World Journal of Cardiovascular Diseases
Vol.2 No.2(2012), Article ID:18741,7 pages DOI:10.4236/wjcd.2012.22010
Electrocardiogram manifestations in hyperkalemia
![]()
1Woodhull Medical Center, New York University School of Medicine, New York, USA
2St. George’s University School of Medicine, St. George’s, Grenada
Email: *ronny.cohen@nychhc.org
Received 31 October 2011; revised 16 December 2011; accepted 23 December 2011
Keywords: EKG; ECG; Hyperkalemia; Electrocardiogram
ABSTRACT
Hyperkalemia is defined as serum potassium level of more than 5 mmol/L. Prompt identification of hyperkalemia and appropriate management are critical, since severe hyperkalemia can lead to lethal cardiac dysrhythmias. There is a wide range of electrocardiogram (EKG) changes associated with hyperkalemia. The sequence of EKG changes has been previously described with limited information to correlate the level of potassium to a particular change in the EKG. This study aims to describe a correlation between the level of potassium and EKG changes in the presence or absence of certain diagnoses, to determine which EKG finding in the context of level of hyperkalemia, should be considered life-threatening and prompt emergency intervention. If a relationship between serum levels of potassium and EKG changes is significant, clinicians may be able to better monitor and treat hyperkalemic patients. This paper reviews the literature on hyperkalemia, potassium homeostasis and EKG changes attributed to elevated potassium.
1. INTRODUCTION
Extracellular potassium concentration is normally maintained between 4 and 4.5 mmol/L. Hyperkalemia is defined as serum potassium level greater than 5.0 mmol/L. It is a common metabolic disturbance with potentially life-threatening consequences. Since severe hyperkalemia can lead to lethal cardiac dysrhythmias, prompt identification of hyperkalemia and appropriate management are crucial.
1.1. Normal Potassium Homeostasis
The serum potassium concentration is determined by the relationship between potassium intake, the distribution of potassium in the cells and the extra cellular fluid, and urinary potassium excretion. In normal subjects, dietary potassium is largely excreted in the urine, a process that involves the potassium secretion in the principal cells in the cortical collecting tubule. The degree of potassium secretion is primarily stimulated by three factors: an increase in the serum concentration, a rise in the plasma aldosterone concentration and enhanced delivery of sodium and water to the distal secretory site.
Under normal circumstances, renal excretion accounts for approximately 90% of daily potassium elimination. Distal tubule urine flow may influence potassium secretion because increased flow increases the concentration gradient and therefore, potassium loss. As renal function declines, a greater fraction of the filtered load is excreted, and plasma potassium levels generally do not rise until renal function declines to less than 25% of normal [1-3].
1.2. Causes of Hyperkalemia
There are numerous causes of hyperkalemia. Elevated serum potassium levels can be due to either true hyperkalemia or pseudohyperkalemia. Pseudohyperkalemia is artificially elevated plasma potassium [K+] in a blood specimen due to potassium movement out of the cells. The major cause of pseudohyperkalemia is mechanical trauma during venipuncture (hemolytic) and prolonged tourniquet placement during venipuncture. This may result in potassium release from cells and adds characteristic reddish tint to serum due to concomitant release of hemoglobin from cells.
True hyperkalemia occurs as a result of transcellular shift, increased potassium intake and decreased potassium excretion by kidneys. Transcellular shift can result from Diabetic Ketoacidosis (DKA). The acidemia in DKA causes hydrogen ions (H+) to move into cells and K+ ions to move out of cells to maintain electroneutrality, resulting in subsequent hyperkalemia. Insulin deficiency and hyperosmolar state also contribute to the shift of potassium from intracellular fluid to extracellular fluid. Other examples include non-selective beta-blockers, digitalis overdose, tumor lysis syndrome, rhabdomyolysis, et al. Increased potassium intake is usually iatrogenic due to over replenishing of potassium in the presence of renal impairment. It may occur slowly if the kidney cannot excrete potassium (e.g. renal failure, aldosterone antagonists), and it may occur rapidly if potassium is being dumped from cells into the blood (e.g. crushing injuries, necrotic tissue, acidosis). The failing kidney can adapt by increasing potassium excretion per functioning nephron is low potassium diet is maintained, until oliguria ensues [4-6]. Any cause of decreased aldosterone release can decrease the efficiency of potassium excretion. Drugs affecting aldosterone include potassium-sparing diuretics, NSAIDs, heparin and pentamidine. The Transtubular Potassium Gradient (TTKG) can be useful when suspecting the diagnosis of hypoaldosteroneism. The TTKG in normal subjects on a regular diet are 8 - 9, and rises to 11 with a potassium load, indicating increased potassium secretion. A value below 7, particularly below 5 in a hyperkalemic patient is highly suggestive of hypoaldosteronism. The diagnosis can be confirmed with the serum level of plasma aldosterone.
