Open Journal of Respiratory Diseases
Vol.09 No.01(2019), Article ID:90630,10 pages
10.4236/ojrd.2019.91003
How to Implement Change in Asthma Management in a Developing Country
Uchenna Onubogu
River State University Teaching Hospital, Portharcourt, Nigeria

Copyright © 2019 by author(s) and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: January 20, 2019; Accepted: February 18, 2019; Published: February 21, 2019
ABSTRACT
The goal of asthma management is to control symptoms, reduce the need for short acting beta agonist, and maintain optimal pulmonary function, and normal physical activities. Uncontrolled asthma can lead to obesity, suboptimal pulmonary function, poor quality of life and mortality. Children with bronchial asthma in River State University Teaching Hospital were just receiving acute care in the emergency room with no concrete plan for a follow up care for their chronic asthma; as a result most of the patients had uncontrolled asthma. In the hospital, the situation led to increased emergency hospitalization, resulting in decreased bed availability, increased burden on manpower and health resource utilization thereby putting more pressure on the limited health resources. Using the Kotter’s model for change management, transformational and situational leadership style, the change in the desired quality and scope of health service rendered to asthmatic patients was successfully implemented; as a result there was a decrease in emergency room visit for acute asthma by 57.5% and an increase in the uptake of scheduled clinic visits for asthma control services. The effect of these changes was an improvement in the control of asthma and quality of life of our patient cohort. Implementation of change in health service delivery is a delicate process that needs a stepwise approach in order to successfully implement and sustain the desired change.
Keywords:
Bronchial Asthma, Health Service, Developing Country, Kotter’s Model, Leadership

1. Introduction
The goal of asthma management is to control symptoms, reduce the need for short acting beta agonist, and maintain optimal pulmonary function, and normal physical activities while ensuring that patients are satisfied with the quality of care they are receiving [1] . Uncontrolled asthma can lead to obesity, suboptimal pulmonary function, poor quality of life and mortality [2] [3] . This article will be discussing the change in the quality and scope of the health care rendered to children with bronchial asthma in River state University Teaching Hospital from January 2015 to December 2017. It will also be discussing the management of the change process and critically review the leadership theories that were used to effect that change.
2. Implementation Location
River State University teaching Hospital is a tertiary hospital in Port Harcourt city, Rivers state, Nigeria. It was initially known as Braithwaite Memorial Specialist hospital till April 2018 when it was officially upgraded and renamed in order to serve the River state University. The paediatric department contains 80 beds out of which 12 beds are in the emergency ward. The paediatric emergency department treats an average of 1724 children annually.
3. Change Management
Children with bronchial asthma in the hospital were just receiving acute care in the emergency room with no concrete plan for a follow up care for their chronic asthma. As a result, most of these children visited the emergency room regularly for quick relief of their acute symptoms without receiving follow up plans; this caused the patients to have a high frequency of uncontrolled asthma. In the hospital, the situation led to increased emergency hospitalization, resulting in decreased bed availability, increased burden on manpower and health resource utilization thereby putting more pressure on the limited health resources. In view of this, the consultant in charge of the respiratory unit, identified that there was a need for change in the care of bronchial asthma patients, to expand it beyond urgent care and include chronic asthma management as this would improve asthma control.
Recognizing what needs to change and why, are one of the first steps to enable that change [4] . Bringing about change within an organization can be challenging especially in health care service delivery, this is because many professionals with relatively autonomous regulating bodies, patients and careers have to work together to render patient care [5] . In order to successfully implement any change process, it is very important to recognize the potential barriers to implementing that change and strategize on how to overcome them [5] [6] . Organizations with strong leadership where improving patient care is the primary focus usually succeed in implementing progressive changes [5] . However, whatever change is being planned in the health industry, patient’s safety should never be compromised [4] .
Various change management models have been described, Kurt Lewin describes change as a three staged process involving an unfreezing stage in which people are suddenly made aware that the status quo is not good and that there is an urgent need to change to an improved and better place, this stage also involves a force field analysis aimed at the reduction of restraining forces and increasing the driving forces [7] [8] . The second phase involves the change process for those involved in making the necessary changes that are needed. It usually needs a lot of support in terms of training, coaching and continuous communication of the clear picture of the new process. The third stage is the refreezing in which the change has been institutionalized and stabilized, attaining a new norm [7] [8] .
