Paper Menu >>
Journal Menu >>
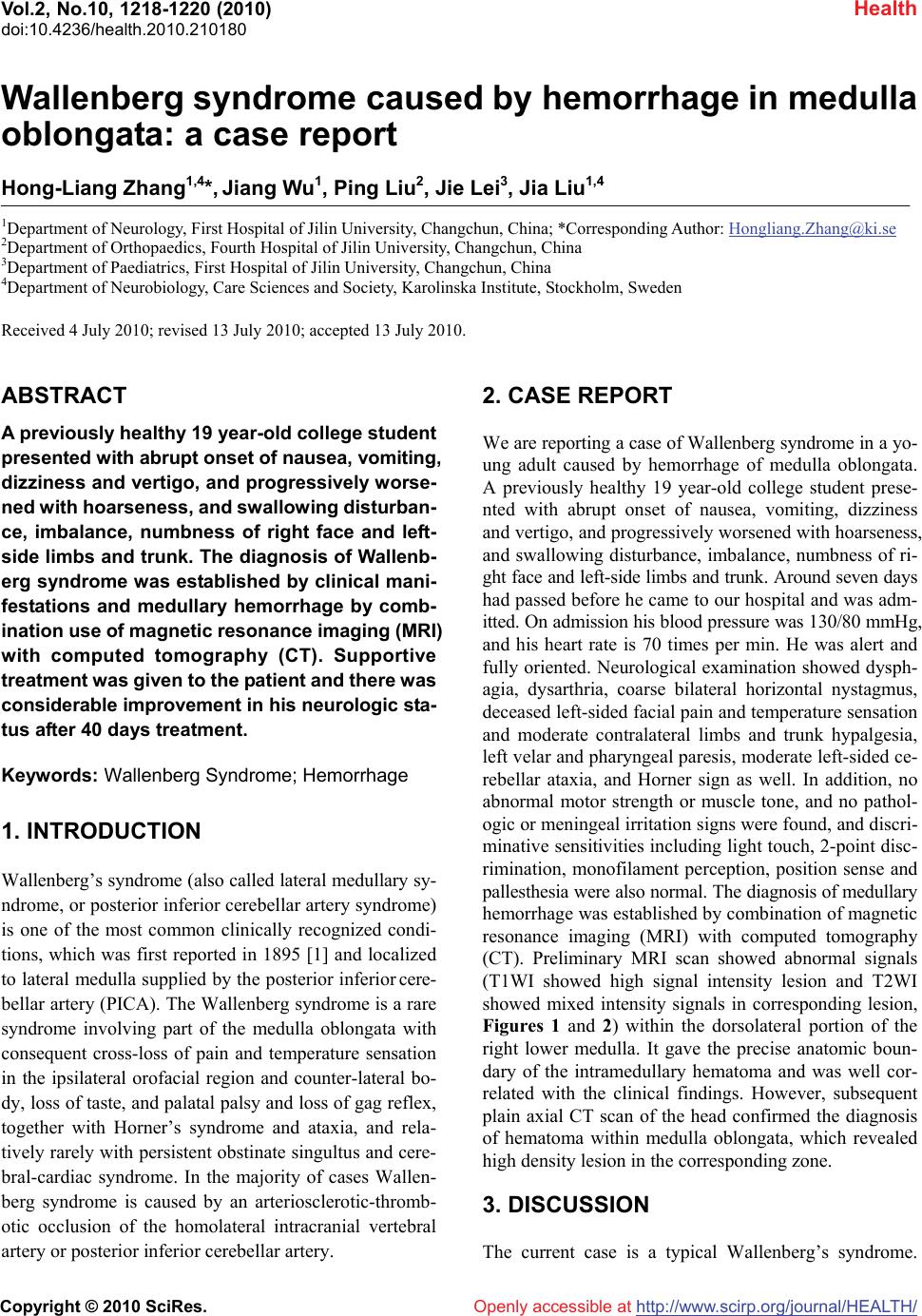 Vol.2, No.10, 1218-1220 (2010) Health doi:10.4236/health.2010.210180 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ Wallenberg syndrome caused by hemorrhage in medulla oblongata: a case report Hong-Liang Zhang1,4*, Jiang Wu1, Ping Liu2, Jie Lei3, Jia Liu1,4 1Department of Neurology, First Hospital of Jilin University, Changchun, China; *Corresponding Author: Hongliang.Zhang@ki.se 2Department of Orthopaedics, Fourth Hospital of Jilin University, Changchun, China 3Department of Paediatrics, First Hospital of Jilin University, Changchun, China 4Department of Neurobiology, Care Sciences and Society, Karolinska Institute, Stockholm, Sweden Received 4 July 2010; revised 13 July 2010; accepted 13 July 2010. ABSTRACT A previously healthy 19 year-old college student presented with abrupt onset of nausea, vomiting, dizziness and vertigo, and progressively worse- ned with hoarseness, and swallowing disturban- ce, imbalance, numbness of right face and left- side limbs and trunk. The diagnosis of Wallenb- erg syndrome was established by clinical mani- festations and medullary hemorrhage by comb- ination use of magnetic resonance imaging (MRI) with computed tomography (CT). Supportive treatment was given to the patient and there was considerable improvement in his neurologic sta- tus after 40 days treatment. Keywords: Wallenberg Syndrome; Hemorrhage 1. INTRODUCTION Wallenberg’s syndrome (also called lateral medullary sy- ndrome, or posterior inferior cerebellar artery syndrome) is one of the most common clinically recognized condi- tions, which was first reported in 1895 [1] and localized to lateral medulla supplied by the posterior inferior cere- bellar artery (PICA). The Wallenberg syndrome is a rare syndrome involving part of the medulla oblongata with consequent cross-loss of pain and temperature sensation in the ipsilateral orofacial region and counter-lateral bo- dy, loss of taste, and palatal