Open Journal of Modern Neurosurgery
Vol.07 No.02(2017), Article ID:75478,6 pages
10.4236/ojmn.2017.72004
Post-Traumatic Spinal Meningioma: A Case Report and Review of the Literature
Mahmoud M. Taha
Department of Neurosurgery, Faculty of Medicine, Zagazig University, Zagazig, Egypt

Copyright © 2017 by author and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: February 2, 2017; Accepted: April 16, 2017; Published: April 19, 2017
ABSTRACT
Post-traumatic meningioma is a matter of controversy with many reported cases of cranial post-traumatic meningioma and rare cases for such pathology in human spine. The author reports a 61-year-old woman who had post-trau- matic spinal meningioma at the site of old traumatic fracture for 26 year after her initial trauma. The patient treated successfully with microsurgical resection and posterior fusion with improvement of here recent weakness. The author reviews the literatures for similar cases as well as reviews the controversies regarding the development of post-traumatic meningiomas.
Keywords:
Meningioma, Lumbar Spine, Trauma

1. Introduction
Meningiomas are slowly growing benign tumor commonly arising in the intracranial compartment more than the spinal canal [1] . They are located mostly intradural and generally respecting the pial layer of the spinal cord [2] . Spinal meningiomas are more commonly diagnosed in elderly patients, and lead to symptoms only after reaching a distinct size due to spinal cord compression [1] . With the advancement of neuroimaging investigation and microsurgical techniques, these tumors can be excised with low morbidity and mortality [1] [3] . Viral infections, exogenous or endogenous sex hormones, ionizing radiation and trauma may be associated with development of meningiomas [4] [5] . Posttraumatic intracranial meningiomas were reported before in several case reports and large series studies, while posttraumatic spinal meningiomas were extremely rare [6] [7] [8] [9] [10] . The author in this paper presents a case report of meningioma that developed at the site of previous spinal trauma with review of the literatures for similar cases.
2. Case Report
A 61-year-old female patient was with history of spinal trauma in 26 year ago. Patient fall down from height and had a traumatic L1 fracture. Patient was managed conservatively at that time as she refused surgical intervention and had no neurological deficit. Patient experienced frequent attacks of low back pain and rarely sciatic pain that was treated with analgesia. 6 months ago, the patient had a progressive heaviness in both lower limbs with urinary incontinence and visited the outpatient clinic. On examination, the patient was paraparetic with motor power grade II or III below L1. Patient had hypotheisa below L1 with diminished knee and ankle reflexes. MRI lumbar and dorsal spine showed the post-traumatic L1 fracture with a new large intra-dural mass most probably meningioma or schwnoma as shown in Figure 1. Patient operated with posterior lumbar approach including posterior L1 and D12 