Kotter on the other hand, described an eight step change model which involves; creating a sense of urgency, forming a guiding team, creating a vision with strategy, communicating the vision, empowering broad-based action, generating short term wins, consolidating the gains and finally making the change stick into the organization culture [9] [10] .
In discussing the process used to implement the change in the management of asthma, the consultant seemed to use the Kotter’s change model [10] . She started by setting the stage for the change she wanted to happen. First of all, she created a sense of urgency in her followers and put together a guiding team to see the rest of the hospital staff through that change. She was able to achieve this through setting up a meeting with members of her unit in order to educate and inform them of the impact of the prevailing system of care being rendered to asthma patients. She then taught them the standard guidelines for asthma management [11] aimed at symptom control, with all its benefits both for the patients and hospital. At the end of the meeting, the unit members made up of the consultant, one senior registrar, one junior registrar and two house officers formed a team that would guide the rest of the hospital through that change.
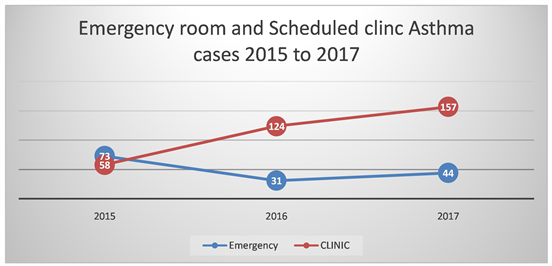
The guiding team then made decisions on things that needed to be done and the strategies they would use to bring about the change in the pattern of health care being rendered to asthma patients. The plan was to set up an asthma clinic that would run on the consultant’s allotted weekly clinic days, draw up an asthma treatment and discharge protocol to involve counselling and teaching about asthma home care and asthma clinic appointment within one week of being discharged from the hospital. The clinic was also structured to be able to accommodate those with recent attacks seen in the emergency room in order to have a rapid access to chronic asthma care. They also identified the key people that needed to be approached for approval to implement this change. In other to make this vision happen, the consultant had a meeting with the departmental head to communicate this vision and seek approval for implementing this change. She then tried to bring the whole department on board by teaching the department in a clinical meeting, drawing their attention to the draw backs of the status quo and the benefits of the new plan. She also highlighted what would be required for the clinic to run and what the new update to the asthma management protocol would entail. She clarified questions and worries that people had and reassured the major units affected by the change, mainly, the clinic and emergency department that a step down training would be done at those sections especially for those running shifts who were absent at the first meeting. One of the guiding team doctors was identified as the contact person for operation bottle necks. A step down training was later done and the individual staffs that would be directly affected by the new change were empowered with the skill and knowledge to carry out the modifications needed in their daily routine in order to implement the change. In the emergency room, the management protocol was updated and the discharge instruction was drawn up to include discharge to the asthma clinic with a clinic appointment communicated to the patient and caregiver. In the outpatient clinic, the nurses had to establish two parallel clinic lineups using the same waiting area one for the asthma clinic and the second for the routine general paediatric clinic. In the clinic, the patients were then assessed and given an asthma management plan which included a home treatment plan, they were also taught the importance of compliance with their treatment plan. In order to have an objective instrument to create a visible evidence for the success of this change, the clinic set up an asthma register which not only shows the increasing number of referrals to it but also tracks the severity of patients symptoms at first visit, degree of asthma symptom control, need for emergency room visits and patients compliance to treatment plan. Within the first year of implementation of implementation of this change, records showed that the number of asthma clinic visits to the emergency room dropped by 57.5% while outpatient clinic attendance increased steadily at a rate of 113% in the first year and 26.6% in the second year (Figure 1). With the drop in emergency room visits seen in 2016 there was also a slight increase in emergency room attendance in 2017, the reason could be because of the improvement in the hospitals’ reputation in terms of asthma care which resulted in more new asthma cases presenting to the emergency department.
In order to continue to improve on the success already achieved, she subsequently started requesting for improved clinic space and a nurse that could help work in the increasingly busy clinic. Overtime, the hospital has routinely adopted this new asthma management plan as its standard of care.
Both change models start with creating the desire for change in the followers and end with establishing the change to be part of the culture of the organization, the major difference between them is that while Kotter’s model requires everybody to be on board in the change campaign, Lewin acknowledges that in reality it may not always be feasible to have everybody on board and as such one would have to strategize in order to reduce the power of resisting forces and increase the power for the supporting forces. In implementing the change discussed, the leader used transformational and situational leadership theories.