Renal tubular acidosis (RTA) is a disease that occurs when the kidneys fail to excrete acids into the urine, which causes a person’s blood to remain too acidic. There are several types of RTA. Type 4 is called hyperkalemic RTA and is caused by a generalized transport abnormality of the distal tubule. The transport of electrolytes such as sodium, chloride, and potassium that normally occurs in the distal tubule is impaired. Type 4 RTA occurs when blood levels of the hormone aldosterone are low or when the kidneys do not respond to it. Drugs that may cause type 4 RTA include diuretics, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), trimethoprim, pentamidine, heparin, nonsteroidal anti-inflammatory drugs (NSAIDs) and some immunosuppressive medications. Type 4 RTA may also result from diseases that alter kidney structure and function such as diabetic nephropathy, HIV/AIDS, Addison’s disease, sickle cell disease, urinary tract obstruction, lupus, amyloidosis, removal or destruction of both adrenal glands, and kidney transplant rejection [7].
1.3. Clinical Manifestations of Hyperkalemia
Hyperkalemia can be difficult to diagnose clinically since complaints may be vague. With non-specific findings, hyperkalemia often is an incidental laboratory finding. Clinical manifestations depend on both the severity as well as the rate of increase in potassium concentration. Patients with hyperkalemia may present as asymptomatic or may report weakness, generalized fatigue, paresthesias, paralysis or even cardiac arrest [3,8,9]. Patient history is most valuable in identifying conditions that may predispose hyperkalemia.
1.4. EKG Changes with Hyperkalemia
Hyperkalemia is not always expressed with EKG changes, therefore EKG is not a reliable indicator of the severity of hyperkalemia. Profound hyperkalemia can be seen in absence of classic EKG changes, but the presence of EKG changes mandates treatment [10,11]. The EKG changes from hyperkalemia can range from peaked T waves, loss of P waves, prolonged QRS complex, ST segment elevation, extopic beats and escape rhythm, progressive widening of QRS complex, sine wave, ventricular fibrillation, asystole, axis deviation, bundle branch block and fascicular blocks. EKG alterations are also associated with sinus node depression, appearance of escape rhythms and malignant ventricular arrhythmias [12-14].
Hyperkalemia can cause several characteristic EKG abnormalities that are often progressive. Initially the T wave becomes tall, symmetrically peaked and tented. Widening of the QRS complex with an intraventricular conduction delay then occurs. Additional elevation of serum potassium leads to a decrease in the amplitude of the P wave and its eventual disappearance from the EKG. Rarely, ST segment elevation mimicking myocardial infarction, described as “pseudoinfarction” pattern, is present. Further progression of hyperkalemia leads to a sine wave appearance of EKG and eventual asystole. These progressive changes in EKG have not been previously studied in respect to the corresponding serum K+ levels.
1.5. Therapeutic Options for Hyperkalemia
Hyperkalemia is one of the most fatal electrolyte abnormalities; it is also the most treatable. American Heart Association defines hyperkalemia as greater than 5 mEq/L, and moderate (6 - 7 mEq/L) and severe (>7 mEq/L) are life threatening and require immediate therapy. Therapeutic options aim to antagonize the effects of hyperkalemia at the cellular level (calcium salts, decrease serum potassium levels by promoting the influx of potassium into cells of the body (insulin and sodium bicarbonate), and finally, remove potassium from the body (resins, loop diuretics, hemodialysis) [6,14].
