Open Journal of Anesthesiology
Vol.2 No.2(2012), Article ID:18549,6 pages DOI:10.4236/ojanes.2012.22007
The GlideScope® Video Laryngoscope and the Macintosh Laryngoscope Compared in a Simulated Difficult Airway with Immobilization and Bleeding—A Randomized, Prospective, Crossover Study
![]()
Penn State Milton S. Hershey Medical Center, Department of Anesthesiology, Penn State University, Herhsey, USA.
Email: *ackermannw00@gmail.com
Received January 17th, 2012; revised February 4th, 2012; accepted February 14th, 2012
Keywords: GlideScope; Difficult Airway
ABSTRACT
Background: This study assesses the effectiveness of the GlideScope® Videolaryngoscope (GS) in comparison with the Macintosh laryngoscope in a simulated difficult airway with blood in the airway and restricted range of motion of the neck. 39 participants experienced with the GS and the Macintosh laryngoscope were used. Methods: This analysis is a prospective, randomized, crossover study. Our study was performed on an intubation simulation model with artificial blood in the airway and restricted range of motion. The intubation time was recorded from picking up the laryngoscope to advancing the endotracheal tube through the glottic opening. Secondary endpoints were the Cormack & Lehane score, the percentage of the glottis seen, the subjective difficulty of the procedure on a scale of 0 to 10, the number of adjustment maneuvers, the number of attempts, and the number of failed intubations. Attempts were defined as removal of instruments from the airway and reinsertion. Failed intubations were defined as esophageal intubations or intubations lasting longer than 120 seconds. Results: The mean intubation time was 47.6 seconds with the GS and 21.4 seconds with the Macintosh laryngoscope. There were 3 failed intubations with the Macintosh laryngoscope and 4 failed intubations with the GS. The failed intubations with the Macintosh laryngoscope were all esophageal intubations. The failed intubations with the GS were due to exceeding the time limit of 120 seconds. Both devices had a mean Cormack & Lehane score of 1.8 and the mean percentage of the Glottis seen was 58% for both devices. The average subjective difficulty on a scale from 0 to 10 was ranked 4.16 for the Macintosh and 5.14 for the GS. Participants needed an average of 1 adjustment maneuvers with the Macintosh laryngoscope and 2.7 adjustments with the GS. Conclusion: The GS, used by experienced anesthesiologists in a simulated difficult airway, had an inferior performance compared to the Macintosh laryngoscope in terms of intubation time, number of intubation attempts, number of adjustment maneuvers, and number of failed intubations.
1. Introduction
The placement of an endotracheal tube (ETT) in order to secure the airway is possible in the majority of patients. This can commonly be accomplished with direct laryngoscopy, however, there is a 0.3% incidence of failed intubations [1]. If airway management fails, the outcome can be catastrophic.
The GlideScope® (GS), a new video device for indirect laryngoscopy is available since 2002 [2]. This is a device which is handled similarly to the Macintosh laryngoscope (Mac) [2-5]. It has a high resolution camera near the tip of the blade with a light source next to it [3-5]. This blade has a 60 degree angle [2,4,5]. The GS does not depend on an external line of sight from the anesthesiologist’s eye to the glottis and can provide a better view of the larynx compared to direct laryngoscopy [2,3]. Good visualization of the glottis and easy advancement of the ETT through the vocal cords is vital for the safety and efficiency of the intubation. The intubation can be watched on an LCD screen, which makes it easier for another person to help with a difficult airway. It is also very useful for teaching purposes [3,4].
The purpose of this study was to assess the effectiveness of the GlideScope® in comparison with the Macintosh laryngoscope in a simulated difficult airway with blood in the airway and restricted range of motion of the neck.
To our knowledge, this study is the only prospective, randomized, crossover study, which simulates a difficult airway with blood in the oropharynx. Bleeding can occur in different situations, such as traumatic airways or malignancies in the airway. Investigating the performance of airway devices in bloody airways is essential. Frequently, suctioning cannot resolve the blood, because the bleeding is too intense or because the blood is too thick or coagulated.
Our hypothesis, based on the results of previous studies [2-4,6,7], was that the GS has a superior performance compared to the Macintosh laryngoscope in terms of a difference in intubation time of at least 20 seconds.
