Open Journal of Medical Psychology
Vol.2 No.2(2013), Article ID:30667,4 pages DOI:10.4236/ojmp.2013.22012
Parental Awareness and Perception of Their Children’s Body Size
Department of Psychology, University of Northern British Columbia, Prince George, UK
Email: *gcp@unbc.ca
Copyright © 2013 Jane Allen, Glenda C. Prkachin. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received January 28, 2013; revised March 3, 2013; accepted March 11, 2013
Keywords: Perception of Size; Change Blindness; BMI Categories; Childhood
ABSTRACT
Objective: To investigate parents’ misperception of their active children’s size. Subjects: One hundred and forty male or female parents and their children from a youth soccer league participated. Actual Child Body Mass Index (BMI) percentiles and BMI categories were compared to the results of a Body Size Estimation Task and lifestyles questionnaire results. Results: Parents underestimated the body size of their children and placed them in a lower BMI category than the children actually belonged in. As was the case in other studies children in the unhealthy or at risk to become overweight category where seen as a healthy weight. Unlike other studies, many healthy weight children were seen as underweight. Conclusions: An explanation of body size misperception and underestimation of body size may be “change blindness”. The growing prevalence of obesity in children may be better addressed by focusing on the parents’ apparent lack of concern about excess childhood weight and the parents’ identification of excess childhood weight as “just normal” rather than seeing excess weight as a potential problem.
1. Introduction
The World Health Organization [1,2] describes obesity as one of the most blatantly visible, yet most neglected public health problems today. However, there is not just an increase in obesity, there appears to be an increase in the weight of all children. The conclusion from a 2010 health survey was that all Canadian “children are taller, heavier, fatter and weaker” than in the previous decade [3].
The origin of obesity for children and adults is obviously a complex and interconnected effect of genetics, anatomy, physiology, behaviour, and the social environment. The factors that result in the development and maintenance of obesity in children may differ from that of adults since the potential to develop obesity during childhood is likely to be influenced by differential growth, metabolic and activity factors. Consequently the risk factors for an individual child and the appropriate changes to a child’s diet for healthy growth will likely require modifications beyond simple reduction of diet and lifestyle changes. However, recent studies have provided another perspective by focusing on the influence of parental awareness and perception of their child’s weight.
Baughcum et al. [4] simply asked the mothers of overweight children if they felt their child was very underweight, a little underweight, about the right weight, a little overweight, or very overweight. They reported that 79% of mothers failed to perceive their overweight child as overweight. A later study [5] reported that nearly one third (32.1%) of the mothers of children age 2 to 11 years of age reported their overweight child as “about the right weight”. Misperception of overweight children by British parents’ was assessed in a large sample of 3 to 5 years old children and found that only 17.1% of the parents of obese children accurately described their overweight child as overweight [6]. We can assume that the inaccuracy was due to a misperception by 80% of the parents that their overweight children weighed less than they did since no parent judged their child to be very overweight. Rather the parent perceived their child to be “just about right”. Similar results with large sample sizes have been reported in the UK [7] and USA [8,9]. The conclusion from these studies is that parents with overweight children do not identify them as being overweight. This suggests that even when a child’s weight problem is “blatantly visible” to other people, parents are evidently unaware and unconcerned.
Baur [10] speculated about the reasons parents’ underestimate the weight of their overweight children and the consequences of these misperceptions. He suggested that overweight has become a relative judgment in a culture that is desensitized to the sight of increased body fatness and there is a stigma attached to overweight that may have resulted in denial of responsibility and parental control over the child’s eating behavior. However, it is unlikely that most people are very accurate at perceiving weight and height without a referent. In addition we need to determine what referent the individual making the judgment is using. In the majority of these studies the parent is asked to remember the child’s size or compare it to pictures of other children rather than making an immediate comparison of their child in a background of other children of various sizes. When parents were provided with lifelike drawings of children based on the different BMI categories they were more likely to select the sketches of the heavier child as representing their overweight child [8]. The drawings in this study included depictions of obvious fat in areas of the body for the heavier child sketches that were based on photographs of actual children. While they are accurate representations of the overweight child they may not represent the parent’s actual image of the child. After children start to bath and dress themselves a parent would rarely see the distribution of fat on their bodies, but they would have an image of their overall size.
