Open Journal of Blood Diseases
Vol.3 No.2(2013), Article ID:33614,5 pages DOI:10.4236/ojbd.2013.32015
Prevalence and Distribution of ABO and Rh-D Antigens along with Its Subgroups & Rare Types in Greater Gwalior Region
![]()
1Department of Pathology, Gajra Raja Medical College, Gwalior, India; 2Emergency Blood Bank, Gwalior, India.
Email: *dr_dharmesh_sharma@yahoo.com
Copyright © 2013 Dharmesh Chandra Sharma et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received December 22nd, 2012; revised January 31st, 2013; accepted February 9th, 2013
Keywords: ABO; Rh-D; ABO Phenotype
ABSTRACT
Among a total of 29 blood group systems and over 600 different blood group antigens discovered so far, ABO and Rhesus are the most important blood group systems. The most significance rhesus antigen is Rh-D because of its immunogenicity. The sound knowledge of ABO and Rh-D antigens and its distribution in population is essential for the effective management of blood transfusion services, in population genetic studies, in resolving medico-legal issues and more importantly in compatibility test in blood transfusion practice. Study is aimed to provide data on ABO and Rh-D distribution in Gwalior region (Madhya Pradesh) and its comparison with related studies in India and abroad. Total 90,000 samples in 4 years from January 2004 to December 2007 were grouped for ABO, Rh-D and their subgroups at Blood Bank of Gajra Raja Medical College, along with Emergency Blood Bank, Gwalior, Madhya Pradesh, India. Blood group distribution among these samples showed phenotypes A, B, AB and O as 22.7%, 37.5%, 9% and 30.8% respectively. A2 and A2B were 8.0% and 8.6% respectively. The Rh-D negative phenotype was found 8.9% and DU variants/weaker D was 0.036% among the sample tested. In cord blood samples, the incidence of A2 and A2B were 18.6% and 20.2% respectively.
1. Introduction
Among a total of 29 blood group systems and over 600 different blood group antigens discovered so far, ABO and Rhesus are the most important blood group systems [1]. Landsteiner and his colleagues classified ABO group system into four blood groups (A, B, AB and O) depending on presence or absence of A and B antigens on red cells [2,3].
Group A individuals were further subdivided into A1, A2 and other rare types like A3, A intermediate (int.), Ax, Am, A bantu, A end, Ay, A finland (fin), A el, Ah (Hpartially deficient, non-secretor), and A weak. Blood group of A individual divided into two subgroup A1 and A2 on the basis of strength of the antigen in which former being stronger [4]. Group A red cells which react with both anti-A and Anti-A1 are classified as A1. A1 constituted approximately 80% of entire A blood group population and group A cell which react with anti-A and not agglutinate with anti-A1 are classified as A2, making up of remaining 20% [5]. Subgroup of B are very rare and occur less frequently than subgroup of A and they are B3, Bx, Bm, Bh (H-partially deficient, non-secretor).
The Rh antigen is present in almost 85% of human whites [6]. The original Rh antigen was referred to as D and related ones are C and E; the antithetically related antigens are called c and e [6].
Other blood group systems are Lewis, P, I, MNSs, Kell, Duffy, Kidd and many more. Bombay (oh) phenotype was discovered in 1952 [7]. Para-Bombay subject shows weaker reaction with anti H reagent [8].
Despite the long list of several other blood groups discovered so far, for the safety of blood/blood products transfusion till date [9], the knowledge and distribution of ABO and Rh-D blood group are essential for effective management of blood bank inventory [10] as well as useful in population genetic studies, researching population migration patterns and resolving certain medicolegal issues [9].
A limited study investigated the ABO and Rh-D blood group frequency in Madhya Pradesh (M.P), especially in and around Gwalior region of India. This study was aimed to provide data on ABO and Rh-D blood group distribution with their subtypes and weaker variants in Gwalior and surrounding region and compare their frequency in other parts of India and abroad.
