International Journal of Clinical Medicine
Vol.4 No.7A2(2013), Article ID:34613,3 pages DOI:10.4236/ijcm.2013.47A2003
Medium-Term Follow-Up of Children with Unilateral Non or Poorly Functioning Kidney: A Single-Center Experience
![]()
1Pediatric Urology Unit, Schneider Children’s Medical Center of Israel, Petah Tiqwa, Israel; 2Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel.
Email: *azikhof@gmail.com
Copyright © 2013 Azik Hoffman et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received May 8th, 2013; revised June 10th, 2013; accepted June 25th, 2013
Keywords: Nonfunctioning Kidney; Conservative Treatment
ABSTRACT
Purpose: The aim of the study was to assess the safety of conservative management of nonfunctioning kidney in children. Materials and Methods: The study group consisted of 29 children with a unilateral or poorly functioning kidney who were followed at the outpatient clinic of the Urology Unit of a tertiary pediatric medical center for at least two years. Pain, hypertension, urinary tract infection, and renal calculi were assessed regularly during follow-up. Results: Mean duration of follow-up was 62 months. The main causes for non-functioning kidney were high grade vesicoureteral reflux (55%) and ureteropelvic junction obstruction (34%). Urinary tract infection (24%) occurred mostly during the first 18 months of follow up. UTI was observed in all children who had bilateral vesicoureteral reflux or an ectopic ureter. None of the children developed pain, hypertension or renal calculi during follow-up period. Conclusions: In children, preserving a nonfunctioning kidney due to causes other than vesicoureteral reflux does not increase the risk of complications on medium term follow up. Those with non-functioning kidney due to high grade vesicoureteral reflux should be offered nephrectomy to decrease the risk of UTI.
1. Introduction
The decision to remove a nonfunctioning or poorly functioning kidney in asymptomatic children is based on the assumption of a high risk of future complications. However, solid long term data on rates of pain, urinary tract infection (UTI), hypertension, and renal calculi in these patients are lacking. Furthermore, parents are often reluctant to remove a nonor poorly functioning kidney or moiety if the child is asymptomatic and is developing normally.
This study aims to assess the safety of conservative management of a nonfunctioning kidney in the pediatric population.
2. Materials and Methods
Our cohort included 29 children with a nonfunctioning or poorly functioning kidney or a non functioning upper or lower pole moiety who were followed at the outpatient clinic of the Urology Unit of a tertiary pediatric medical center. Children not operated on because of parental refusal were offered conservative management by medical follow up once every 3 to 6 months, and those who maintained regular follow up for at least two years were included in this study. Exclusion criteria included prior oncologic surgery and renal transplantation.
Follow up protocol included physical examination, blood pressure measurement, and periodic renal sonography to assess hydronephrosis or nephrolithiasis.
Renal function was determined by analyzing the parenchymal-phase image after the administration of a weight-adjusted dose of dimercaptosuccinic acid (DMSA) labeled with technetium-99 m.
Febrile UTI was defined as combined findings of temperature greater than 38.5˚C and positive urine culture: greater than 100,000 colony forming units per ml (CFU/ml) of a single pathogen by midstream collection (older children) or greater than 1000 CFU/ml by urinary catheter. Hypertension was defined according to blood pressure nomograms [1]. Pain, urinary tract infection, hypertension, and renal calculi during the follow-up period were assessed according to medical chart documentations.
3. Results
Mean duration of follow-up was 62  41 months. Child characteristics are summarized in Table 1. Residual renal function was 10.3%
41 months. Child characteristics are summarized in Table 1. Residual renal function was 10.3%  7.4%. The most common causes of renal dysfunction (Table 2) were vesicoureteral reflux and ureteropelvic junction obstruction. The rates of UTI are illustrated in Figure 1. Seven children (24.1%) had a documented episode of UTI, mostly during the first 18 months of follow up. All children with bilateral vesicoureteral reflux or an ectopic ureter had documented UTI during follow up. None of the children suffered hypertension or renal calculi.
7.4%. The most common causes of renal dysfunction (Table 2) were vesicoureteral reflux and ureteropelvic junction obstruction. The rates of UTI are illustrated in Figure 1. Seven children (24.1%) had a documented episode of UTI, mostly during the first 18 months of follow up. All children with bilateral vesicoureteral reflux or an ectopic ureter had documented UTI during follow up. None of the children suffered hypertension or renal calculi.