Our study is a prospective, randomized, crossover study to compare the GlideScope® video laryngoscope and the Macintosh laryngoscope in a simulated difficult, bloody airway situation, and restricted range of motion of the neck.
2. Methods
This study was conducted at the Milton S. Hershey Medical Center. The Institutional Review Board exempted the study, because it was conducted on a model and did not involve real patients. Twenty-nine anesthesiology attendings and ten senior anesthesiology residents were recruited. The participants were informed about the study and voluntary verbal consent was obtained.
The AirSim Bronchi® intubation simulation model (TruCorp Limited Belfast, UK) was used. To simulate a difficult airway we injected artificial blood through a soft suction tube which was inserted nasally into the pharynx. The artificial blood was created in our simulation laboratory by combining normal saline and red food dye to a very dark red liquid. Clear surgical lubrication gel was then added to this liquid to obtain the viscosity of real blood. This artificial blood had the color, transparency, and viscosity of real partially clotted blood. Additionally, to simulate coagulated blood, we soaked a gauze pad (4 × 4 Kendall Curity gauze sponge 12-Ply USP type VII gauze, Tyco Healthcare) in the artificial blood after cutting it in half and inserted it into the manikin’s airway with the help of the GlideScope® and Magill forceps, so that it came into position right above the glottis, covering about 50% to 70% of the view onto the glottis. This was done by the same person each time to ensure the same conditions for each procedure. This person was not a participant in the study. Furthermore we restricted the neck extension of the model mechanically to simulate situations such as cervical spine immobilization via inline stabilization. Figure 1 shows our simulated airway seen on the GS screen. For direct visual laryngoscopy a

Figure 1. Our simulated airway on the GlideScope® screen. Visible is the large artificial blood clot. The glottis opening is visible as a dark circle above the blood clot. On the upper edge of the screen one can see a part of the epiglottis.
Macintosh blade size 3 was used. For indirect laryngoscopy we used the GlideScope® Cobalt video laryngoscope (Verathon Medical Inc., Bothell, WA, USA). A size 7.5 mm high volume low pressure oral/nasal cuffed ETT (Covidien Mallinckrodt, Mansfield, MA, USA) was used for all intubations. For intubations with the Macintosh laryngoscope the participants were provided a stylet, which they were allowed to bend and adjust according to preference. For intubations with the GS the stylet provided by the GS manufacturer was used.
The intubating conditions were exactly the same for each intubation, for both devices. Each participant attempted endotracheal intubation once with each device. The order in which the devices were used was determined by a computer generated randomization list. The two attempts were performed at a time interval no shorter than 24 hours.
Our primary outcome was the time until full visualization of the glottis and the time until completed intubation. Timing began when the participant picked up the laryngoscope and was stopped when the ETT passed through the vocal cords into the trachea. This could simply be seen by the observer watching the trachea equivalent of the manikin or on the monitor of the GS. Our hypothesis was that there would be an intubating time difference of at least 20 seconds. We believe that a difference of 20 seconds intubating time can be clinically significant.
Secondary outcomes were the Cormack & Lehane score, the percentage of the glottis visually appreciated by the participants, and the subjective difficulty of the procedure on a scale of 0 - 10. In addition we documented the number of adjustment maneuvers, the number of attempts, and the number of failed intubations. Adjustment maneuvers were defined as up and down movements of the laryngoscope or the ETT without removing these devices from the patient’s airway or the application of cricoid pressure. Attempts were defined as removal of all instruments from the airway for any reason and reinsertion. Failed intubations were defined as esophageal intubations, intubations that lasted longer than 120 seconds, or simply failure to pass the ETT through the vocal cords.
Paired t-tests were used to compare the two timepoints with respect to intubation time and time to glottis view as well as the glottis view, subjective difficulty, and number of adjustments. The calculated sample size to show a mean intubating time difference of 20 seconds with a power of 80% for a paired t-test was 34 participants. This calculation was done for an alpha error of 0.05 and an expected standard deviation of the mean difference of 40 seconds. Our sample for the intubating time was 34 pairs, because among 35 participants who intubated with both devices one was not able to intubate the trachea once, resulting in no intubating time. For all other outcomes the sample size was 35.
