Advances in Reproductive Sciences
Vol.05 No.03(2017), Article ID:78694,9 pages
10.4236/arsci.2017.53006
Varicocele and DNA Fragmentation in Senegalese Infertile Males
―A Study of 95 Cases
Mama Sy Diallo1*, Oumar Faye1, Yoro Diallo2, Rokhaya Ndiaye Diallo1, Jean Pascal Demba Diop1, Abdoulaye Séga Diallo1, Babacar Diao3
1Cytogenetic and Reproductive Biology Laboratory, University Teaching Hospital Aristide Le Dantec, Dakar, Senegal
2Department of Urology, Faculty of Health Sciences, University of Thies, Thies, Senegal
3Urology and Andrology Unit, University Teaching Hospital Aristide Le Dantec, Dakar, Senegal

Copyright © 2017 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: July 18, 2017; Accepted: August 21, 2017; Published: August 24, 2017
ABSTRACT
Varicocele is the first etiology of infertility in men worldwide and affects almost half of the men dealing with infertility in Senegal. Varicocele is associated with a high rate of sperm DNA fragmentation so this test is being more and more recommended especially when patients have to benefit from an ART (Assisted Reproductive Technology) procedure. The aim of our study was to assess if our patients with varicocele are concerned by higher DNA fragmentation rate in spermatozoon. Sperm samples were collected (95 cases of varicocele and 30 controls) and analyzed between January 2013 and June 2016 in a prospective study. Sperm DNA damage, characterized by the rate of DNA fragmentation was evaluated by TUNEL assay using fluorescence microscopy. There was a significant higher percentage of DNA fragmentation in patients with varicocele (p < 0.001), compared to controls. We plan to study a bigger cohort to assess this tendency and study the benefits of surgery in varicocele by evaluating DNA fragmentation after the procedure.
Keywords:
Varicocele, DNA Fragmentation, Male Infertility, TUNEL Assay

1. Introduction
Infertile men may have increased sperm DNA fragmentation [1] and varicocele that seems to be the first etiology of male infertility [2] [3] , are also correlated with high levels of sperm DNA fragmentation index [4] . In the general population, the prevalence of varicocele has been reported to be as high as 10 to15% [5] . In male infertility the prevalence of varicocele varies between 19 and 30% [6] . Previous studies in our context have showed that this prevalence was up to 40% [7] [8] . Studies have been conducted to explain how varicocele could be responsible for infertility but the pathophysiology of infertility in varicocele still remains unclear [3] . The main hypothesis and mechanisms described to be responsible for infertility are: Germinal cell dysfunction secondary to hypoxia (after venous stasis), the back flow of adrenal and renal metabolic products through the left spermatic vein, increased scrotal temperature and endocrinological changes. Thanks to progress in molecular biology we now know that all that phenomena can be responsible for increased oxidative stress [9] [10] and decreased anti-oxi- dant capacity on animal’s models [11] . These mechanisms are also responsible for apoptosis. The fact that apoptosis and oxidative stress are two main mechanisms of DNA fragmentation in spermatozoon, could explain why DNA fragmentation is increased in patients with varicocele. New data suggest that varicocelectomy improves sperm DNA damage in infertile men [12] and some authors like Kadioglu [13] , reported that high preoperative DNA fragmentation index was associated with a large decrease of DNA fragmentation in spermatozoon after surgery. If we refer to Esfahani’s review [14] , individuals who have high DNA fragmentation in their semen samples should be prior to surgery. Varicocele is a treatable affection that represents in our practice, almost half of our patients dealing with male infertility [15] . The aim of our study was to evaluate DNA fragmentation among our patients and assess the association of varicocele with increased DNA fragmentation in our population.
2. Materials and Methods
2.1. Patients
Our study was prospective and included 125 patients between January 2012and January 2016.Among them 95 were followed up for varicocele and 30 were controls. The control samples were collected from men who fathered within less than two years with normozoospermia values after semen analysis. We selected randomly, 95 men who came into our laboratory with one or more years of infertility and followed up for varicocele confirmed by ultrasound. We included men with clinically palpable varicocele (classified as grade 1, 2, or 3 according to Dubin and Amelar Classification [16] ) and assessed by ultrasound, we also included men with infra-clinical varicocele. Men with genital infection, cryptorchidism, hypogonadism or presenting a history of smoking and excessive alcohol use were excluded from the study. Men with any other disease that could be responsible for infertility were excluded too. All subjects provided informed consent and the study was approved by research and ethics committee.