Calcium salts, such as calcium chloride and calcium gluconate, antagonize cardiac toxicity by increasing the threshold potential and reestablishing cardiac excitability but have no direct effect on potassium levels. Calcium administration shifts the threshold potential shifts to a less negative value (that is, from –75 mV to –65 mV), so that the initial difference between resting and threshold potentials of 15 mV can be restored. Calcium therapy for hyperkalemia is contraindicated in the setting of digoxin toxicity because calcium can potentiate the toxic effects of this drug.
Shifting potassium from the extracellular to the intracellular compartment remains a mainstay of acute treatment. Insulin and beta-2 adrenergic agonists (e.g., salbutamol/albuterol) decrease serum potassium by stimulating the Na/K-ATPase pump, shifting potassium from the extracellular to the intracellular compartment in exchange for sodium. Beta-2 adrenergic stimulants combined with insulin have been shown to have potassium-lowering effect greater than when used alone, and also have been shown to reduce the incidence of insulin induced hypoglycemia. The efficacy of beta-2 adrenergic agonists is variable, and these agents should not be used as monotherapy. There is growing evidence for the role of albuterol in treating severe hyperkalemia [15]. Catecholamines activate Na-K ATPase pumps through B2 receptor stimulation that may add to the effects on insulin [16]. In addition to insulin, sodium bicarbonate buffers hydrogen ions extracellularly while shifting potassium intracellularly to maintain electrical neutrality. Sodium bicarbonate should be reserved for cases with metabolic acidosis because effects may be delayed or unreliable especially in patients with renal dysfunction.
Resins such as sodium polystyrene sulfonate are used to move potassium out of the body via the gastrointestinal tract. Each 1 g of resin administered orally removes approximately 1 mEq of potassium. Forced diuresis with a loop diuretics (e.g. furosemide) takes advantage of the potassium-wasting effects of furosemide. Loop diuretics act by blocking the tubular reabsorption of sodium in the loop of Henle and early distal tubule, thus increasing sodium delivery to the distal tubule and stimulating potassium excretion [17,18]. The ultimate therapy for hyperkalemia due to iatrogenic causes is hemodialysis, but while waiting 50% dextrose and insulin may be given to push potassium into cells, NG suction and exchange resins may be given to remove potassium via the GI tract or IV calcium may be given to neutralize its effect on cellular membranes [19]. The latter provides the quickest protection [20].
2. METHODS
2.1. Study Design and Population
This is a retrospective, non-randomized review based on the medical records. The institutional review board of the medical center approved the study design. The study population included consecutive patients admitted to Woodhull Medical Center in Brooklyn, NY, diagnosed with hyperkalemia in the period from January 1, 2005- October 31, 2007. Data will be collected by reviewing medical records using either electronic medical records as well as physical charts of previously discharged patients admitted with a diagnosis of hyperkalemia in the Medical-Surgical unit including ICU and Telemetry.
2.2. Study Protocol
Each chart was carefully reviewed for different parameters and demographic information. The EKGs taken at the moment of high levels of potassium were interpreted to see any changes compared to previous EKGs (if available). This data was analyzed according to the level of significance, if any correlation is found between a certain level of serum potassium and certain EKG changes. A value will be given according to how strong this correlation is.
EKGs done at the time of less than one hour when the high potassium level was measured were interpreted by two different cardiologists (Figures 1-3). Any positive finding will be recorded. If the presence of an EKG change is consistently seen at a certain level or interval throughout all the samples in a significant manner using statistical calculations, a correlation can be made between EKG change with special serum potassium levels.
3. RESULTS
A total of 309 patients met the defined criteria. Demographic breakdown of the sample is depicted in Table 1. More than half the sample was male, 90% were either Hispanic or African American, and the average age was 62.47 years, (range = 23 - 102 years). Nearly three quarters (73.8%) of the sample had renal failure (defined as signs of kidney injury or a GFR less than 90 cc/kg/hr). Of those with renal failure, 9% (21/228) had end stage renal disease (defined as a GFR less than 15 cc/kg/hr). Two thirds of the sample (67.6%; 209/309) was diabetic.