3. Results
We recruited 39 participants. Thirty-five participants intubated once with the GS and once with the Macintosh laryngoscope. Four participants only performed one intubation with either the GS or the Macintosh and did not return for their second intubation with the other device. Nonetheless, their data were included in our analysis, except for the paired t-tests. There were 74 intubations total, 38 with the Macintosh and 36 with the GS. All individuals had more than 2 years of experience in anesthesia and performed more than 200 intubations with the Macintosh laryngoscope and an average of 27.5 intubations with the GS.
Table 1 summarizes our results.
3.1. Time to Achieve an Effective Airway
The average time to view the glottis was significantly shorter using the Macintosh laryngoscope (11.9 ± 6.6 seconds) as compared to the GS (17.9 ± 9 seconds) (Figure 2). The mean time to intubation was significantly shorter for the Macintosh laryngoscope (21.4 ± 9.6 seconds) versus the GS (47.6 ± 38.7 seconds including 3 intubations that took more than 120 seconds and 38 ± 21 seconds when these 3 intubations were excluded) (Figure 2).
3.2. View
The mean Cormack & Lehane score was 1.8 for both devices. The mean percentage of the glottis seen by the participants was 58% for both devices. Therefore, the view of the glottis was rated the same for both devices and no significant difference could be detected with the paired t-test (Figure 2).
3.3. Difficulty
The average subjective difficulty on a scale from 0 to 10 was ranked 4.16 (±2.5) for the Macintosh and 5.14 (±2.5) for the GS. The paired t-test analysis did not show any significance (Figure 2).
3.4. Success
Participants needed an average of one adjustment maneuver with the Macintosh laryngoscope and 2.7 adjustments with the GS. The amount of adjustment maneuvers was significantly higher when the GS was used. All participants needed only one attempt for the intubation with the Macintosh laryngoscope. There were 5 participants
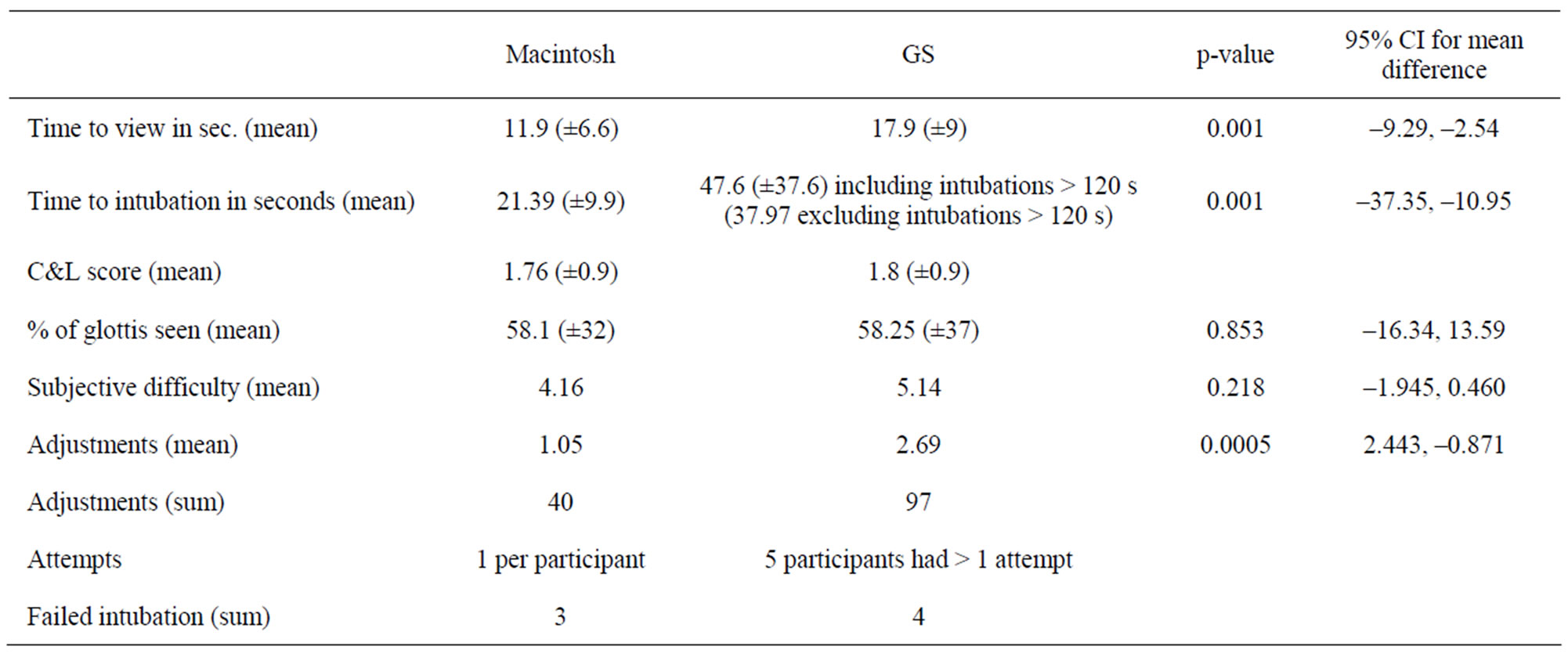
Table 1. Study outcomes, including paired t-test results with p-values and confidence intervals (standard deviation in brakets).