In addition to a referent, perception of the child’s size is also a cognitive process since size must be translated to a label or category. It is likely that it is at this stage of the perceptual process that the stigma attached to being overweight could bias the misperception or ambiguous perception towards a lower category. Simply put, the misperception of children’s weight could be an error of cognition rather than lack of concern about their child’s weight, since it can be overcome (outgrown), or denial of responsibility and parental control over the child’s eating behavior.
In this study we focused on body size and parents’ ability to classify their child in the correct body mass index (BMI) category. Specifically, we asked if parents would underestimate or over-estimate their child’s body size in relation to a visible referent for a child’s body mass percentile. The parents were asked to identify a representation of four different sized drawings of soccer players while observing their own child in a soccer uniform and against a background of other children dressed in similar uniforms. We used cartoon like drawings as a graphic representation of the four BMI categories in order to minimize identification and emphasis on weight and fat in any particular area of the body.
To date, research concerning parental perception and awareness has focused on overweight children. We expected that the lack of awareness of body size is a perceptual and cognitive difficulty that occurs regardless of a child’s actual body mass category. In other words, we hypothesized that parents would misperceive the size of their child regardless of the child’s actual size. Correspondingly, we attempted to determine if this perceptual change blindness might be responsible for parents’ lack of concern if their child was at risk of being overweight or if the child was already overweight, by including a questionnaire about the child’s activities, family eating and the attitude of the parents.
2. Method
2.1. Participants
One hundred and forty parents and children were recruited for this study during a weekend tournament at a large soccer field. The pitches are located in a single central location in the city. Soccer is popular and the youth organization attracts a representative sample of children in the city. Child participants were from ages five to sixteen (M = 61, F = 58). Parents were both male (37) and female (82) and 119 parent-child pairs completed each research task.
2.2. Apparatus & Materials
Parents were asked to choose one of the four body size drawing, which best represented their child. Each figure represented a body mass index category as defined by body mass index percentiles for individuals aged two to twenty. Parents were simply asked to circle the most representative figure. A standard scale and rigid measuring tape was adjusted to take into account the added weight and height of the cleats. The uniforms were provided by the soccer association and apart from the colour of the banding were of identical shape and size-appropriate. The questionnaire consisted of 10-items examining eating behaviours, the child’s level of physical activity, and parent’s concern about their child's eating behaviour and weight. Parent’s demographic information was also requested.
2.3. Procedure
Research assistants approached parents on the sidelines and asked if they were interested in participating in a study looking at their ability to judge the size of their child. They were then given a full explanation of the purpose of the study and the informed consent forms. They were asked to complete the body size estimation task, the questionnaire, and bring their children over to our research area for height and weight measurements at their convenience. The child was asked if they would allow us to measure their size. Following the child’s measurements the researchers addressed questions about the research and results of the measurements.
2.4. Data Reduction and Analysis
Participant height and weight measurements were used to calculate Body Mass Index (BMI) percentiles (weight (kg)/height (m2) as per CDC guidelines for children aged 2 to 20 and participants were coded into one of four actual BMI (ABMI) categories. The number circled on the body size estimation task is referred to as the perceived BMI (PBMI). ABMI and PBMI were compared. Parent questionnaire responses were correlated with the ABMI and PBMI.
3. Results
The ABMI for the children ranged from the 6th to 99th percentile. Female ABMI percentiles ranged from 6th to 96th, and males from 14th to 94th. No child was classified as underweight. Seventy three percent (45 males and 42 females) were a healthy weight, 14% (9 males and 8 females) were at risk of becoming overweight, and 13% (7 males and 8 females) were overweight.
Parents’ estimates of their children’s BMI categories were dramatically different from the BMI category in which their children belonged. The ABMI and PBMI categories were compared and differed reliably t(115) = 15.3, p < 0.001. These results are described in Figure 1 and Table 1.
There was a significant correlation between the ABMI and PBMI, r(116) = 0.559, p < 0.000. Comparison of ABMI and PBMI are included in Table 1 and support the conclusion that underestimating the size of the children is not restricted to the overweight category.