laminectomy. Total standard microscopic excision of the intra-dural soft tissue mass with moderate vascularity was performed successfully. A posterior D11, D12 and L2 trans-pedicular screw fusion was performed at the end of the procedure. Histopathological examination revealed multiple nodules of proliferated meningothelial cells separated by delicate fibrous tissue, with thick walled blood vessels and calcified psammoma bodies together with oval to rounded cells with oval nuclei, occasional nuclear clearing and infrequent mitosis arranges in whorly pattern with rounded calcified psamma bodies. A meningeothelial and psamomatous meningioma was reported as shown in Figure 2. The patient has smooth postoperative course with improvement of her neurological deficit with physiotherapy. 4 months after surgery, the patient was able to ambulate without assistance. On her last follow up after one year of surgery; the patient has no neurological deficit and can ambulate without assistance
3. Discussion
Meningioma is a benign slowly growing tumor arising from the arachnoid cells and frequently located in the intracranial compartment more than the spinal compartment [1] [4] . Spinal meningiomas account for 25% of all spinal cord tu- mors and more commonly located in the thoracic spine [1] [2] . The majority of meningiomas develop spontaneously and a few developed in association with external factors such as viral infections, high and low doses of ionizing radiation, genetic factors, endogenous or exogenous hormones or trauma [5] . The association of trauma to the skull or meninges and the development of meningioma were first reported by Cushing in 1938 [11] . Since then, several case reports and large studies investigated this relationship between skull trauma and development of intracranial meningioma. However; the subject remains conteroversial. Annegers et al., in their large and long term study of 2953 patients with head injury reported 3 meningiomas developed 5, 12, and 26 years respectively after trauma [6] . The authors demonstrated that the results of their large series cannot absolutely refute the possibility that head trauma predisposes to brain tumor, but the individual risk is very small and the evidence does not support such as-
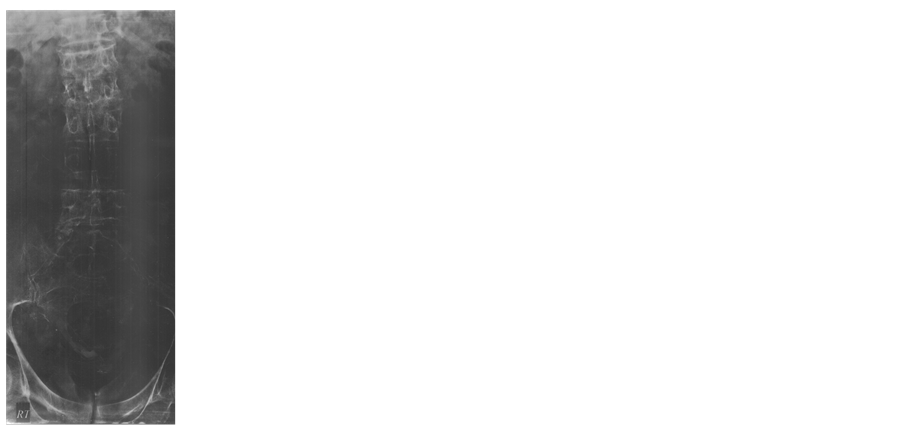
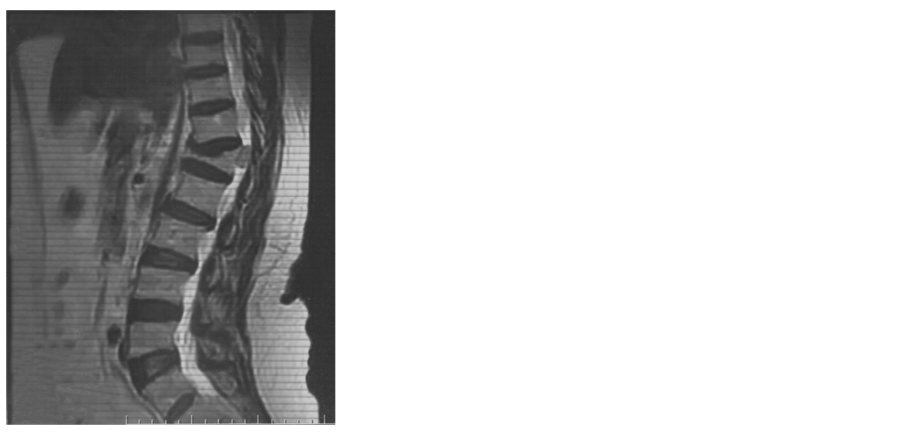
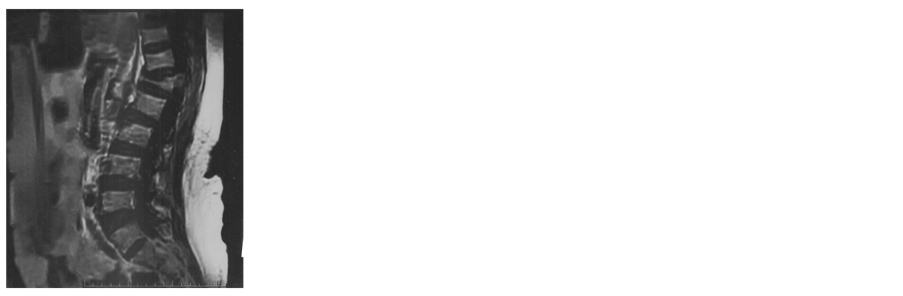
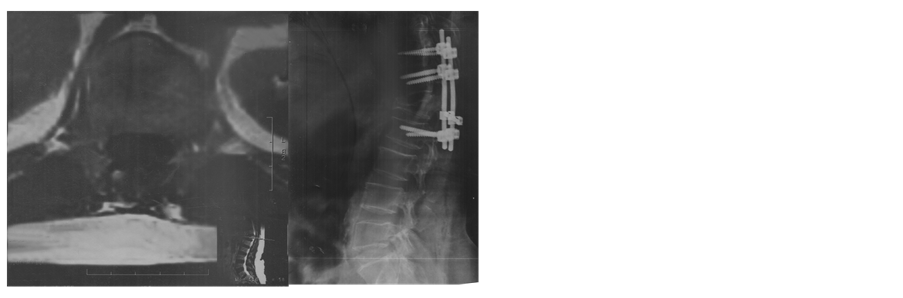
Figure 1. (a) X ray lateral view shows L1 fracture; (b) X ray anteroposterior view shows L1fracture; (c) MRI lumbosacral spine T2 weighted image sagittal view shows the L1 fracture and the intradural mass; (d) MRI lumbosacral spine T1 weighted image sagittal view shows the L1 fracture and the intradural mass; (e) MRI Dorsal spine T2 weighted image sagittal view shows the L1 fracture and the intradural mass; (f) MRI lumbosacral spine T2 weighted image axial view shows the intradural mass compressing the cord; (g) X ray lateral view shows the pedicular screws; (h) X ray anteroposterior view shows the postoperative fusion.