4. Discussion
Current literature yields almost no data on the natural history of nonfunctioning or poorly functioning kidneys treated conservatively. The largest available study, Hammad et al. [2], examined etiology rather than the
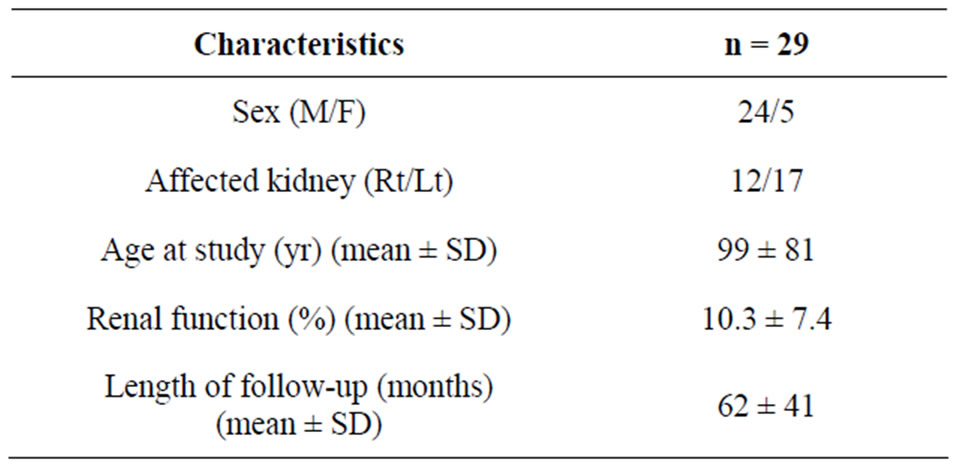
Table 1. Children characteristics.
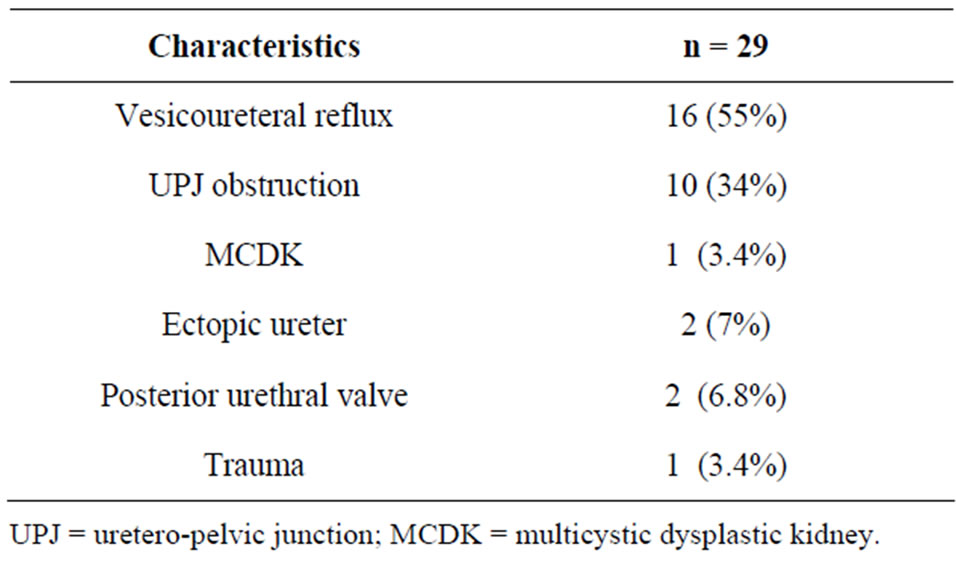
Table 2. Causes of renal dysfunction.
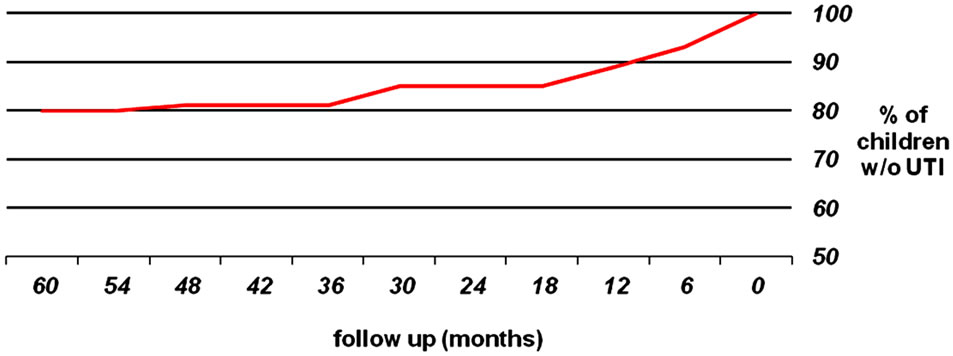
Figure 1. UTI probability during follow up period.
factors affecting the decision to perform nephrectomy. In that study the most common nonmalignant indications for nephrectomy were MCDK (31%), versicoureteral reflux (17%), and ureteropelvic junction obstruction (7%). Heminephrectomy was generally performed for a nonfunctioning moiety of duplicated systems.