4. Transformational Leadership
Transformational leadership is a type of leadership in which there is a form of interaction between a leader and a follower that yields a connection which causes both the leader and follower to have higher motivations and values [12] . This
Figure 1. Emergency room and scheduled clinic asthma cases 2015 to 2017.
type of leadership is attentive to the needs of the follower. It is the type of leadership that transforms people as it assesses the inner ambition of people and drives them into desiring to attain higher achievements and motivation for the good of others [13] . The Consultant had a vision of the change she wanted to impact and in the process of trying to achieve that goal she had to communicate to the other members of her health team. By doing a clinical teaching, she was not only able to give a vision of the goal her unit was planning to achieve, she also met the training needs of the junior doctors. And by keeping records of the unit’s activity she was able to have a factual evidence of the success and positive impact of the change process which motivated the junior doctors to aspire to do more.
Advocates of transformational leadership favor it for a number of reasons. To start with, it is a type of leadership that offers a clear organizational direction. Because in transformational leadership theory, the leader has a clear vision which he communicates to the followers and motivates the followers in a way that they have confidence in their ability to achieve this vision [12] . This clear sense of direction gives the followers a sense of identity as they put in their efforts towards achieving this goal; it also boosts their confidence and gives them a sense of self efficiency [14] . Secondly, it is a leadership that develops the capacity of its followers. Due to the fact that in transformational leadership, the leader raises the aspirations of the followers, this drives the willingness of the followers to improve the status quo for the benefit of an institution. As a result, the followers identify with the vision of the leader which makes them to own the vision and to put in efforts beyond the basic in order to achieve that goal. Here, there is an emphasis on intrinsic follower development and motivation [15] as the needs of the followers are taken into account in drawing the road map to achieving the organizational goal. This means that the follower in the organizational goals is able to identify with the process and has a deep sense of commitment because he sees the vision as part of a personal development plan. Thirdly, transformational leadership produces better quality leaders because it is a type of leadership in which the leaders experience personal development and training during the process. In transformational leadership the interaction between the leader and the follower creates a higher sense of motivation and moral values that not only develops the follower but also positively transforms the leader [12] . Furthermore, transformational leadership has a social moral benefit that impacts on the society. In transformational leadership, the leaders are strong role models for the beliefs and values that they want their followers to adopt. These leaders have a significant influence on what their followers identify with, are inspired by, trust and have an emotional connection to [16] [17] [18] . A transformation leader can shape the ideology of a whole society resulting in a wide spread movement.
On the other hand, transformational leadership has some limitations and draw backs. For instance, it has the tendency to create one powerful personality as against one strong institution. This is because in transformational leadership the leader has the tendency to be described as a visionary who has this powerful influence to drive people to achieve a common goal [12] . In the context of healthcare management where team work, shared leadership and rotation of leadership roles help efficient patient management, having one big personality with “the vision” to influence the follower could be counterproductive [19] . Also in the social sector the strong sense of loyalty, affection and intense obedience to the ideology of the leader can be detrimental if the vision is antisocial by being self-consumed, power oriented and exploitative like the case of Adolf Hitler and Saddam Hussein [12] . Although some may argue that the emphasis on good morals and values for the good of all would separate an authentic transformation leader from pseudo transformational leaders [15] [17] who have personalized selfish interest, yet, the fact is that they both have the same influence on follower using similar strategies.
Furthermore, transformational leadership can lead to a more tedious and possibly unpredictable road map to achieving a leader’s goal. Because transformational leadership process depends upon meeting the needs of the followers who play a central role in the process of transformational leadership. It also depends on their predisposition and their ability to be motivated to exceed expectations [20] .
5. Situational Leadership
Another leadership theory used in achieving the change described earlier is situational leadership. This is the type of leadership that adapts different styles to various situations as the need arises but with a common objective of achieving a set goal. The various styles are created by use of directive and supportive dimensions in various proportions based on the follower’s need as evaluated by the leader [21] . In the implementation of the change processes in asthma management, various situations required different styles of leadership in order to effect that change.