Questionnaire results are included in Table 2’s matrix of correlations. In general, parents who estimated their child as being in the at risk of becoming overweight category, or who were actually at risk or overweight, were more accurate at describing their child’s weight and
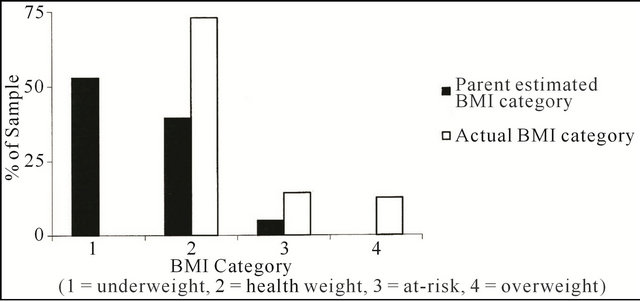
Figure 1. Actual BMI categories (ABMI) compared to parent estimated or perceived category (PBMI).
Table 1. Parents’ underestimation of the size of their children is not restricted to those with overweight children.
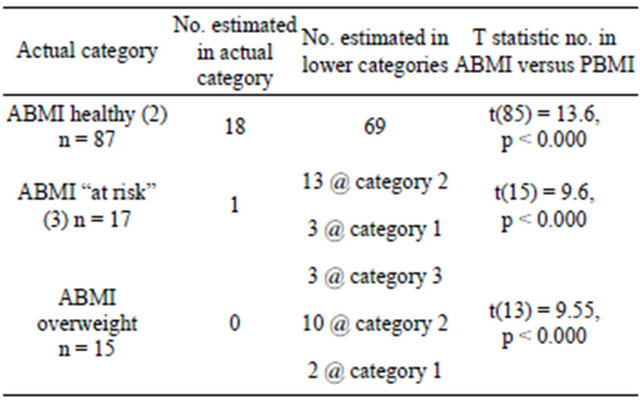
Table 2. Correlations between ABMI, PBMI and questionnaires.
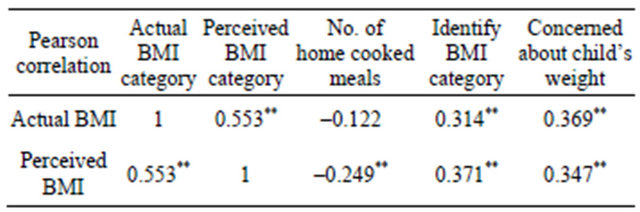
Note: *r significant ≤ 0.05, **r significant ≤ 0.01.
were more concerned about their child becoming overweight.
Of interest is the similarity of the correlations of the ABMI and PBMI for describing the child’s weight and parent’s concern about the child’s weight. These significant and positive correlations occurred for the “at risk” and overweight children in spite of the parent’s estimation that the child was much smaller than they actually were and described their weight as normal.
4. Discussion
In line with studies that examined parents’ perception of overweight children and our research hypothesis, the majority of parents (more than 50%) did not classify their children in their actual BMI category, but underestimated the size and placed them in a lower category. In addition, fifty percent of parents underestimated the size of their healthy weight children and placed them in the underweight category. This finding was not the result of the healthy weight children being close to the actual underweight category, since the misperception was distributed across the healthy weight category with 14 of the 26 participants with a child between the 70th and 84th ABMI identified by their parent as being in the underweight category.
As the children’s actual body size increased, there was a tendency to indicate increased concern about eating habits of their family, but these did not result in high or reliable correlations. A few of the parents expressed concern about a weight problem for their child, but, identify their child’s weight as “normal” on the questionnaire. Other parents identified their child as underweight but also described their child’s weight as “normal”. We used the term normal since “normal”, in common use, implies that the judgment is based on an internalized standard for a population as opposed to a more individual or personal assessment. Internalization of a shifting normalization for excess weight may be responsible for the apparent lack of concern by the parents. However, many parents misperceived their child’s size, not just the parent of the overweight child and almost all of the parents described their child’s weight as normal. Perhaps we need to consider the misperception of size and concern or evaluation of excess weight as separate psychological processes for the parent, with different consequences for interventions.