2.2. Sperm Collection and Semen Analysis
Each patient provided a freshly ejaculated semen sample by masturbation after 3 days of sexual abstinence. The samples were analyzed within 30 min of collection. After liquefaction, seminal analysis was performed according to WHO 4th laboratory manual for semen analysis [17] and we used the modified classification of David [18] to analyze the morphology of the spermatozoon with normal forms ≥15%.
2.3. TUNEL Assay for Measurement of Sperm DNA Fragmentation
TUNEL test (Terminal deoxynucleotidyl transferase dUTP nick end labeling) was performed to assess sperm DNA fragmentation as described by Sharma’s [19] protocol. We followed all the steps of this standardized protocol to measure DNA fragmentation. We used “In Situ Cell Death Detection Kit, Fluorescein®” (Roche Diagnostics, GmbH, Mannheim, Germany) to evaluate DNA fragmentation. For the reading of the results, we chose fluorescence microscopy, more accessible in our practice than flow cytometry. In a previous study, we described the setting up of this protocol in our laboratory. We found a cut-off of 15% with an accuracy of 72.1% [15] to differentiate infertile men with DNA damage from healthy men.
3. Samples
The TUNEL test was performed after accruing10 samples for cost effectiveness. Fresh samples with 5 millions spermatozoa were collected after evaluation for volume and concentration. The samples were centrifuged at 600 g for 10 min at room temperature and the supernatant discarded. The obtained pellet was suspended in 1 ml of PBS (pH 7.4) and fixed with 4% paraformaldhéhyde (PF4)% (30 minutes at room temperature). The spermatozoon were then washed and resuspended in a (methanol/acetic acid) mixture and stored at ?20˚C until run time (Carnoy II solution). The test was performed according to the protocol of our laboratory [15] . To permeabilize cells, we used a solution of Triton. Briefly, after another wash with PBS (at 300 g for 5 min), we obtained a pellet that was suspended in the staining solution containing lwabeled nucleotides and enzyme terminal transferase. This mixture was kept in a dark room at 37˚ (Celsius degrees) for 1 hour. Negative and positive controls were included for each run. After the reaction (Hybridization), the cells were washed twice in PBS (at 300 g for 5 min) and suspended in 0.5 ml of DAPI solution (4’, 6’-diamidino-2-phenylindole) for counterstaining (30 minutes in the dark, at room temperature). The suspension was centrifuged (at 300 g for 5 min), and the pellet resuspended in 100 μl of PBS. The samples were smeared on super frost slides and mounted with Vectashield® (Vectorlaboratories, Inc.).
3.1. Fluorescence Microscopy
The slides were examined by fluorescence microscopy (BX50 Olympus) with DAPI (4’, 6 Diamino2 phénylindol) filter and FITC (Fluoroisothiocyanate) filter. The percentage of green spermatozoon with fragmented DNA (labelled with the TUNEL dUTP coupled with green fluorochrom) to the blue spermatozoon (Labeled with Dapi) gives the percentage of DNA fragmentation. Two hundred cells were counted for each slide.
3.2. Statistical Analysis
Student t test was used to compare continuous variables represented as mean with standard deviation (as mean age) and categorical variables as percentages. We compared two groups in our study: patients with varicocele and controls. Non- parametric variables like mean rates of DNA fragmentation were compared using the Mann-Whitney U-test.
Mann-Whitney U-test for unpaired non parametric data was p value less than 0.05 (p < 0.05) was considered statistically significant. Analysis was performed using R software version 3.2.2 for windows.
4. Results
4.1. Age
The mean ages of our patients with varicocele (n = 95) was 38.4 ± 1.1 and 38.4 ± 6.6 for the controls (n = 30). There was no significant difference between the two groups from a statistical point of view (p > 0.05).
4.2. Duration of Infertility
The mean duration of infertility was more than three years with 38.7 months ± 6. Patients were followed up for primary infertility in 71.3% of cases.