2. Material and Method
Total 90,000 blood samples were grouped for complete ABO and Rh-D grouping along with subgroup panel over 4 years (Jan. 2004 to Dec. 2007). Blood samples were received from blood donor, blood recipient, antenatal OPD, neonates, cord blood and people who came for routine medical checkup at blood bank, Gajra Raja medical college & JAH groups of hospital and emergency blood bank, Gwalior (M.P) India. All entries were double checked by each author.
ABO and Rh-D grouping were carried out by standard tile and tube technique with appropriate positive and negative control. The tile technique was done by using one drop of 5% RBC suspension mixed with 2 drops of appropriate antiserum, rocked gently and looked for agglutination. In tube method, it was done by taking one drop of 5% cell suspension mixed with one drop of antiserum, incubate for 10 minutes at appropriate temperature and centrifuged for one minute at 1500 revolution per minute (rpm) and examined macroscopically and also under microscope for confirmation of agglutination.
Reverse grouping was done by using pooled A and B cells [11]. For complete ABO grouping (forward and reverse) anti A, anti A1, anti B, anti AB, anti H antiserum and A, B, O pooled cells were used.
For Rh typing anti-D (Ro & R1) antiserum were used. For confirmation of blood grouping & Rh-D typing supportive tests like Indirect Coombs Test (ICT), saliva grouping and absorption elution test, were also performed when necessary.
Data on frequency of ABO and Rh-D blood groups were reported in simple percentages.
3. Result
Out of 90,000 blood samples collected, 20,432 (22.7%) were of blood group A, 33,748 (37.5%) of B, 27,719 (30.8%) of O and 8101 (9%) were of blood group AB (Figure 1). Out of 20,432 total cases of group A; 18,798 (92%) were of A1 and 1634 (8%) were subgroup A2, while weaker variant of A like Aint-5 (0.024%), A3-3 (0.014%), Ax-2 (0.009%) were also reported (Table 1).
Amongst 33,748 cases of blood group B, weak B variants were found in 4 (0.011%) and 1 case (0.0029%) of pseudo B was also reported. Out of 8101 cases of blood group AB; 7405 (91.4%) were A1B and 696 (8.6%) were A2B while 3 cases (0.04%) off A3B was also reported (Table 1). Incidence of irregular antibody, anti-A1 was 10% in A2 and 21% in A2B cases, detected by agglutination method.
Out of 90,000 samples, 8980 samples were collected from cord blood/neonates and showed 2103 cases (23.4%) of A blood group, 3322 cases (36.9%) of B, 2754 cases
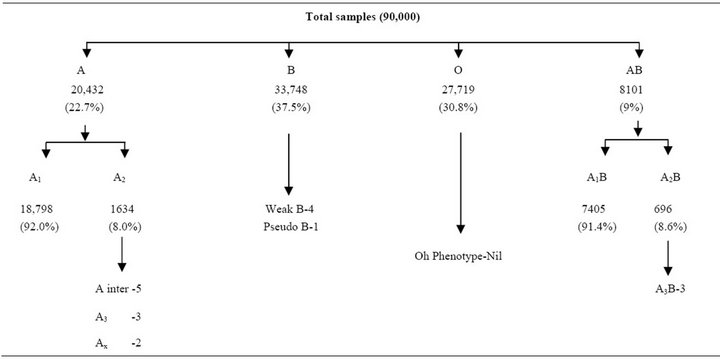
Table 1. Distribution of ABO blood groups and it’s subtypes in total samples.
(30.6%) of O and 801 cases (9.1%) of AB respectively. Incidence of A2 and A2B was 18.6% (392) and 20.2% (162) respectively. Weaker variants of A and AB like A inter-3 (0.14%), A3-3 (0.14%), Ax-1 (0.047%), A3B-1 (0.37%) were also reported (Table 2). Bombay Group (Oh) and its variants were not reported in the present study.
