3D Reconstruction with Spiral Computed Tomography in Choroidal Osteoma 5
Figure 3. B-scan ultrasonography showing clearly demon-
strable calcific densities in the posterior pole of the affected
eye (black arrow) and an associated exudative retinal de-
tachment.
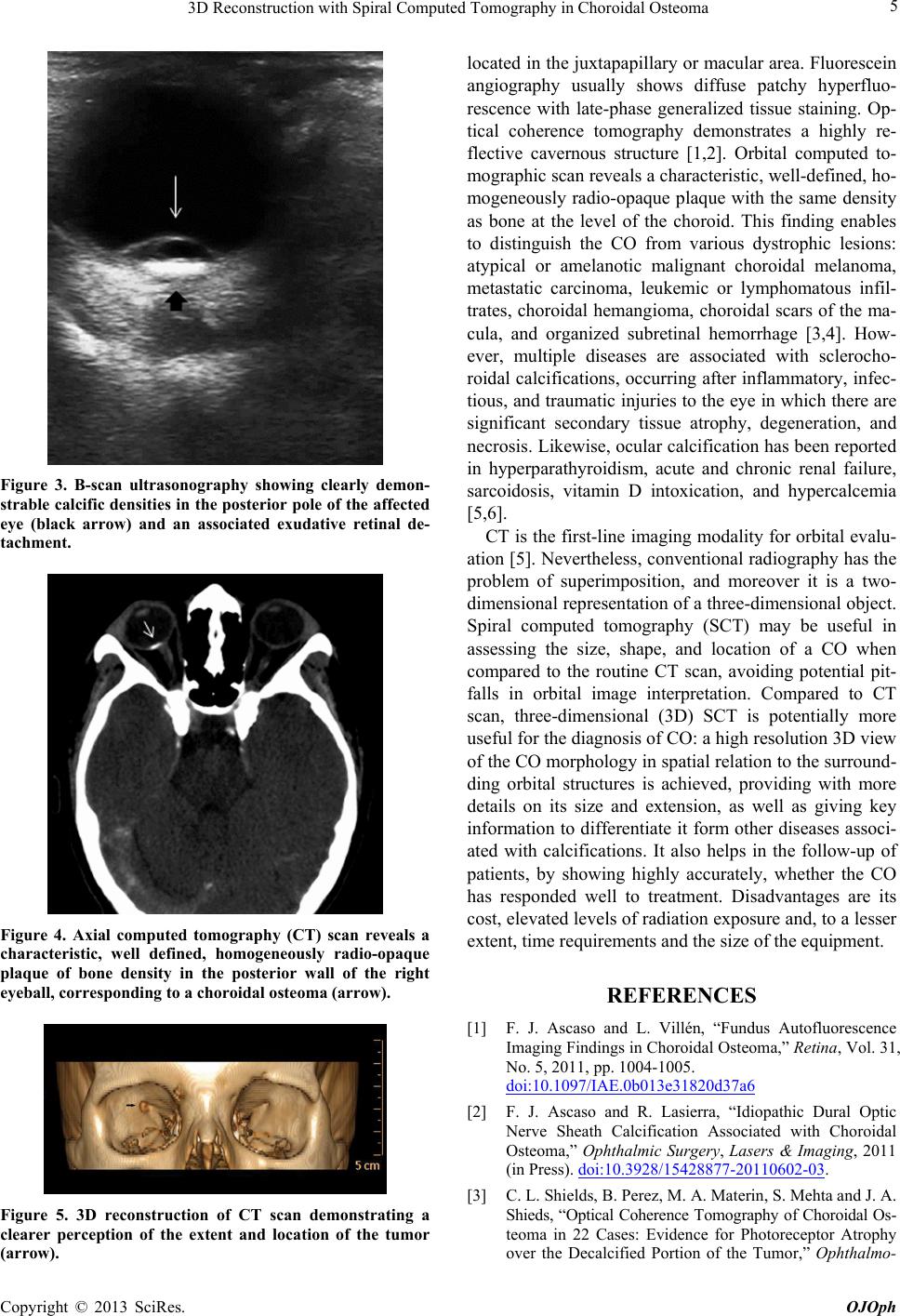
Figure 4. Axial computed tomography (CT) scan reveals a
characteristic, well defined, homogeneously radio-opaque
plaque of bone density in the posterior wall of the right
eyeball, corresponding to a choroidal osteoma (arrow).
Figure 5. 3D reconstruction of CT scan demonstrating a
clearer perception of the extent and location of the tumor
(arrow).
located in the juxtapap illary or macular area. Fluorescein
angiography usually shows diffuse patchy hyperfluo-
rescence with late-phase generalized tissue staining. Op-
tical coherence tomography demonstrates a highly re-
flective cavernous structure [1,2]. Orbital computed to-
mographic scan reveals a characteristic, well-defined, ho-
mogeneously radio-opaque plaque with the same density
as bone at the level of the choroid. This finding enables
to distinguish the CO from various dystrophic lesions:
atypical or amelanotic malignant choroidal melanoma,
metastatic carcinoma, leukemic or lymphomatous infil-
trates, choroidal hemangioma, choroidal scars of the ma-
cula, and organized subretinal hemorrhage [3,4]. How-
ever, multiple diseases are associated with sclerocho-
roidal calcifications, occurring after inflammatory, infec-
tious, and traumatic injuries to the eye in which there are
significant secondary tissue atrophy, degeneration, and
necrosis. Likewise, ocular calcification has been reported
in hyperparathyroidism, acute and chronic renal failure,
sarcoidosis, vitamin D intoxication, and hypercalcemia
[5,6].
CT is the first-line imaging modality for orbital evalu-
ation [5]. Nevertheless, conventional radiography has the
problem of superimposition, and moreover it is a two-
dimensional representation of a three-dimensional object.
Spiral computed tomography (SCT) may be useful in
assessing the size, shape, and location of a CO when
compared to the routine CT scan, avoiding potential pit-
falls in orbital image interpretation. Compared to CT
scan, three-dimensional (3D) SCT is potentially more
useful for the diagno sis of CO: a high resolu tion 3D view
of the CO morphology in sp atial relation to th e surround-
ding orbital structures is achieved, providing with more
details on its size and extension, as well as giving key
information to differentiate it form other diseases asso ci-
ated with calcifications. It also helps in the follow-up of
patients, by showing highly accurately, whether the CO
has responded well to treatment. Disadvantages are its
cost, elevated levels of radiation exposure and, to a lesser
extent, time requirements and the size of the equipment.
REFERENCES
[1] F. J. Ascaso and L. Villén, “Fundus Autofluorescence
Imaging Findings in Choroidal Osteoma,” Retina, Vol. 31,
No. 5, 2011, pp. 1004-1005.
doi:10.1097/IAE.0b013e31820d37a6
[2] F. J. Ascaso and R. Lasierra, “Idiopathic Dural Optic
Nerve Sheath Calcification Associated with Choroidal
Osteoma,” Ophthalmic Surgery, Lasers & Imaging, 2011
(in Press). doi:10.3928/15428877-20110602-03.
[3] C. L. Shields, B. Perez, M. A. Materin, S. Mehta and J. A.
Shieds, “Optical Coherence Tomography of Choroidal Os-
teoma in 22 Cases: Evidence for Photoreceptor Atrophy
over the Decalcified Portion of the Tumor,” Ophthalmo-
Copyright © 2013 SciRes. OJOph