4.3. Varicocele
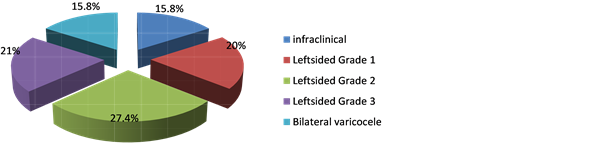
In our group of study, there were 95 varicocele and 15 had infraclinical varicocele. Left sided varicocele (grade 1, 2 and 3) were found in 65 cases. The repartition of those cases is presented in Figure 1. Grade 2 varicocele was the most frequent in our sample. Varicocele was unilateral in most of the cases (68.4% of palpable varicocele).
4.4. Semen Parameters
The main sperm characteristics of controls and patients are shown in Table 1. Of the 95 cases of varicocele, 36 (37.9%) had normal sperm parameters, while 59 (62.1%) had an abnormality in one or more of these parameters. The most
Figure 1. Repartition of patients according to the clinical grade of varicocele.
Table 1. Semen parameters in patients with varicocele and in control subjects.
frequent abnormality was oligoasthenoteratonecrozoospermia (20%) followed by asthenonecrozospermia (9%) teratozoospermia (Table 1).
4.5. Varicocele and DNA Fragmentation
DNA fragmentation in patients with varicocele (n = 95) was higher, from a statistical point of view than DNA fragmentation in controls (n = 30) (p < 0.001) (Table 2).
5. Discussion
The association between DNA damage and diminished reproductive outcomes is being increasingly recognized [20] . The most commonly performed tests to assess DNA fragmentation are SCSA (Sperm Chromatin Structure Assay) and TUNEL test. Even if standardized techniques were proposed to measure DNA fragmentation ( [21] [1] ), thresholds vary a lot among studies making comparisons difficult. Despite this difficulty, the conclusions are the same from the main studies: increased DNA fragmentation is associated with poor results after IVF (In vito Fertilization) or ICSI (Intra Cytoplasmic Sperm Injection) procedures ( [9] [22] [23] [24] [25] ). We found a very few number of study assessing the contrary. For example in [26] study, there were no correlation between DNA fragmentation and the issue of ART technique. But it is important to note the fact that in that study, the cases included oocyte donor (so young selected women with high quality oocyte). This can be a confusing bias because it is considered, that oocyte has the capacity of repairing DNA spermatozoa damage [27] . This finding could explain the good results after the ART procedure despite high level of DNA fragmentation in spermatozoon.
Guidelines for clinical utility of sperm DNA integrity testing are now available [20] [28] and varicocele belongs to one of the subgroups of infertile patients in which the fact of testing DNA fragmentation is justified. The new event is the fact that in that pathology DNA fragmentation is a reversible lesion after surgery ( [13] [29] ). This is as a new argument to support the clinical utility of this test. Indeed varicocele surgery has been a subject for controversy for many years. This surgical repair procedure, in our study context is associated with spontaneous pregnancy ( [7] [8] ) and better results in ART procedure. Using DNA fragmentation for triage can reduce the cost of varicocele management by the use of less com-
Table 2. DNA fragmentation of patients with varicocele compared to controls.
plicated technique of ART. Some authors like Jallouli [30] , Coccuza [31] or Daitch [32] showed that the improvement of semen quality after surgery helped to choose less expensive technique of ART or even avoid it [33] [34] , with spontaneous pregnancies following the repair [7] . In our study, DNA fragmentation is significantly more important in patients with varicocele. Wang meta-analysis [29] including 416 patients (240 varicocele and 176 controls) in seven studies showed the same tendency and there was a significant decrease after surgery. We find the same tendency in Kadioglu study [13] (2014) that included 92 cases of varicocele. After Varicocelectomy, authors note a decrease of sperm DNA fragmentation ( [35] [36] ) and even induction of spermatogenesis in case of azoospermia [37] . We think that those findings are important to consider in management of varicocele especially in our context where varicocele represents almost half of our patients with male infertility and where ART is not accessible to everyone because of the costs. The study of DNA fragmentation in varicocele could help us to better understand the pathophysiology of varicocele and also its treatment and management. The comprehension of the theories underlying DNA damage such as oxidative stress, abortive apoptosis and default of protamination during sperm compaction ( [14] [11] ) could make the link between this factors and infertility because, all that mechanisms responsible for DNA damage and infertility are factors described in varicocele. The correlation between semen parameters and DNA fragmentation is difficult to assess because of the number of controversial conclusions in literature. We even found that high DNA fragmentation could be associated with normal semen parameters [38] and this could be the reason of some cases of unexplained infertility.