In 90,000 blood samples, incidence of Rh-D negative was 8.9% (8010) and Rh-D positive was 91.1% (81,990) (Figure 2). DU variant/weaker D were observed in 0.036% (34).
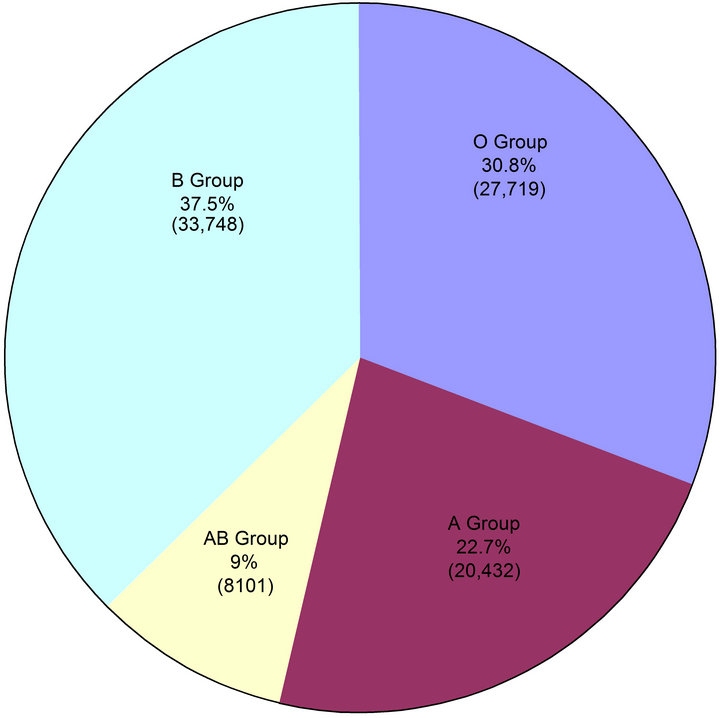
Figure 1. Distribution of various ABO phenotypes among the samples studied (90,000).
Apparently, there was difference in distribution of ABO and Rh-D phenotypes among the samples obtained from different sources.
4. Discussion
Variation in ABO and Rh-D phenotypes are observed widely across races and geographical boundaries [12]. The resultant polymorphism remains important in the population genetic studies, estimating the availabilities of compatible blood, evaluating the possibilities of hemolytic disease of newborn, resolving disputes of paternity/
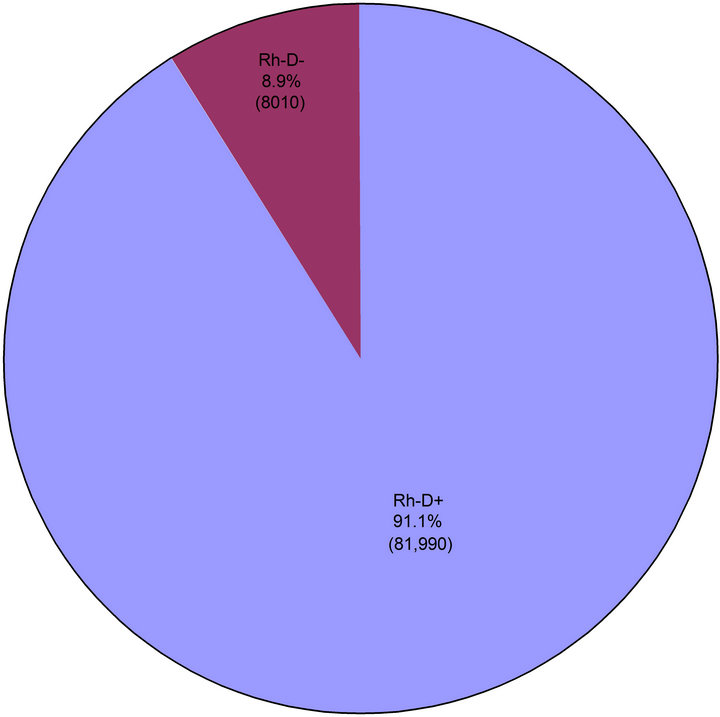
Figure 2. Distribution of various Rh phenotypes among the samples studied (90,000).