A more recent review by Cambio et al. [3] showed that although nephrectomy had been common practice for MCDK up to three decades ago [4], the risk of hypertension in affected patients was not increased relative to the general population, the risk of Wilm’s tumor was less than 0.05%, and UTI was more often associated with vesicoureteral reflux than with dysplastic kidney. These findings led to the suggestion that conservative management and close follow up may be the preferred approach to asymptomatic MCDK [5]. As a result, there are probably many more children today with MCDK being followed by nephrologists without referral to a pediatric urologist.
Overall, the most common cause of a nonfunctioning or poorly functioning kidney in the present study was reflux nephropathy. UTI developed in 24% of the children during the follow up period. Hammad et al. [2] reported an even higher rate of children with reflux nephropathy, 66%. Therefore, we suggest that nephrectomy should be considered in asymptomatic children with high-grade reflux in a non-functioning kidney, and children with asymptomatic upper or lower nonfunctioning moiety of a duplicated kidney should be considered candidates for heminephrectomy if diagnosed with a high grade reflux to this moiety.
Ureteropelvic junction obstruction was the second most common cause of nonfunctioning kidney in our study. All of those children remained asymptomatic. Nevertheless, previous studies reported increased rate of UTI in children with severe upper tract obstruction, although they did not focus on nonor poorly functioning kidneys [6,7]. Given the small number of children with this complication in our study (n = 11) we are unable to conclude as to the optimal management approach in such children.
Of note, none of the children developed hypertension or renal calculi, and the number of children with an asymptomatic nonfunctioning kidney of other etiology was too small to draw conclusions regarding the treatment approach.
5. Conclusion
In the pediatric population, preserving a nonfunctioning kidney due to causes other than vesicoureteral reflux does not increase the risk of complications on medium term follow up. Nephrectomy or heminephrectomy may be considered in asymptomatic nonfunctioning kidneys or moieties with high grade reflux. The approach to other nonmalignant etiologies may be conservative, although a larger prospective study is needed to elucidate this issue.
REFERENCES
- B. Rosner, R. J. Prineas, J. M. Loggie and S. R. Daniels, “Blood Pressure Nomograms for Children and Adolescents, by Height, Sex, and Age, in the United States,” Journal of Pediatrics, Vol. 123, No. 6, 1993, pp. 871-886. doi:10.1016/S0022-3476(05)80382-8
- F. T. Hammad and V. Adhyay, “Indications for Nephrectomy in Children: What Has Changed?” Journal of Pediatric Urology, Vol. 2, No. 5, 2006, pp. 430-435. doi:10.1016/j.jpurol.2005.09.009
- A. J. Cambio, C. P. Evans and E. A. Kurzrock, “NonSurgical Management of Multicystic Dysplastic Kidney,” British Journal of Urology International, Vol. 101, No. 7, 2008, pp. 804-808. doi:10.1111/j.1464-410X.2007.07328.x
- A. C. Gordon, D. F. Thomas, R. J. Arthur and H. C. Irving, “Multicystic Dysplastic Kidney: Is Nephrectomy Still Appropriate?” Journal of Urology, Vol. 140, No. 5, 1988, pp. 1231-1234.
- E. Kuwertz-Broeking, O. A. Brinkmann, et al., “Unilateral Multicystic Dysplastic Kidney: Experience in Children,” British Journal of Urology International, Vol. 93, No. 3, 2004, pp. 388-392. doi:10.1111/j.1464-410X.2003.04623.x
- C. C. Roth, J. M. Hubanks, B. C. Bright, et al., “Occurrence of Urinary Tract Infection in Children with Significant Upper Urinary Tract Obstruction,” Journal of Urology, Vol. 73, No. 1, 2009, pp. 74-78. doi:10.1016/j.urology.2008.05.021
- Y. H. Shim, J. W. Lee and S. J. Lee, “The Risk Factors of Recurrent Urinary Tract Infection in Infants with Normal Urinary Systems,” Pediatric Nephrology, Vol. 24, No. 2, 2009, pp. 309-312. doi:10.1007/s00467-008-1001-0
NOTES
*Corresponding author.