Levels of serum potassium were collected for the sample. The distribution is illustrated in Table 2. Twelve
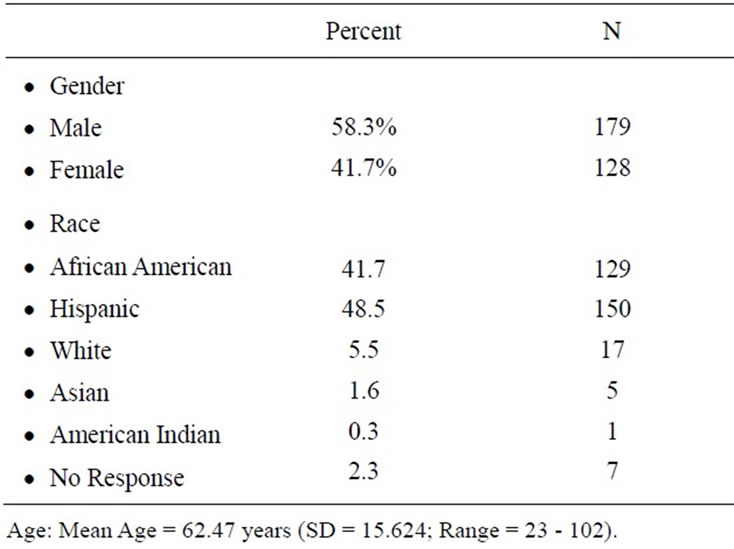
Table 1. Demographics of respondents.