palsy and loss of gag reflex, together with Horner’s syndrome and ataxia, and rela- tively rarely with persistent obstinate singultus and cere- bral-cardiac syndrome. In the majority of cases Wallen- berg syndrome is caused by an arteriosclerotic-thromb- otic occlusion of the homolateral intracranial vertebral artery or posterior inferior cerebellar artery. 2. CASE REPORT We are reporting a case of Wallenberg syndrome in a yo- ung adult caused by hemorrhage of medulla oblongata. A previously healthy 19 year-old college student prese- nted with abrupt onset of nausea, vomiting, dizziness and vertigo, and progressively worsened with hoarseness, and swallowing disturbance, imbalance, numbness of ri- ght face and left-side limbs and trunk. Around seven days had passed before he came to our hospital and was adm- itted. On admission his blood pressure was 130/80 mmHg, and his heart rate is 70 times per min. He was alert and fully oriented. Neurological examination showed dysph- agia, dysarthria, coarse bilateral horizontal nystagmus, deceased left-sided facial pain and temperature sensation and moderate contralateral limbs and trunk hypalgesia, left velar and pharyngeal paresis, moderate left-sided ce- rebellar ataxia, and Horner sign as well. In addition, no abnormal motor strength or muscle tone, and no pathol- ogic or meningeal irritation signs were found, and discri- minative sensitivities including light touch, 2-point disc- rimination, monofilament perception, position sense and pallesthesia were also normal. The diagnosis of medullary hemorrhage was established by combination of magnetic resonance imaging (MRI) with computed tomography (CT). Preliminary MRI scan showed abnormal signals (T1WI showed high signal intensity lesion and T2WI showed mixed intensity signals in corresponding lesion, Figures 1 and 2) within the dorsolateral portion of the right lower medulla. It gave the precise anatomic boun- dary of the intramedullary hematoma and was well cor- related with the clinical findings. However, subsequent plain axial CT scan of the head confirmed the diagnosis of hematoma within medulla oblongata, which revealed high density lesion in the corresponding zone. 3. DISCUSSION The current case is a typical Wallenberg’s syndrome. 