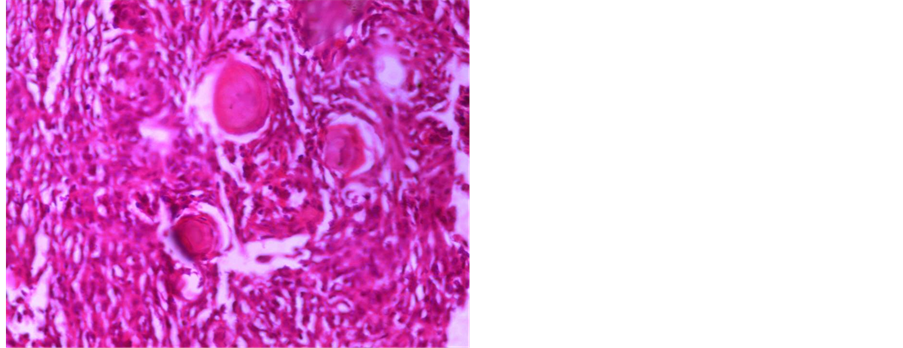
Figure 2. (a) Photomicrograph showing multiple nodules of proliferated meningothelial cells separated by delicate fi- brous tissue, with thick walled blood vessels and calcified psammoma bodies, H & E × 40 (b) and (c) Photomicr- graph of meningioma showing oval to rounded cells with oval nuclei, occasional nuclear clearing and infrequent mi- tosis arranges in whorly pattern with rounded calcified psammoma bodies, H & E × 400.
sociation between trauma and the development of intracranial meningioma [4] . Other studies have addressed the epidemiology of intracranial meningioma and considered head trauma as a possible risk factors [12] . Preston-Martin [12] study of 1178 glioma and 330 meningioma cases found that the risk for ever having experienced a head injury was highest for male meningiomas. Among male meningiomas, latency of 15 to 24 years significantly increased risk [12] . Overproliferation of arachnoid cells was linked to the course of wound healing process at the site of old fracture and probable dural laceration [8] . Barnett et al. postulated that chronic inflammation caused by foreign bodies or granuloma formation may lead to meningeal irritation, cellular atypia with subsequent tumor formation [7] .
Spinal meningiomas are slowly growing benign tumors usually presented with unspecific symptoms as local pain which are often misinterpreted [1] [3] . This was the situation in our case where the patient complained of low back pain that was explained on the base of here old fracture spine and the accompanied spondylosis until neurological deficit and gait disturbance which occurred at an advanced stage.
The primary goal of surgery is to achieve complete tumor resection and to avoid additional neurological damage [3] with the advancement of microsurgical procedures this goal can be achieved in majority of cases as in our patient with posttraumatic L1 meningioma. Additional posterior pedicular fusion was added to the standard microsurgical technique to avoid exacerbation of posttraumatic kyphosis after laminectomy.
To best of the author's knowledge, two cases of post-traumatic spinal meningioma were reported before [9] [10] . Holländer et al. reported a 38-year-old female who had a meningioma at the site of traumatic fracture at the T12 level that occurred 19 years previously [9] . Kasantikul and his colleagues described a 61- year-old man with flaccid paraplegia after traumatic T4 fracture 3 years before examination at the emergency room. The patient had sudden cardiorespiratory arrest and died 4 hours after admission to the emergency room. Postmortem examination revealed thinned and sclerotic spinal cord from the T4-6 segments. A gray-white subdural extramedullary tumor, 3 cm in length and 1 cm in diam- eter, the lesion was diagnosed as a transitional meningioma [10] .