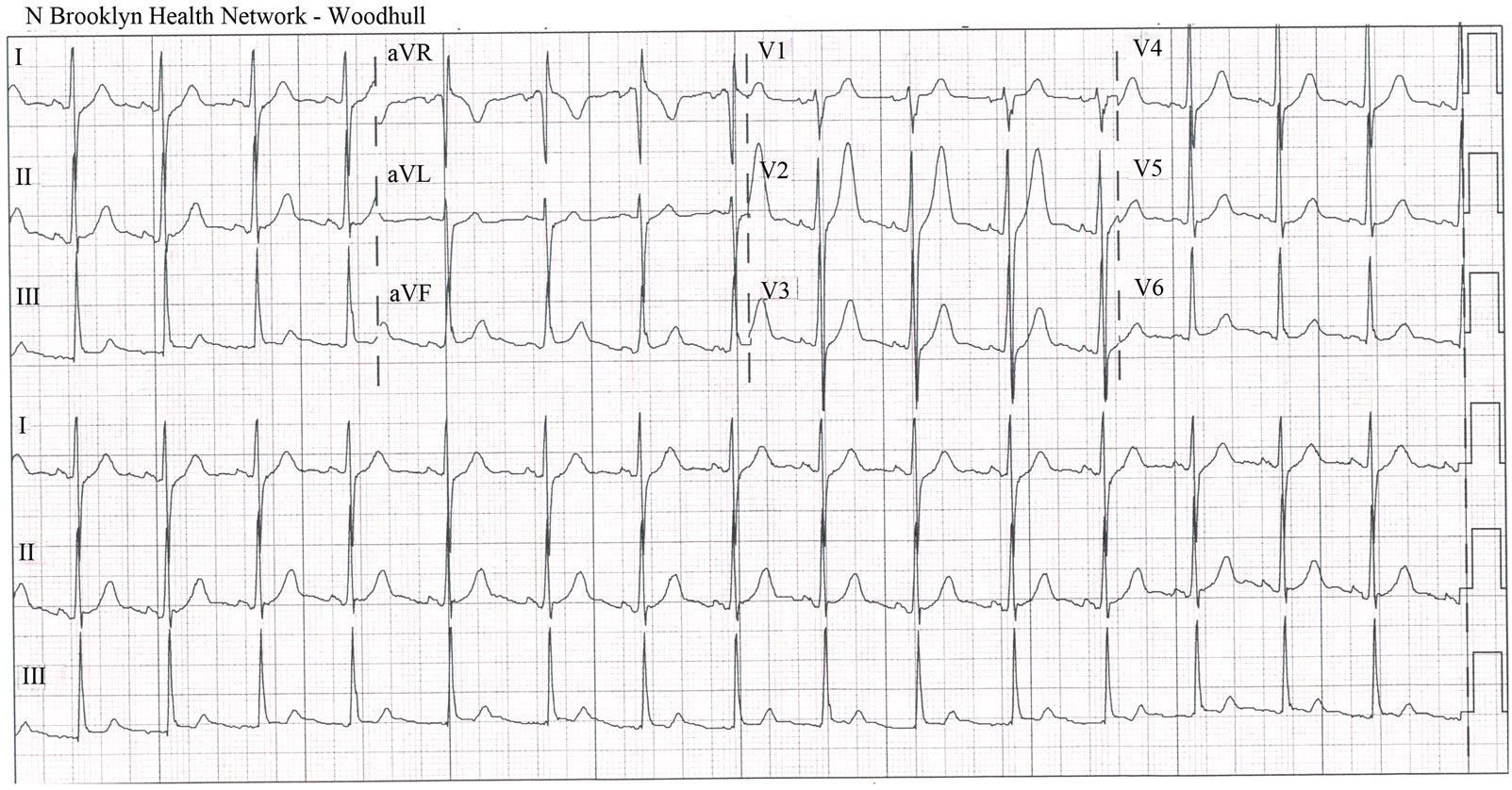
Figure 1. EKG manifestations with potassium level of 5.5 mEq/L.
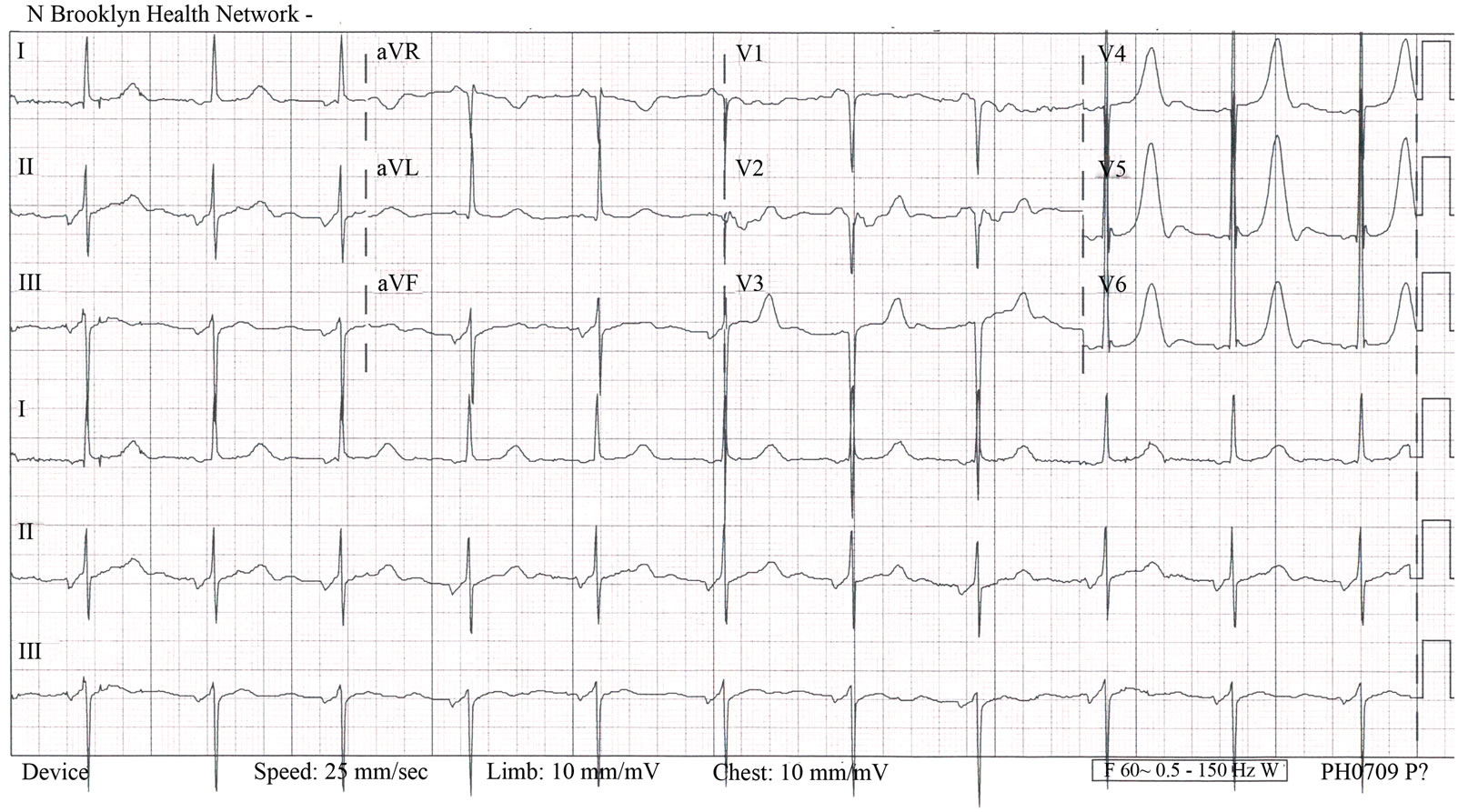
Figure 2. EKG manifestations with potassium level of 6.1 mEq/L.