Perception of changes in size, like all perception of change is subject to a phenomenon called change blindness or attention blindness. We do not see children growing. We simply don’t notice something as obvious as Simons and Chabris’ [11] Gorilla in the room. We are blind or inattentive to them getting taller or fatter. Rather, we perceive that they have grown by comparing their size to an external referent, for example, fit of clothing, compared to our own height or other objects. Children generally only grow in one direction and if the internalized representation of the child has not recently been updated then the perception should be an underestimation of their size. Since the origin and consequence of change inattention is the same for overweight children and healthy weight children it is unnecessary to propose that the parents of unhealthy weight children are subject to unconscious denial or other perceptual mechanisms that differ from the parents of healthy weight children.
Baur [10] suggested that “It is ironic that such an obvious medical condition in children can apparently be almost invisible to the parents of such children”. Change in a child’s size isn’t “blatantly visible” or obvious to the parent of a child of any size. Being unaware of changes in weight and size is not the problem. Ultimately the parents’ psychological process of “normalizing” and faulty evaluation or lack of concern is the problem for the overweight child. It is possible that, by the time parents notice that their child could have a weight problem, the weight problem is already present or severe. In this way, body size misperception may be linked to the growing prevalence of obesity in children, but misperception of their size is not the cause.
REFERENCES
- World Health Organization, “Physical Status: The Use and Interpretation of Anthropometry,” Report of the WHO Expert Committee (WHO Technical Report Series, No. 854), WHO, Geneva, 1995.
- World Health Organization, “Obesity: Preventing and Managing the Global Epidemic,” Report of the WHO Expert Committee (WHO Technical Report Series, No. 894), WHO, Geneva, 2000.
- M. S. Tremblay, M. Shields, M. Laviolette, C. L. Craig, I. Janssen and S. C. Gorber, “Fitness of Canadian Children and Youth: Results from the 2007-2009 Canadian Health Measures Survey. Statistics Canada,” Health Reports, Vol. 21, No. 1, 2010, pp. 1-15.
- A. E. Baughcum, L. A. Chamberlin, C. M. Deeks, S. W. Powere and R. C. Witaker, “Maternal Perceptions of Overweight Preschool Children,” Pediatrics, Vol. 106, No. 6, 2000, pp. 1380-1386. doi:10.1542/peds.106.6.1380
- L. M. Maynard, D. A. Galuska, H. M. Blanck and M. K. Serdula, “Maternal Perceptions of Weight Status of Children,” Pediatrics, Vol. 111, No. 5, 2003, pp. 1226-1231.
- S. Carnell, C. Edwards, H. Croker, D. Boniface and J. Wardle, “Parental Perceptions of Overweight in 3 - 5 Years Olds,” International Journal of Obesity, Vol. 29, No. 1, 2005, pp. 353-355. doi:10.1038/sj.ijo.0802889
- A. N. Jeffery, L. D. Voss, B. S. Metcalf, S. Alba and T. J. Wilkin, “Parent’s Awareness of Overweight in Themselves and Their Children: Cross Sectional Study within a Cohort,” BMJ, Vol. 330, No. 2, 2005, pp. 23-24. doi:10.1136/bmj.38315.451539.F7
- K. C. Eckstein, L. M. Mikhail, A. Ariza, J. S. Thomson, S. C. Millard and H. J. Binns, “Parents’ Perceptions of Their Child’s Weight and Health,” Pediatrics, Vol. 117, No. 3, 2006, pp. 681-690.
- D. S. West, J. M. Raczynski, M. M. Phillips, Z. Bursac, C. H. Gauss and E. E. Montgomery, “Parental Recognition of Overweight in School-Age Children,” Obesity, Vol. 16, No. 3, 2008, pp. 630-636. doi:10.1038/oby.2007.108
- L. A. Baur, “Editorial: Childhood Obesity: Practically Invisible,” International Journal of Obesity, Vol. 29, No. 1, 2005, pp. 351-352. doi:10.1038/sj.ijo.0802931
- D. J. Simons and C. F. Chabris, “Gorillas in Our Midst: Sustained Inattentional Blindness for Dynamic Events,” Perception, Vol. 28, No. 9, 1999, pp. 1059-1074. doi:10.1068/p2952
NOTES
*Corresponding author.