In our study, significantly higher DNA fragmentation is observed in patients with varicocele compared to control (p < 0.05). These results are preliminary and were calculated on a small sample. A bigger cohort is necessary to assess our results. The mean rate of DNA fragmentation after TUNEL assay and reading by fluorescence microscopy was 22.4 +/− 10.0 in patients with varicocele vs 13.7 +/− 3.3 in controls. We noticed some obstacles for the use of DNA fragmentation test such as the high number of different methods, the lack of standardization, the use of subjective analyzing method instead of direct quantification. The first studies included most of the time some small cohort on a statistical point of view (Wang meta analysis). Despite all this, the tendency is the same in the studies. We think that it is a promising test to better understand varicocele and if it is well used, it can be a promising biomarker for the management of varicocele. We would like to know if this test can be used to measure the severity of varicocele and to evaluate the necessity of a surgical repair. We also want to know if there will be an improvement of sperm DNA quality after surgery within our patients and study the correlation between DNA fragmentation and spontaneous pregnancy after surgery.
6. Conclusion
We found significantly increased DNA fragmentation in our patients with varicocele. Furthermore, we plan to study if there is an improvement after surgical repair and evaluate if DNA fragmentation testing can be a tool in the management of varicocele.
Conflicts of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Cite this paper
Diallo, M.S., Faye, O., Diallo, Y., Diallo, R.N., Diop, J.P.D., Diallo, A.S. and Diao, B. (2017) Varicocele and DNA Fragmentation in Senegalese Infertile Males―A Study of 95 Cases. Advances in Reproductive Sciences, 5, 47-55. https://doi.org/10.4236/arsci.2017.53006
References
- 1. Sergerie, M., Bleau, G., Teulé, R., Daudin, M. and Bujan, L. (2005) Sperm DNA Integrity as Diagnosis and Prognosis Element of Male Infertility. Gynécologie Obstétrique & Fertilité, 3, 89-101. https://doi.org/10.1016/j.gyobfe.2005.02.012
- 2. Naughton, C.K., Nangia, A.K. and Agarwal, A. (2001) Pathophysiology of Varicoceles in Male Infertility. Human Reproduction, 5, 473-481. https://doi.org/10.1093/humupd/7.5.473
- 3. Marmar, J.L. (2001) The Pathophysiology of Varicoceles in the Light of Current Molecular and Genetic Information. Human Reproduction, 5, 461-472. https://doi.org/10.1093/humupd/7.5.461
- 4. Smith, R., Kaune, H., Parodi, D., Madariaga, M., Rios, R., Morales, I. and Castro, A. (2006) Increasedsperm DNA Damage in Patients with Varicocele: Relationship with Seminal Oxidative Stress. Human Reproduction, 4, 986-993.
- 5. Gorelick, J.I. and Goldstein, M. (1993) Loss of Fertility in Men with Varicocele. Fertility and Sterility, 59, 613-616. https://doi.org/10.1016/S0015-0282(16)55809-9
- 6. Alsaikhan, B., Alrabeeah, K., Delouya, G. and Zini, A. (2016) Epidemiology of Varicocele. Asian Journal of Andrology, 2, 179-181.
- 7. Diao, B., Sy, M.R., Fall, B., Sow, Y., Mohamed, S., Sine, B., Fall, A., Ndoye, A.K., Ba, M. and Diagne, B.A. (2012) Varicocèle et infertilité masculine. [Varicocele and Male Infertility.] Basic and Clinical Andrology, 22, 29-35. https://doi.org/10.1007/s12610-012-0157-9
- 8. Niang, L., Ndoye, M., Labou, I., Jalloh, M., Kane, R., Diaw, J.J., Ndiaye, A. and Guèye, S.M. (2009) Epidemiological and Clinical Profile of Male Infertility in the Senegal’s Grand-Yoff General Hospital in Senegal: A Study of 492 Cases. Andrology, 19, 103-107.