The pathology of the reported case in this study was a benign meningioma. This coincides with the reported case of Kasantikul and his colleagues [10] who reported a post-traumatic case of benign spinal meningioma. Both reports were different from post-traumatic meningiomas of the intracranial compartment where the majority of cases were described as atypical or malignant [8] .
4. Conclusion
In summary, this case report and the review of the literatures of similar cases highlight the importance of old trauma as a risk factor for development of meningioma.
Cite this paper
Taha, M.M. (2017) Post-Traumatic Spinal Meningioma: A Case Report and Review of the Literature. Open Journal of Modern Neurosurgery, 7, 34-39. https://doi.org/10.4236/ojmn.2017.72004
References
- 1. Sandalcioglu, I.E., Hunold, A., Müller, O., Bassiouni, H., Stolke, D. and Asgari, S. (2008) Spinal Meningiomas: Critical Review of 131 Surgically Treated Patients. European Spine Journal, 17, 1035-1041.
https://doi.org/10.1007/s00586-008-0685-y - 2. Haegelen, C., Morandi, X., Riffaud, L., Amlashi, S.F.A., Leray, E. and Brassier, G. (2005) Results of Spinal Meningioma Surgery in Patients with Severe Preoperative Neurological Deficit. European Spine Journal, 14, 440-444.
https://doi.org/10.1007/s00586-004-0809-y - 3. Ozkan, N., Dammann, P., Chen, B., Schoemberg, T., Schlamann, M., Sandalcioglu, I.E. and Sure, U. (2013) Operative Strategies in Ventrally and Ventrolaterally Located Spinal Meningiomas and Review of the Literature. Neurosurgical Review, 36, 611-619.
https://doi.org/10.1007/s10143-013-0462-1 - 4. Argyriou, A.A., Polychronopoulos, P., Partheni, M., Konstantinou, D., Papapetropoulos, S. and Chroni, E. (2008) Co-Occurrence of Brain Tumors and Demyelination of the Central Nervous System: Coincidence or Interrelation. European Journal of Cancer Care, 17, 616-618.
- 5. Pacheco Compaña, F.J., Midón Míguez, J., Avellaneda Oviedo, E.M. and Busto Lodeiro, E. (2016) Post-Traumatic Cutaneous Meningioma. Archives of Plastic Surgery, 43, 381-384.
https://doi.org/10.5999/aps.2016.43.4.381 - 6. Annegers, J.F., Laws Jr., E.R., Kurland, L.T. and Grabow, J.D. (1979) Head Trauma and Subsequent Brain Tumors. Neurosurgery, 4, 203-206.
https://doi.org/10.1227/00006123-197903000-00001 - 7. Barnett, G.H., Chou, S.M. and Bay, J.W. (1986) Posttraumatic Intracranial Meningioma: A Case Report and Review of the Literature. Neurosurgery, 18, 75-78.
https://doi.org/10.1227/00006123-198601000-00012 - 8. François, P., N’dri, D., Bergemer-Fouquet, A.M., Ben Ismail, M., Papagiannaki, C., Cottier, J.P. and Jan, M. (2010) Post-Traumatic Meningioma: Three Case Reports of This Rare Condition and a Review of the Literature. Acta Neurochirurgica, 152, 1755-1760.
https://doi.org/10.1007/s00701-010-0730-6 - 9. Holländer, H., Kosmaoglou, V. and Sturm, W. (1971) Intraspinal Meningioma Following Vertebral Fracture. Zentralblatt fur Neurochirurgie, 32, 179-185.
- 10. Kasantikul, V., Charuchaikul, S. and Shuangshoti, S. (1991) Extramedullary Subdural Meningioma after Trauma. Neurosurgery, 29, 930-931.
https://doi.org/10.1227/00006123-199112000-00025 - 11. Cushing, H. and Eisenhardt, L. (1938) Meningiomas: Their Classification, Regional Behavior, Life History and Surgical Results. Archives of Neurology and Psychiatry, 41, 657-658.
https://doi.org/10.1097/00000441-193811000-00052 - 12. Preston-Martin, S., Pogoda, J.M., Schlehofer, B., Blettner, M., Howe, G.R., Ryan, P., Menegoz, F., Giles, G.G., Rodvall, Y., Choi, N.W., Little, J. and Arslan, A. (1998) An International Case-Control Study of Adult Glioma and Meningioma: The Role of Head Trauma. International Journal of Epidemiology, 27, 579-586.
https://doi.org/10.1093/ije/27.4.579