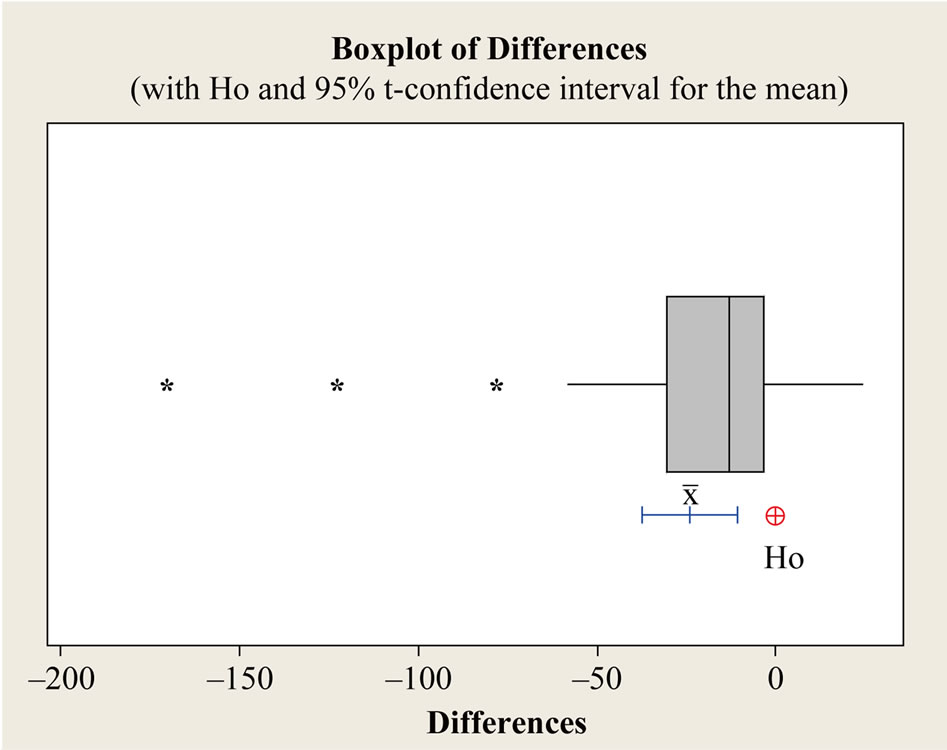
Figure 2. Bloxplot of differences with 95% interval for the mean and Ho for Time to intubate.
who needed more than one attempt to intubate with the GS. There were three failed intubations with the Macintosh laryngoscope, which were esophageal intubations. There were 4 failed intubations with the GS, 3 of which were classified failed, because it took more than 120 seconds to successfully intubate. There was difficulty advancing the ETT into the trachea, despite a good view onto the glottis. One intubation failed because the participant was not able to pass the ETT through the vocal cords into the trachea at all.
There were only three cases in which the GS had to be removed from the airway to wipe blood off the lens. Six participants specifically mentioned difficulty positioning and maneuvering the ETT to the vocal cords when using the GS.