- 9. Sakkas, D. and Alvarez, J.G. (2010) Sperm DNA Fragmentation: Mechanisms of Origin, Impact on Reproductive Outcome, and Analysis. Fertility and Sterility, 4, 1027-1036. https://doi.org/10.1016/j.fertnstert.2009.10.046
- 10. Yoon, C.J., Park, H.J. and Park, N.C. (2010) Reactive Oxygen Species in the Internal Spermatic and Brachial Veins of Patients with Varicocele-Induced Infertility. Korean Journal of Urology, 5, 348-353. https://doi.org/10.4111/kju.2010.51.5.348
- 11. Aitken, R.J., Smith, T.B., Jobling, M.S., Baker, M.A. and De Iuliis, G.N. (2012) Oxidative Stress and Male Reproductive Health. Basic and Clinical Andrology, 1, 29-35.
- 12. Werthman, P., Wixon, R., Kasperson, K. and Evenson, D.P. (2008) Significant Decrease in Sperm Deoxyribonucleic Acid Fragmentation after Varicocelectomy. Fertility and Sterility, 90, 1800-1804.
- 13. Kadioglu, T.C., Aliyev, E. and Celtik, M. (2014) Microscopic Varicocelectomy Significantly Decreases the Sperm DNA Fragmentation Index in Patients with Infertility. Biomed Research International, 2014, Article ID: 695713. https://doi.org/10.1155/2014/695713
- 14. Esfahani, M.H.N. and Tavalaee, M. (2012) Origin and Role of DNA Damage in Varicocele. International Journal of Fertility & Sterility, 3, 141-146.
- 15. Diallo, M., Faye, O., Diallo, A., Diallo, Y. and Diao, B. (2015) Increased DNA Fragmentation in Patients with Infertility in Dakar (Senegal). Advances in Reproductive Sciences, 3, 97-105. https://doi.org/10.4236/arsci.2015.34012
- 16. Dubin, L. and Amelar, R.D. (1970) Varicocele Size and Results of Varicocelectomy in Selected Subfertile Men with Varicocele. Fertility and Sterility, 21, 606-609.
- 17. WHO (1999) Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction. 4rd Edition, Cambridge University Press, Cambridge.
- 18. Auger, J. and Eustache, F. (2000) Standardization of the Morphological Assessment of Human Spermatozoa According to Modified David’s Classification. Andrologie, 10, 358-373. https://doi.org/10.1007/BF03034491
- 19. Sharma, R.K., Sabanegh, E., Mahfouz, R., Gupta, S., Thiyagarajan, A. and Agarwal, A. (2010) TUNEL as a Test for Sperm DNA Damage in the Evaluation of Male Infertility. Journal of Urology, 76, 1380-1386.
- 20. Regan, R. (2014) Practice Committee of the American Society for Reproductive Medicine. Asian Journal of Andrology, 1, 31-38.
- 21. Agarwal, A., Majzoub, A., Esteves, S.C., Ko, E., Ramasamy, R. and Zini, A. (2016) Clinical Utility of Sperm DNA Fragmentation Testing: Practice Recommendations Based on Clinical Scenarios. Translational Andrology and Urology, 6, 935-950. https://doi.org/10.21037/tau.2016.10.03
- 22. López, G., Lafuente, R., Checa, M.A., Carreras, R. and Brassesco, M. (2013) Diagnostic Value of Sperm DNA Fragmentation and Sperm High-Magnification for Predicting Outcome of Assisted Reproduction Treatment. Asian Journal of Andrology, 6, 790-794. https://doi.org/10.1038/aja.2013.81
- 23. Lewis, S.E., John Aitken, R., Conner, S.J., Iuliis, G.D., Evenson, D.P., Henkel, R., Giwercman, A. and Gharagozloo, P. (2013) The Impact of Sperm DNA Damage in Assisted Conception and Beyond: Recent Advances in Diagnosis and Treatment. Reproduction Biomedecine Online, 4, 325-337.