patients with hyperkalemia were not included because their samples were hemolyzed. No statistically significant relationships were found between serum potassium levels and gender or race/ethnicity. Therefore, the sample was treated as a whole.
EKGs were performed and available on 292 of the patients. There were 36 EKGs reported as abnormal with changes consistent with hyperkalemia. Four distinct groups were identified: Peaked T waves, prolonged QRS, prolonged QTc interval, and prolongation of the PR interval. There were no statistically significant relationships identified between EKG results and serum potassium levels.

Figure 3. EKG manifestations with potassium level of 6.8 mEq/L.
(see Table 3).
4. DISCUSSION
Hyperkalemia was diagnosed in all patients, however only 36 EKGs were reported abnormal with changes with hyperkalemia. As seen in previous studies, not all patients with hyperkalemia had any abnormal EKG manifestations. Patients presenting with hyperkalemia may have a normal EKG or have changes that are so
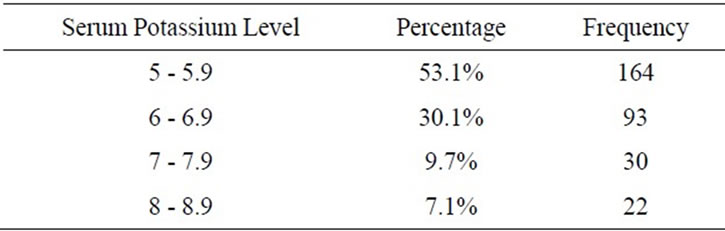
Table 2. Serum potassium levels, total sample.
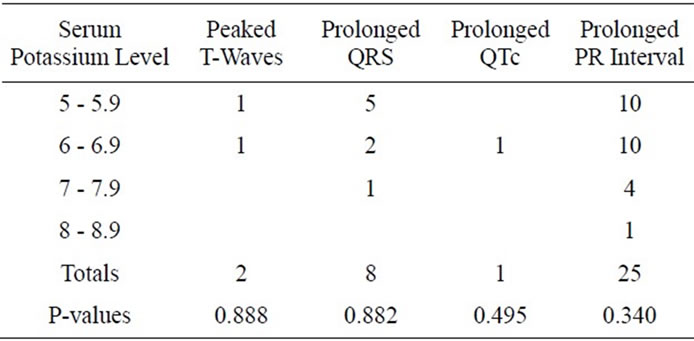
Table 3. Serum Potassium Levels by EKG Findings Consistent with Hyperkalemia.
subtle that physicians have difficulty attributing these changes to potassium levels. Within this study, only 40 abnormal EKGs were found of the 292 patients included in this study. This is consistent with previous reviews of EKG changes with hyperkalemia, the sensitivity of EKG for diagnosis of hyperkalemia is poor.