Situational leadership has many strengths that make it a desirable leadership style, to start with, it is very practical and its practicality makes it easy to comprehend and implement. It recognizes two vital qualities needed in a follower in order to accomplish a task and that is commitment and competence and it goes ahead to prescribe to the leader what leadership style to use for each follower based on their level of development. By the leader’s use of directive and supportive behaviors in various proportions, four leadership styles can be adopted for any follower’s developmental stage thus enabling the leader to delegate, support, coach or direct [22] . The directive behavior clarifies what the goal is, how it is to be achieved, and sets time line for evaluation of that goal while the supportive behavior helps the follower to feel comfortable with themselves and in their working environment in order to accomplish the said task [21] . It is also an accommodating type of leadership style in that it adapts to the follower’s level of development [22] . For instance, followers with the lowest level of development is D1 and they are described as having low competence and high commitment while the highest level, D4, have high commitment and high competence, D2 and D3 are in between. In situational leadership, the leader objectively assesses your developmental level and prescribes what leadership style he needs to work with you in order to achieve the set goals. This makes situational leadership an all-inclusive type of leadership which recognizes the variability in the capability of different followers and adjusts to give them a style that suits them. In other words, it does not make room for rejecting or writing off a follower rather it makes the leaders take ownership of the adjustment in leadership style in order see the follower succeed [23] . A situational leader therefore should be able to identify the competency and commitment level of a follower [24] . In the health sector where lot of training is done, situational leadership can be a good approach for training health workers [25] . This is because when trainees are new, they are usually very eager to learn but are yet to achieve the necessary competence and skill so a directing approach would be recommended at that stage. Along the line however, they gain more knowledge and begin to understand the magnitude of what is required of them which may make them to begin to lose confidence, at this stage, they would require a supportive leadership style. Later in their training they become more experienced, confident and motivated and would then require delegation leadership style [26] .
In addition, situational leadership is a good model for training leaders and has been known to be used for training in various organizations [21] . This is probably because of its prescriptive approach in which it tells the leader the right and wrong approaches in various contexts. Also, the flexibility of situational leadership makes it a good approach in change management, this is because at the implementation of a change process in an organization a lot of workers would be at the learning stage and based on their interest and predisposition they could have varying levels of commitment. The leader in this situation would need to be applying the various styles of situation leadership, to different trainers and at different times in the change process till the whole team is at the required level as was required in the change discussed above.
Critics of situational leadership however have argued that the weighting of the developmental level of the subordinates is ambiguous as well as the components of the factors that constitute development [23] [27] . Also situational leadership seems to be lacking in addressing how group leadership should be handled this is because groups go through various developmental levels and the prescribed leadership style for each group is meant to be adequate for the overall developmental level of the group [28] . However, the individuals in the group would be at different stages of development and situational leadership is not really clear on how the leader should relate with individuals within the group with regards to the prescribed leadership style if it should be based on their individual developmental level or on the group developmental level [21] .
6. Conclusion
In order to successfully implement the change in asthma care, the leader had to use a strategic change management model and more than one leadership ship style. Besides the two leadership styles discussed above other styles include transactional leadership, visionary leadership, authentic leadership, ethical leadership and medical leadership also known as shared leadership [19] . The choice of the type of leadership style to implement is any situation is a combination of the goal to be achieved, the factors that are necessary for its successful completion, the leader’s preference and behavioral attributes.
Conflicts of Interest
The author declares no conflicts of interest regarding the publication of this paper.
Cite this paper
Onubogu, U. (2019) How to Implement Change in Asthma Management in a Developing Country. Open Journal of Respiratory Diseases, 9, 26-35. https://doi.org/10.4236/ojrd.2019.91003
References
- 1. Girish, D.S. (2017) Paediatric Asthma Treatment and Management. https://emedicine.medscape.com/article/1000997-treatme
- 2. Pavord, I.D., Mathieson, N., Scowcroft, A., Pedersini, R., Isherwood, G. and Price, D. (2017) The Impact of Poor Asthma Control among Asthma Patients Treated with Inhaled Corticosteroids plus Long-Acting β2-Agonists in the United Kingdom: A Cross-Sectional Analysis. NPJ Primary Care Respiratory Medicine, 27, 17.
- 3. Zhong, N., Lin, J., Zheng, J., Lai, K., Xie, C., Tang, K., et al. (2016) Uncontrolled Asthma and Its Risk Factors in Adult Chinese Asthma Patients. Therapeutic Advances in Respiratory Disease, 10, 507-517.