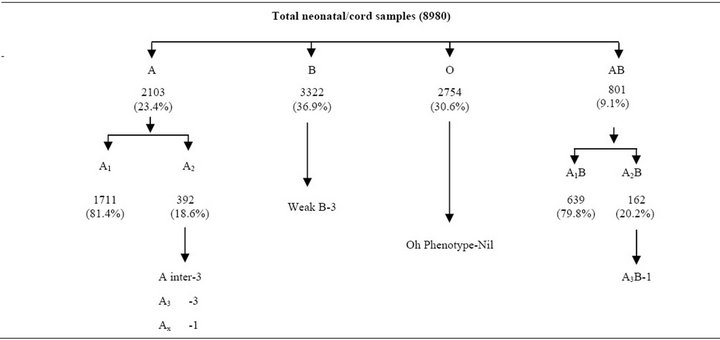
Table 2. Distribution of ABO blood groups and it’s subtypes in neonatal/cord samples.
maternity and for forensic purpose [9,13]. The present study provides information on the status of ABO and Rh-D blood group distribution along with subgroup in Gwalior and surrounding regions.
The most common blood group in present study is B (37.5%) while it is reported O from Bangalore, Karnataka (39.81%) [14] and from South India (38.75%) [15]. In Lodha tribe in Midnapore district, West Bengal it is A [16] and in Northern India (Uttar Pradesh and Punjab) it is B (37.39%) [17]. In white population most common blood group is O (45%) which is closely fallowed by A (41%) [18]. Blood groups differ regionally and ethnically. A, O, B, AB groups are identified in order, 37.1%, 46.7%, 12.2%, 4.1% in USA; 41.8%, 46.6%, 8.6%, 3% in England; 48.2%, 34.2%, 12%, 5.5% in Greece; 39.9%, 35.8%, 16.8%, 7.6% in Bulgaria; 42%, 35.4%, 14.4%, 8.1% in Lebanon [19,20]. In Turkey, however, it is 42.8%, 32.7%, 16.5%, 8% respectively [20]. Frequency of B group is twice in Asians and blacks as in whites.
The most uncommon blood group in our study was AB and it is also observed in other parts of India and abroad. The incidence of A2 and A2B was 8% and 8.6% in our study which is more than studies conducted in India. In south India it is A2—3.01% and A2B—1.43% [15] and in Andhra Pradesh it is less than 4% [21]. Significance of weaker variant like A2, A2B and other subgroups of A and AB is that they may have anti-A1, which gives an incorrect ABO blood typing in reverse grouping and mistyped AB as B and A as O. Substantial qualitative differences between A1 and A2 antigen is also exist. A2 and A2B individuals can not recognize A1 antigens as being part of there own red cells make up and are immunologically stimulated to produce specific Anti-A1 antibody that does not cross react with A2 red cells. A1 and A2 are interchangeable as far as transfusion purposes are concerned. Both types will react with anti-A serum, so a mistake in typing will usually not be made. There is a very small percentage of A2 and large group of A2B people who produce antiA1, which gives an incorrect blood typing result for ABO type, it become critical as failure to detect a weak subgroup of A may result in a patient or donor being mistyped as group AB or B. They may also be mistyped as group O but this is not a serious problem.
Surprisingly incidence of A2 and A2B in neonatal/cord blood sample was 18.6% and 20.2% respectively and it is much more than reported in adults. Most of the group A infants appears to be A2 at birth, because ABO antigens are not fully developed on the red cells at this time. However no difficulty is usually encountered in grouping cord red cells because most of the reagent contains potent anti-A and anti-AB. Most of the cord blood of A2 cells will eventually group as A1 after few months [22]. We have also reported weaker variants of B like weak B and pseudo B.
