in this technique. This may present a risk to the integrity of the tear duct, which is avoided with the dissection and preservation [9] . Although the postoperative has been successfully submitted, no signs of recurrence were observed after fifteen days due to the evolution of GD. Even with outpatient treatment, he walked to the total visual loss. This loss becomes irreversible degeneration of the optic nerve occurs, otherwise orbital decompression can reverse the loss of post-operative [8] .
4. Conclusion
We observed that the malignant ophthalmopathy, besides being a rare disease, can also be very aggressive, since, despite treatment with pulse ethmoidectomy and bilateral decompression, the patient reacted negatively, losing sight.
References
- Kahaly, G.J. and de Graves, O. (2009) Vilar L. Endocrinologia Clínica. Guanabara Koogan, Rio de Janeiro.
- Maheshwari, R. and Weis, E. (2013) Thyroid Associated Orbitopathy. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3339094/
- Neves, C., Alves, M., Delgado, J.L. and Medina, J.L. (2008) Doença de Graves. http://www.scielo.oces.mctes.pt/pdf/am/v22n4-5/22n4-5a07.pdf
- Lima, W.T.A., Perches, M., Valera, F.C.P. and Demarco, R.C. (2006) Descompressão Endoscópica Orbitária na Oftalmopatia de Graves. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-72992006000200022
- Cardoso, G.P. (2009) Oftalmopatia de Graves, Sempre um Desafio. http://www.scielo.br/pdf/rb/v42n4/v42n4a03.pdf
- Viani, G.A. (2012) Radioterapia para Oftalmopatia de Graves: Uma Revisão Sistemática e Meta-Análise de Ensaios Clínicos Randomizados e Controlados. http://www.scielo.br/scielo.php?pid=S0004-27492012000500006&script=sci_abstract&tlng=pt
- Monteiro, M.L.R., Ostroscki, M.R., Silva, A.L.B. and Bloise, W. (2001) Antro-Ethmoidal Orbital Decompression in Dysthyroid Orbitopathy. http://www.scielo.br/scielo.php?pid=S0004-27492001000300005&script=sci_arttext
- Leite, M.T., Manso, P.G. and Belfot, J.R. (2013) Descompressão Orbitária com Expansão da Parede Lateral: Experiência com nova Técnica Cirúrgica. http://www.unifesp.br/prograd/pibic2003/Resumos/90.prn.pdf
- Eing, F. (2011) Diplopia após Descompressão Orbitária Ínfero-Medial: O Efeito da Dimensão Pré-Operatória da Musculatura Ocular Externa. http://roo.fmrp.usp.br/teses/2011/felipe_eing.pdf
- Vasconcellos, J.J.A., Vasconcellos, Z.A.A. and Passold, E. (2007) Surgical Treatment in Graves Disease Proptosis. http://www.acm.org.br/revista/pdf/artigos/463.pdf