4. Discussion
Since the introduction of the GlideScope® into clinical practice, it was compared with the Macintosh laryngoscope in several studies [2-18]. In most studies the participants did not have experience with the GlideScope® [2-6,11-14] and in some of the more recent studies the participants did not even have experience with direct laryngoscopy (medical students) [12,14]. Only three studies used exclusively participants with GS and Macintosh experience [7,8,17]. Our participants were experienced with both devices, although their experience with the Macintosh laryngoscope was greater which may bias our results towards this device. However, the GS holds a much steeper learning curve compared to the Macintosh laryngoscope [3-5]. This is demonstrated by the finding that participants with no experience with direct and indirect laryngoscopy needed less time to intubate with the GS [14]. Furthermore, the experience of our participants correctly reflects the clinical experience many anesthesiologists have with both devices.
The initial publications utilized patients as study subjects [2,3,6-8,12,17,18], while more recent reports, including this study, chose to use simulated airway models [4,5,10,11,13-16]. We are not aware of any previous study that included blood in the airway. To our knowledge, there is only one other study apart from ours that set a specific time interval in between the intubations [5]. This was done to avoid the learning effect, so that participants could not develop any routine skills with our simulation model.
Our results show that the mean time to intubation was significantly longer with the GS compared to the Macintosh laryngoscope. This outcome reflects what was found in previous studies which show that experienced participants who perform intubations frequently require less time to intubation with the Macintosh laryngoscope compared to the GS [7,16,18]. Participants with no experience with direct and indirect laryngoscopy needed less time to intubate even easy airways with the GS [14].
Previous studies found the time to intubate with the GS is longer in normal airways, but only minimally longer to significantly shorter the more difficult the airway becomes [4,8,10,13,15,17].
The advancement of the ETT to the vocal cords is challenging with the GS and might require some experience with the device [3-5,7,8]. This has been reported to be the main reason for the prolonged time for intubation and failure to intubate using the GS. Our results confirm this. The average time to view the glottis was only six seconds longer using the GS. This difference, although significant, of may not be of clinical importance. The mean time to intubation was significantly longer with the GS compared to the Macintosh and this difference has great clinical relevance. While it is often not difficult to obtain a view of the vocal cords with the GS, the difficulty using the GS is to maneuver the ETT to the vocal cords and into the trachea. Mastering this might take a certain degree of experience.
Previous studies showed that with the GS the glottis view is the same or somewhat better in easy airways but significantly better in difficult airways. Especially, in patients with limited range of motion of the neck and/or tongue edema the glottis view is greatly improved [2,3, 5-12,15,17-19]. In our study the view of the glottis was rated the same for both devices.
The literature rates the subjective difficulty of the intubation process as about the same for easy airways and often easier with the GS for difficult airways [4,5,7,10, 11,13,17]. The experience of the participants has great influence on this outcome. Participants without experience with direct and indirect laryngoscopy find the GS less difficult to use even in easy airways [13,14]. According to our results the average subjective difficulty on a scale from 0 to 10 was ranked one point higher for the GS. However, this difference was not statistically significant.
In previous studies less optimization maneuvers were needed with the GS during the intubation (i.e. cricoid pressure etc.) [7,13,14,17]. In our study participants needed significantly more adjustment maneuvers when using the GS. This was most likely due to difficulty advancing the ETT to the vocal cords.
In three cases the GS had to be wiped clean due to blood on the lens which caused the participant to have more than one attempt to intubate with the GS. We feel that the need to wipe blood off the GS lens in only three cases speaks for the use of this device in a difficult bloody airway.
All three failed intubations with the Macintosh laryngoscope were esophageal intubations. We believe that this is a noteworthy finding. Esophageal intubations can increase the risk for aspiration due to gastric inflation. They also increase the risk for hypoxia as they can go unnoticed. None of our participants were aware that they intubated the esophagus until they were notified of it. There were no esophageal intubations with the GS.
As shown in Figure 1, we created a very realistic traumatic airway and usually there is thick blood and blood clots involved. An ETT may be able to penetrate a true blood clot. In our model the ETT would drag the artificial blood clot into the trachea in very few cases. The artificial blood clot was placed with the GS. This could bias the results towards the GS. Our results show that this bias did not occur. The placement of the clot was done by one separate person that did not participate in the study. The tracheal tube may impact the anterior wall of the subglottic space when using the Glidescope [20]. This is a potential reason for prolonged intubation that we could not reconstruct in our model, because the subglottic airway in our model was soft rubber.