Subgroups of A and B differentiated by using the following reactions:
1) Cell’s agglutination with antiserum like, anti A, anti A1, anti B, anti AB, and anti H sera;
2) Presence of A, B & H substance in saliva;
3) Adsorption elution studies;
4) Presence or absence of antibodies in the serum.
Incidence of Rh-D negative in present study is 8.9% which is more than observed in other part of India like South India—5.42% [15], Lodha tribe in Midnapore district of West Bengal 0.5% (16), Assam >2% [23], Northern India i.e. U.P and Punjab—8.7% [17]. It is higher in European population (15%) and in Nigeria it is 6% [24].
The discrepancy between our finding and that reported from other area may be attributed to ethnic difference among the population of Gwalior and surrounding region.
5. Conclusion
We concluded that among the various ABO blood groups, group B is the commonest; followed by O and A while AB is the least common type. The prevalence of Rh-D negative is higher than the other studies. The blood groups A2 and A2B are more frequent in cord blood/neonates than in adults.
6. Acknowledgements
The authors are thankful whole-heartedly to Prof. Dr. Shaila Sapre, Head of the Institute: Ex. Dean G. R. Medical College, Gwalior for her close cooperation and unstinted support without which this study would have not been possible. The authors are also thankful to Mrs. Seema Pathak, and Mr. Dharmendra, technicians’ blood bank, J. A. Hospital, Gwalior.
REFERENCES
- S. Worlledge, S. E. Ogiemudia, C. O. Thomas, B. N. Ikoku and L. Luzzuto, “Blood Group Antigens and Antibodies in Nigeria,” Annals of Tropical Medicine and Parasitology, Vol. 68, No. 3, 1994, pp. 249-264.
- K. Landsteiner, “Zur Kenntnis der Anti-Fermentatiren, Lytrschen and Agglutinierenden Wirkungen des Bluteerums und der Lymphe,” Zentralbi Bakteriol, Vol. 27, 1900, pp. 357-362. http://www.genetics.org/content/155/3/995.full
- K. Landsteiner, “Uber Agglutination Serscheinungen Hormalen Menschichen Blutes,” Wien Klin Wschenschr, Vol. 14, 1901, pp. 1132-1134. http://www.genetics.org/content/155/3/995.full
- E. V. Dungern and L. Hirszfield, “Uber Gruppenspezifizche Strukturen des Blutes Ш,” Z Immun Forsch, Vol. 8, 1911, pp. 526-562. http://labmed.ascpjournals.org/content/41/1/53.full.pdf
- Blood Group A Suptypes, “The Owen Foundation,” 2008.
- A. Pourazar, “Red Cell Antigens: Structure and Function,” Asian Journal of Transfusion Sciences, Vol. 1, No. 1, 2007, pp. 24-32. doi:10.4103/0973-6247.28069
- Y. M. Bhende, C. K. Deshpande, H. M. Bhatia, R. Sanger, R. R. Race, W. T. Morgan, et al., “A New Blood Group Character Related to the ABO System,” Lancet, Vol. 1, No. 6714, 1952, pp. 903-904.
- H. M. Batia and M. S. Sathe, “Incidence of Mumbai (oh) Phenotype and Weaker Variants of A and B Antigents in Mumbai (India),” Vox Sanguinis, Vol. 27, No. 6, 1974, pp. 524-532. doi:10.1111/j.1423-0410.1974.tb02450.x
- L. Calhoun and L. D. Petz, “Erythrocyte Antigens,” In: E. Bentler, M. A. Lichman, B. S. Collar, T. J. Kipps and U. Selisohn, Eds., Williums Haematology, 6th Edition, McGraw Hill, Inc., New York, 2001, pp. 1849-1857.
- M. E. Enosolease and G. N. Bazuaye, “Distribution of ABO and Rh-D Blood Group in the Benin Area of NigerDelta: Implication for Regional Blood Transfusion,” Asian Journal of Transfusion Sciences, Vol. 2, No. 1, 2008, pp. 3-5.