- 4. Berwick, D. (2013) A Promise to Learn—A Commitment to Act. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/226703/Berwick_Report.pdf
- 5. NICE (2018) How to Change Practice. Barriers to Change. https://www.nice.org.uk/media/default/about/what-we-do/into-practice/support-for-service-improvement-and-audit/how-to-change-practice-barriers-to-change.pdf
- 6. Sherring, S. (2012) Nursing Leadership within the NHS: An Evolutionary Perspective. British Journal of Nursing, 21, 491-494. https://doi.org/10.12968/bjon.2012.21.8.491
- 7. Lewin, K. (1951) Field Theory in Social Science: Selected Theoretical Papers. American Journal of Sociology, 57, 86-87.
- 8. Hussain, S.T., Lei, S., Akram, T., Haider, M.J., Hussain, S.H. and Ali, M. (2016) Kurt Lewin’s Change Model: A Critical Review of the Role of Leadership and Employee Involvement in Organizational Change. Journal of Innovation & Knowledge, 3, 123-127.
- 9. Robert, T. (2018) Kotter’s Eight Step Leading Change Model. https://managementisajourney.com/summary-of-kotters-eight-step-leading-change-model
- 10. Kotter, J.P. and Rathgeber, H. (2006) Our Iceberg Is Melting: Changing and Succeeding under Any Conditions. Macmillan, London.
- 11. GINA (2016) Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma.http://ginasthma.org/wp-content/uploads/2016/04/GINA-2016-main-report_tracked.pdf
- 12. Northouse, P.G. (2016) Transformational Leadership. In: Stanley, M., Ed., Leadership: Theory and Practice, 7th Edition, Sage, Thousand Oaks, CA, 161-191.
- 13. Avolio, B.J. (1999) Full Leadership Development: Building the Vital Forces in Organizations. Sage, Thousand Oaks, CA.
- 14. Shamir, B., House, R.J. and Arthur, M.B. (1993) The Motivational Effects of Charismatic Leadership: A Self-Concept Based Theory. Organization Science, 4, 577-594.
- 15. Bass, B.M. and Riggio, R.E. (2014) Transformational Leadership. 2nd Edition, Routledge, New York.
- 16. Burns, J.M. (1978) Leadership. Harper & Row, New York.
- 17. Howell, J.M. and Avolio, B.J. (1992) The Ethics of Charismatic Leadership: Submission or Liberation? AMP, 6, 43-54.
- 18. House, R.J. (1976) Theory of Charismatic Leadership. Working Paper Series 76-06. https://files.eric.ed.gov/fulltext/ED133827.pdf
- 19. NHS and AMRC (2009) Shared Leadership: Underpinning of the MLCF. https://www.fmlm.ac.uk/resources/shared-leadership-underpinning-of-the-mlcf
- 20. Bryman, A. (1992) Charisma and Leadership in Organization. Sage Publications, London.
- 21. Northouse, P.G. (2013) Situational Leadership. Leadership: Theory and Practice. 6th Edition, Sage Publications Ltd., New York, 99-136.
- 22. Blanchard, K., Zigarmi, P. and Zigarmi, D. (1999) Leadership and the One Minute Manager: Increasing Effectiveness through Situational Leadership. 2nd Edition, William Morrow Company, Chicago.
- 23. Graeff, C.L. (1983) The Situational Leadership Theory: A Critical View. AMR, 8, 285-291.
- 24. Lynch, B.M., McCormack, B. and McCance, T. (2011) Development of a Model of Situational Leadership in Residential Care for Older People. Journal of Nursing Management, 19, 1058-1069.
- 25. Giltinane, C.L. (2013) Leadership Styles and Theories. Nursing Standard, 27, 35-39. https://doi.org/10.7748/ns2013.06.27.41.35.e7565
- 26. Grimm, J.W. (2010) Effective Leadership: Making the Difference. Journal of Emergency Nursing, 36, 74-77. https://doi.org/10.1016/j.jen.2008.07.012
- 27. Yukl, G.A. (2013) Leadership in Organizations. 8th Edition, Prentice Hall, Upper Saddle River.
- 28. Carew, D.K., Parisi-Carew, E. and Blanchard, K.H. (1990) Group Development and Situational Leadership: A Model for Managing Groups. Training & Development Journal, 40, 46-50.