Using a simulated airway model has the advantage of providing a consistent standardized airway. When using real patients, it is difficult to create a standardized consistent airway and there are ethical concerns as well. However, we have to point out that essentially all treatments and devices have to be studied on real patients under common conditions before final conclusions can be drawn.
Some of our secondary endpoints, such as the view and the difficulty of the intubation, were subjective and can vary between participants simply because of different judgment, which can affect the results.
It is impossible to blind our study, because the participants will always know what device they are using to intubate. This might have created some bias.
5. Conclusion
We could not show any benefit of the GS. The GS had a lower performance compared to the Macintosh laryngoscope in terms of intubation time, number of intubation attempts, number of adjustment maneuvers and number of failed intubations. We were not able to prove our hypothesis.
REFERENCES
- B. T. Finucane and A. H. Santora, “Principles of Airway Management,” 3rd Edition, Springer-Verlag Inc., New York, 2003.
- F. S. Xue, G. H. Zhang, J. Liu, X. Y. Li, Q. Y. Yang, Y. C. Xu and C. W. Li, “The Clinical Assessment of Glidescope in Orotracheal Intubation under General Anesthesia,” Minerva Anestesiologica, Vol. 73, No. 9, 2007, pp. 451-457.
- R. M. Cooper, J. A. Pacey, M. J. Bishop and S. A. McCluskey, “Early Clinical Experience with a New Videolaryngoscope (GlideScope®) in 728 Patients,” Canadian Journal of Anaesthesia, Vol. 52, No. 2, 2005, pp. 191-198. doi:10.1007/BF03027728
- T. J. Lim, Y. Lim and E. H. Liu, “Evaluation of Ease of Intubation with the GlideScope® or Macintosh Laryngoscope by Anaesthetists in Simulated Easy and Difficult Laryngoscopy,” Anaesthesia, Vol. 60, No. 2, 2005, pp. 180-183. doi:10.1111/j.1365-2044.2004.04038.x
- H. J. Kim, S. P. Chung, I. C. Park, J. Cho, H. S. Lee and Y. S. Park, “Comparison of the GlideScope Video Laryngoscope and Macintosh Laryngoscope in Simulated Tracheal Intubation Scenarios,” Emergency Medicine Journal, Vol. 25, 2008, pp. 279-282. doi:10.1136/emj.2007.052803
- M. R. Rai, A. Dering and C. Verghese, “The Glidescope® System: A Clinical Assessment of Performance,” Anaesthesia, Vol. 60, No. 1, 2005, pp. 60-64. doi:10.1111/j.1365-2044.2004.04013.x
- M. A. Malik, C. H. Maharaj, B. H. Harte and J. G. Laffey, “Comparison of Macintosh, Truview
 , Glidescope®, and Airwayscope® Laryngoscope Use in Patients with Cervical Spine Immobilization,” British Journal of Anaesthesia, Vol. 101, No. 5, 2008, pp. 723-730. doi:10.1093/bja/aen231
, Glidescope®, and Airwayscope® Laryngoscope Use in Patients with Cervical Spine Immobilization,” British Journal of Anaesthesia, Vol. 101, No. 5, 2008, pp. 723-730. doi:10.1093/bja/aen231 - D. A. Sun, C. B. Warriner, D. G. Parsons, R. Klein, H. S. Umedaly and M. Moult, “The GlideScope® Video Laryngoscope: Randomized Clinical Trial in 200 Patients,” British Journal of Anaesthesia, Vol. 94, No. 3, 2005, pp. 381-384. doi:10.1093/bja/aei041
- Y. Hirabayashi, T. Hakozaki, K. Fujisawa, N. Sata, S. Kataoka, O. Okada, M. Yamada, K. Hotta, N. Seo and K. Ikeda, “Use of a New Video-Laryngoscope (GlideScope) in Patients with a Difficult Airway,” Masui, Vol. 56, No. 7, 2007, pp. 854-857.