- J. V. Dacie and S. M. Lewis, “Practical Haematology,” In: S. M. Lewis, B. J. Bain and I. Bates, Eds., 9th Edition, Churchill Livingstone, Harcourt Publishers Limited, London, 2001, pp. 444-451.
- “Racial and Ethnic Distribution of ABO Blood Types bloodbook.com, Blood information for life,” 2006. http://www.bloodbook.com
- H. F. Polesky, “Blood Group, Human Leukocytes Antigens and DNA Polymorphism in Parenting Testing,” In: J. B. Henry, Ed., Clinical Diagnosis and Management by Laboratory Methods, 19th Edition, WB Saunders, Philadelphelphia, 1996, pp. 1413-1426.
- S. Periyavan, S. K. Sangeetha, P. Marimuthu, B. K. Manjunath and D. M. Seema, “Distribution of ABO and Rhesus-D Blood Groups in and around Bangalore,” Transfusion Science, Vol. 4, No. 1, 2010, p. 41.
- P. K. Das, S. C. Nair, V. K. Harris, D. Rose, J. J. Mammen, Y. N. Bose and A. Sudarsanam, “Distribution of ABO and Rh-D Blood Groups among Blood Donors in a Tertiary Care Centre in South India,” Tropical Doctor, Vol. 31, No. 1, 2001, pp. 47-48.
- U. K. Datta, S. Mondal and S. Mukherjee, “A Study of the Distribution of ABO and Rh(D) Blood Groups amongst Lodha Tribe in Midnapore District of West Bengal,” Journal of the Indian Medical Association, Vol. 95, No. 9, 1997, pp. 497-506.
- A. Nanu and R. M. Thapliyal, “Blood Group Gene Frequency in a Selected North Indian Population,” Indian Journal of Medical Research, Vol. 106, 1997, pp. 242- 246.
- A. E. Mourant, A. C. Kopec and K. Domane-Wska-Sobezak, “The Distribution of the Human Blood Groups and Other Polymorphisms,” Oxford University Press, London, 1976, pp. 1-138.
- S. Gezer, N. Akgün, A. Akɪn and A. Işɪklɪ, “Frequency of ABO Blood Groups in Eskişehir,” Çocuk Sağɪɪlğɪ ve Hastalɪklan Dergisi, Vol. 30, 1997, pp. 227-231. http://www.uhod.org/summary_en.php3?id=402
- C. Yakɪncɪ, Y. Durmaz and Ş. S ve ark, “Malatya Yöresinde ABO ve Rh Kan Gruplannɪn Dağɪlɪmɪ,” Turgut Özal Tɪp Merkezi Dergisi, Vol. 2, 1995, pp. 277-279.
- J. M. Naidu and P. Veerraju, “Blood Groups among Brahmin and Kamma Caste Populations of Coastal Andhra Pradesh,” American Journal of Physical Anthropology, Vol. 58, No. 2, 1982, pp. 197-199. doi:10.1002/ajpa.1330580212
- M. Dense, “Harmening,” Test Book on Modern Blood Banking and Transfusion Practices, 3rd Edition, Jaypee Brothers Medical Publishers LTD, New Delhi, p. 95.
- T. Shyamacharan Singh and M. N. Phookan, “A Note on the Frequency Distributio of ABO and Rhesus Blood Groups in Four Thai Populations of Assam, India and Their Position among the Mangoloide of This Region,” Anthropologischer Anzeiger, Vol. 48, No. 1, 1990, pp. 29-35.
- O. A. Adeyemo and O. B. Soboyejo, “Frequency Distribution of ABO, RH Blood Groups and Blood Genotypes among the Cell Biology and Genetics Students of University of Lagos, Nigeria,” African Journal of Biotechnology, Vol. 5, No. 22, 2006, pp. 2062-2065.
NOTES
*Corresponding author.