The patients had a range of elevated serum potassium levels, from mildly elevated 5 - 5.9 mmol/L to severe 8 - 8.9 mmol/L. There were inconsistent EKG abnormalities in each level of potassium elevation. The range of EKG changes varied from peaked T-waves, prolonged QRS, prolonged QTc interval and prolonged PR interval. Peaked T-waves, the most commonly associated EKG change with hyperkalemia, was seen only in two EKGs in the mild levels of hyperkalemia (5 - 6.9 mmol/L). Prolonged PR interval was seen in all ranges of serum K+ levels, also primarily in mild levels. Previous case reports have shown that even with the most profound potassium elevations (greater than 9.0 mEq/L), EKG did not reveal expected manifestations of hyperkalemia. Thus, even with profound serum potassium elevations, EKG cannot reliably be used to exclude the presence of hyperkalemia or to monitor therapy designed to lower the serum potassium concentration. While there were EKG changes seen in a range of serum K+ levels, these corresponding changes were insignificant. There is no correlation between serum K+ level and specific EKG findings.
In experimental models, there is an orderly progression of EKG changes induced by hyperkalemia. Peaked T-waves are usually seen at potassium concentration greater than 5.5 mEq/L and are best seen in leads II, IIIand V2 - V4, but are present in only 22% of the patients with hyperkalemia. As serum potassium levels increase to greater than 6.5 mEq/L, the rate of phase 0 of the action potential decreases, leading to a longer action potential and in turn, a widened QRS complex and prolonged PR interval. As potassium levels reach 8 to 9 mEq/L, sinoatrial node activity may stimulate ventricles without evidence of atrial activity, producing a sinoventricular rhythm. As hyperkalemia worsens and the potassium levels reach 10 mEq/L, SA node conduction no longer occurs, and passive junctional pacemakers take over electrical stimulation of the myocardium. Unabated, the QRS complex widens and blends into T waves, producing classic sine-wave EKG. Once this occurs, ventricular fibrillation and asystole are imminent. In clinical practice and within this study, progressive EKG changes are not consistent with experimental models based on level of potassium severity. In one published series of 127 patients with serum potassium concentrations ranging from 6 and 9.3 mEq/L, no serious arrhythmias were documented. Only 46% of EKGs were noted to have any changes suggestive of hyperkalemia.
4.1. Limitations
The retrospective design of this study may have missed cases of hyperkalemia. We were not able to determine cases of hyperkalemia that did not have a laboratory confirmation of hyperkalemia.
The sample size of this population was 309 patients, however only 36 had abnormal EKGs. With this small number of EKGs available, the study may be underpowered. While serum levels were not correlated with specific EKG abnormalities, the relationship may not be seen in such a small sample size.
There is also potential for confounding variables. While there was identifiable EKG abnormalities, most were nonspecific changes and not correlated with any potassium level. This may be associated with the fact that 6.7% of the patients in this study had End-Stage Renal Disease and 72% were in renal failure. It has been previously reported that hemodialysis patients with hyperkalemia are less likely to show EKG changes, despite the risk for suddenly developing arrhythmias including asystole or ventricular fibrillation without prior EKG abnormalities.
4.2. Conclusion
With the nonspecific nature of symptoms and variability in the serum potassium levels at which manifestations may occur, it is tempting to utilize EKG to identify patients who show early cardiac manifestations of hyperkalemia while waiting for laboratory confirmation. EKG manifestations are not consistent or indicative of severity of hyperkalemia. The challenge in managing hyperkalemia comes from the fact that it can be difficult, if not impossible, to identify the condition solely based on EKG information. Management of potassium should be guided by clinical scenario and serial potassium measurements. Because of such variability in the clinical presentation of hyperkalemia and inconsistency and absence of changes in EKG, recognition of patients with severe hyperkalemia continues to be challenging to clinicians and initiation of appropriate therapy may be delayed.
REFERENCES
- Sood, M.M., Sood, A.R. and Richardson, R., (2007) Emergency management and commonly encountered outpatient scenarios in patients with hyperkalemia. Mayo clinic proceedings, 82, 1553-1561.
- Rose, B.D. and Post, T.W. (2001) Clinical physiology of acid-base and electrolyte disorders. 5th edition, McGrawHill, New York.
- Clark, B.A. and Brown, R.S. (1995) Potassium homeostasis and hyperkalemic syndromes. Endocrinology and Metabolism Clinics of North America, 24, 573-591.