- G. L. Savoldelli, E. Schiffer, C. Abegg, V. Baeriswyl, F. Clergue and J. L. Waeber, “Comparison of the Glidescope®, the McGrath®, the Airtraq® and the Macintosh Laryngoscopes in Simulated Difficult Airways,” Anaesthesia, Vol. 63, No. 12, 2008, pp. 1358-1364. doi:10.1111/j.1365-2044.2008.05653.x
- M. A. Malik, C. O’Donoghue, J. Carney, C. H. Maharaj, B. H. Harte and J. G. Laffey, “Comparison of the Glidescope®, the Pentax AWS®, and the Truview
 with the Macintosh Laryngoscope in Experienced Anaesthetists: A Manikin Study,” British Journal of Anaesthesia, Vol. 102, No. 1, 2009, pp. 128-134. doi:10.1093/bja/aen342
with the Macintosh Laryngoscope in Experienced Anaesthetists: A Manikin Study,” British Journal of Anaesthesia, Vol. 102, No. 1, 2009, pp. 128-134. doi:10.1093/bja/aen342 - P. Nouruzi-Sedeh, M. Schumann and H. Groeben, “Laryngoscopy via Macintosh Blade versus GlideScope: Success Rate and Time for Endotracheal Intubation in Untrained Medical Personnel,” Anesthesiology, Vol. 110, No. 1, 2009, pp. 32-37. doi:10.1097/ALN.0b013e318190b6a7
- S. Nasim, C. H. Maharaj, M. A. Malik, J. O’Donnell, B. D. Higgins and J. G. Laffey, “Comparison of the Glidescope® and Pentax AWS® Laryngoscopes to the Macintosh Laryngoscope for Use by Advanced Paramedics in Easy and Simulated Difficult Intubation,” BMC Emergency Medicine, No. 17, 2009, p. 9. doi:10.1186/1471-227X-9-9
- M. A. Malik, P. Hassett, J. Carney, B. D. Higgins, B. H. Harte and J. G. Laffey, “A Comparison of the Glidescope®, Pentax AWS®, and Macintosh Laryngoscopes When Used by Novice Personnel: A Manikin Study,” Canadian Journal of Anaesthesia, Vol. 56, No. 11, 2009, pp. 802- 811. doi:10.1007/s12630-009-9165-z
- A. T. Narang, P. F. Oldeg, R. Medzon, A. R. Mahmood, J. A. Spector and D. A. Robinett, “Comparison of Intubation Success of Video Laryngoscopy versus Direct Laryngoscopy in the Difficult Airway Using High-Fidelity Simulation,” The Journal of the Society for Simulation in Healthcare, Vol. 4, No. 3, 2009, pp. 160-165. doi:10.1097/SIH.0b013e318197d2e5
- L. Powell, J. Andrzejowski, R. Taylor and D. Turnbull, “Comparison of the Performance of Four Laryngoscopes in a High-Fidelity Simulator Using Normal and Difficult Airway,” British Journal of Anaesthesia, Vol. 103, No. 5, 2009, pp. 755-760. doi:10.1093/bja/aep232
- M. A. Malik, R. Subramaniam, C. H. Maharaj, B. H. Harte and J. G. Laffey, “Randomized Controlled Trial of the Pentax AWS®, Glidescope®, and Macintosh Laryngoscopes in Predicted Difficult Intubation,” British Journal of Anaesthesia, Vol. 103, No. 5, 2009, pp. 761-768. doi:10.1093/bja/aep266
- G. Serocki, B. Bein, J. Scholz and V. Dörges, “Management of the Predicted Difficult Airway: A Comparison of Conventional Blade Laryngoscopy with Video-Assisted Blade Laryngoscopy and the GlideScope,” European Journal of Anaesthesiology, Vol. 27, No. 1, 2010, pp. 24- 30. doi:10.1097/EJA.0b013e32832d328d
- G. L. Murrell, K. M. Sandberg and S. A. Murrell, “GlideScope Video Laryngoscopes,” Otolaryngology—Head and Neck Surgery, Vol. 136, 2007, pp. 307-308. doi:10.1016/j.otohns.2006.10.003
- W. A. Dow and D. G. Parsons, “‘Reverse Loading’ to Facilitate Glidescope® Intubation,” Canadian Journal of Anaesthesia, Vol. 54, No. 2, 2007, pp. 161-162. doi:10.1007/BF03022022
NOTES
*Corresponding author.