- 24. Gil, M., Sar-Shalom, V., Sivira, Y.M., Carreras, R. and Checa, M.A. (2013) Sperm Selection Using Magnetic Activated Cell Sorting (MACS) in Assisted Reproduction: A Systematic Review and Meta-Analysis. Journal of Assisted Reproduction and Genetics, 4, 479-485. https://doi.org/10.1007/s10815-013-9962-8
- 25. Benchaib, M., Braun, V., Lornage, J., Hadj, S., Salle, B., Lejeune, H. and Guérin, J.F. (2003) Sperm DNA Fragmentation Decreases the Pregnancy Rate in an Assisted Reproductive Technique. Human Reproduction, 5, 1023-1028. https://doi.org/10.1093/humrep/deg228
- 26. Esbert, M., Pacheco, A., Vidal, F., Florensa, M., Riqueros, M., Ballesteros, A., Garrido, N. and Calderon, G. (2013) Impact of Sperm DNA Fragmentation on the Outcome of IVF with Own or Donated Oocytes. Reproductive Biomedecine Online, 23, 704-710.
- 27. Jaroudi, S., Kakourou, G., Cawood, S., Doshi, A., Ranieri, D.M., Serhal, P., Harper, J.C. and SenGupta, S.B. (2009) Expression Profiling of DNA Repair Genes in Human Oocytes and Blastocysts Using Microarrays. Human Reproduction, 10, 2649-2655. https://doi.org/10.1093/humrep/dep224
- 28. Practice Committee of American Society for Reproductive Medicine (2008) The Clinical Utility of Sperm DNA Integrity Testing. Fertility and Sterility, 90, S178-S180
- 29. Wang, Y.J., Zhang, R.Q., Lin, Y.J., Zhang, R.G. and Zhang, W.L. (2012) Relationship between Varicocele and Sperm DNA Damage and the Effect of Varicocele Repair: A Meta-Analysis. Reproductive BioMedicine Online, 3, 307-314.
- 30. Jallouli, H., Slimen, M., Sahnoun, A., Kechou, S., Ben Amar, S., Bahloul, A. and Mhiri, M.N. (2008) Surgical Treatment of Varicocele Improves Fertility and Facilitates Medically Assisted Procreation. Progrèsen Urologie, 8, 543-549.
- 31. Cocuzza, M., Cocuzza, M.A., Bragais, F.M.P. and Agarwal, A. (2008) The Role of Varicocele Repair in the New Era of Assisted Reproductive Technology. Clinics, 63, 395-404. https://doi.org/10.1590/S1807-59322008000300018
- 32. Daitch, J.A., Bedaiwy, M.A., Pasqualotto, E.B., Hendin, B.N., Hallak, J., Falcone, T., Thomas, A.J., Nelson, D.R. and Agarwal, A. (2001) Varicocelectomy Improves Intrauterine Insemination Success Rates in Men with Varicocele. Journal of Urology, 5, 1510-1513.
- 33. Cayan, S., Erdemir, F., Ozbey, I., Turek, P.J., Kadioglu, A. and Tellaloglu, S. (2002) Can Varicocelectomy Significantly Change the Way Couples Use Assisted Reproductive Technologies? The Journal of Urology, 167, 1749-1752.
- 34. Chiles, K.A. and Schlegel, P.N. (2016) Cost-Effectiveness of Varicocele Surgery in the Era of Assisted Reproductive Technology. Asian Journal of Andrology, 2, 259-261.
- 35. Telli, O., Sarici, H., Kabar, M., Ozgur, B.C., Resorlu, B. and Bozkur, S. (2015) Does Varicocelectomy Affect DNA Fragmentation in Infertile Patients? Indian Journal of Urology, 2, 116-119. https://doi.org/10.4103/0970-1591.152811
- 36. Ghazi, S. and Abdelfattah, H. (2011) Effect of Microsurgical Varicocelectomy on Sperm DNA Fragmentation in Infertile Men. Middle East Fertility Society Journal, 2, 149-153.
- 37. Pasqualotto, F.F., Sobreiro, B.P., Hallak, J., Pasqualotto, E.B. and Lucon, A.M. (2006) Induction of Spermatogenesis in Azoospermic Men after Varicocelectomy Repair: An Update. Fertility and Sterility, 85, 635-639.
- 38. Evgeni, E., Charalabopoulos, K. and Asimakopoulos, B. (2014) Human Sperm DNA Fragmentation and Its Correlation with Conventional Semen Parameters. Journal of Reproduction & Infertility, 1, 2-14.