- de Denus, S., Tardiff, J.C., Bourassa, M.G., Racine, N., Levesque, S. and Ducharme, A. (2006) Quantification of the risk and predictors of hyperkalemia in patients with left ventricular dysfunction: a retrospective analysis of the studies of left ventricular dysfunction (SOLVD) trials. American Heart Journal, 152, 705-712. doi:10.1016/j.ahj.2006.05.030
- Sims, D.B. and Sperling, L.S. (2005) Images in cardiovascular medicine. ST-segment elevation resulting from hyperkalemia. Circulation, 11, e295-e296. doi:10.1161/01.CIR.0000165127.41028.D1
- Acker, C.G., Johnson, J.P., Palevsky, P.M. and Greenberg, A. (1998) Hyperkalemia in hospitalized patietns: causes, adequacy of treatment, and results of an attempt to improve physician compliance with published therapy guidelines. Archives of Internal Medicine, 158, 917-924. doi:10.1001/archinte.158.8.917
- Brenner, B.M. and MacKenzie, H.S. (1998) Disturbance of renal function. In: Harrison, T.R., ed., Principles of internal medicine. 14th edition, McGraw-Hill, New York, 1499.
- Effiong, C., Ahuja, T.S., Wagner, J.D., et al. (1997) Reversible hemiplegia as a consequence of severe hyperkalemia and cocaine abuse in a hemodialysis patient. The American Journal of the Medical Sciences, 314, 408-410. doi:10.1097/00000441-199712000-00010
- Quick, G. and Bastani, B. (1994) Prolonged asystolic hyperkalemic cardiac arrest with no neurologic sequelae. Annals of Emergency Medicine, 24, 305-311.
- Martinez-Vea, A., Bardaji, A., Garcia, C. and Oliver, J.A. (1999) Severe hyperkalemia with minimal electrocardiographic manifestations. Journal of Electrocardiology, 32, 45-49. doi:10.1016/S0022-0736(99)90020-1
- Yu, A.S. (1996) Atypical electrocardiographic changes in severe hyperkalemia. The American Journal of Cardiology, 77, 906-908. doi:10.1016/S0002-9149(97)89197-7
- Lin, J. and Huang, C. (1990) Successful initiation of hemodialysis during cardiopulmonary resuscitation due to lethal hyperkalemia. Critical Care Medicine, 18, 342-343. doi:10.1097/00003246-199003000-00022
- Dittrich, K.I. and Walls, R.M. (1986) Hyperkalemia: ECG manifesttations and considerations. The Journal of Emergency Medicine, 4, 449-55. doi:10.1016/0736-4679(86)90174-5
- Carbalhana, V., Burry, L. and Lapinsky, S.E. (2006) Management of severe hyperkalemia without hemodialysis: case report and literature review. Journal of Critical Care, 21, 316-321. doi:10.1016/j.jcrc.2005.10.001
- Parham, W., Mehdirad, A., Biermann, A. and Friedman, C. (2006) Hyperkalemia revisited. Texas Heart Institute Journal, 33, 40-47.
- Reardon, L.C. and MacPherson, D.S. (1998) Hyperkalemia in outpatients using angiotensin-converting enzyme inhibitors. Archives of Internal Medicine, 158, 26-32. doi:10.1001/archinte.158.1.26
- Ahee, P. and Crowe, A.V. (2000) The management of hyperkalemia in the emergency department. Journal of accident & emergency medicine, 17, 188-191. doi:10.1136/emj.17.3.188
- Blumberg, A., Weidmann, P., Shaw, S. and Gnadinger, M. (1988) Effect of various therapeutic approaches on plasma potatssium and major regulating factors in terminal renal failure. American Journal of Medicine, 85, 507-512. doi:10.1016/S0002-9343(88)80086-X
- Lin, J. and Huang, C. (1990) Successful initiation of hemodialysis during cardiopulmonary resuscitation due to lethal hyperkalemia. Critical Care Medicine, 18, 342-343. doi:10.1097/00003246-199003000-00022
- Mahoney, B.A., Smith, W.A.D., Lo, D.S., et al. (2005) Emergency interventions for hyperkalemia. John Wiley & Sons, Ltd., New York.
NOTES
*Corresponding author.