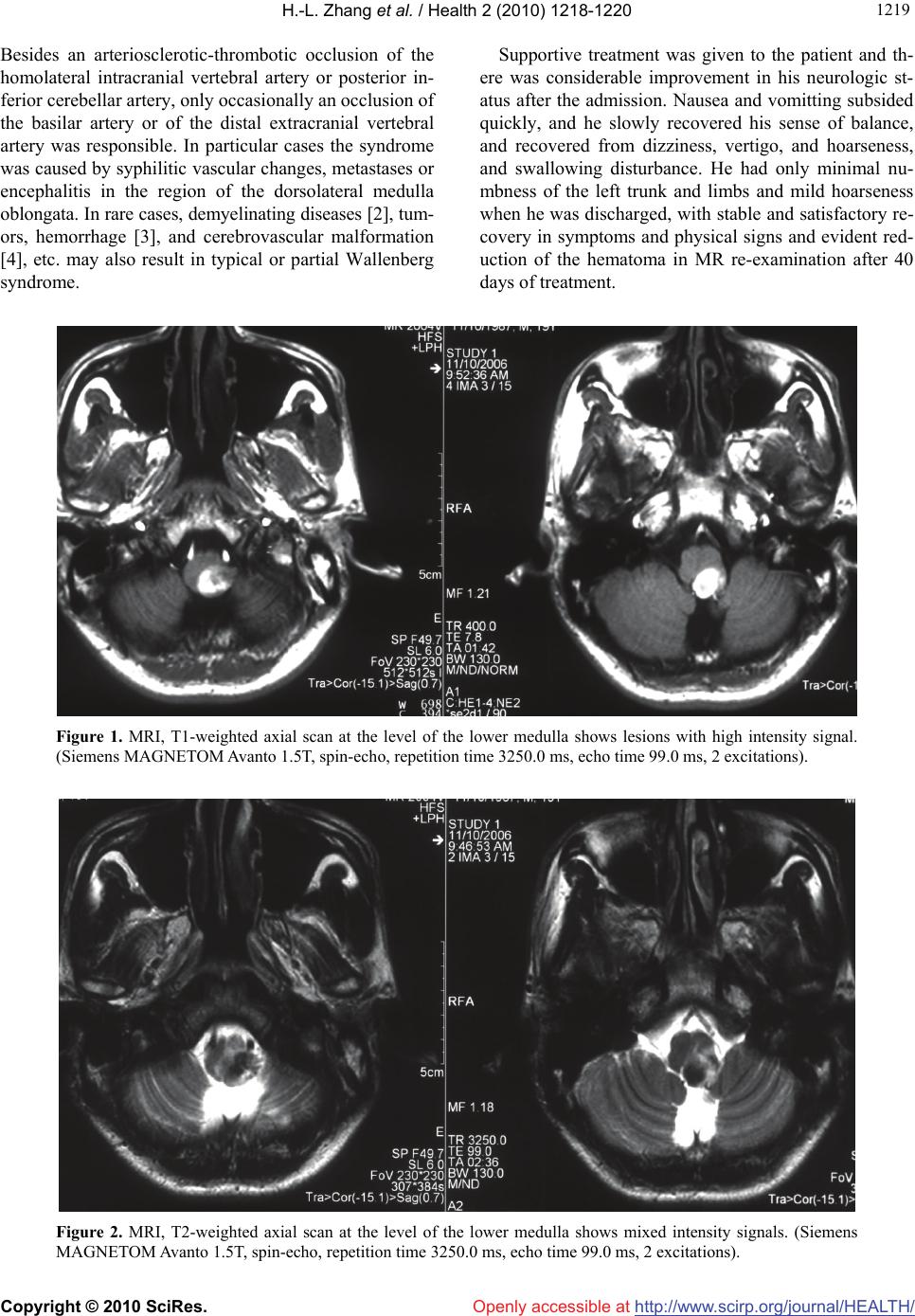 H.-L. Zhang et al. / Health 2 (2010) 1218-1220 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 121 1219 Besides an arteriosclerotic-thrombotic occlusion of the homolateral intracranial vertebral artery or posterior in- ferior cerebellar artery, only occasionally an occlusion of the basilar artery or of the distal extracranial vertebral artery was responsible. In particular cases the syndrome was caused by syphilitic vascular changes, metastases or encephalitis in the region of the dorsolateral medulla oblongata. In rare cases, demyelinating diseases [2], tum- ors, hemorrhage [3], and cerebrovascular malformation [4], etc. may also result in typical or partial Wallenberg syndrome. Supportive treatment was given to the patient and th- ere was considerable improvement in his neurologic st- atus after the admission. Nausea and vomitting subsided quickly, and he slowly recovered his sense of balance, and recovered from dizziness, vertigo, and hoarseness, and swallowing disturbance. He had only minimal nu- mbness of the left trunk and limbs and mild hoarseness when he was discharged, with stable and satisfactory re- covery in symptoms and physical signs and evident red- uction of the hematoma in MR re-examination after 40 days of treatment. Figure 1. MRI, T1-weighted axial scan at the level of the lower medulla shows lesions with high intensity signal. (Siemens MAGNETOM Avanto 1.5T, spin-echo, repetition time 3250.0 ms, echo time 99.0 ms, 2 excitations). Figure 2. MRI, T2-weighted axial scan at the level of the lower medulla shows mixed intensity signals. (Siemens MAGNETOM Avanto 1.5T, spin-echo, repetition time 3250.0 ms, echo time 99.0 ms, 2 excitations). 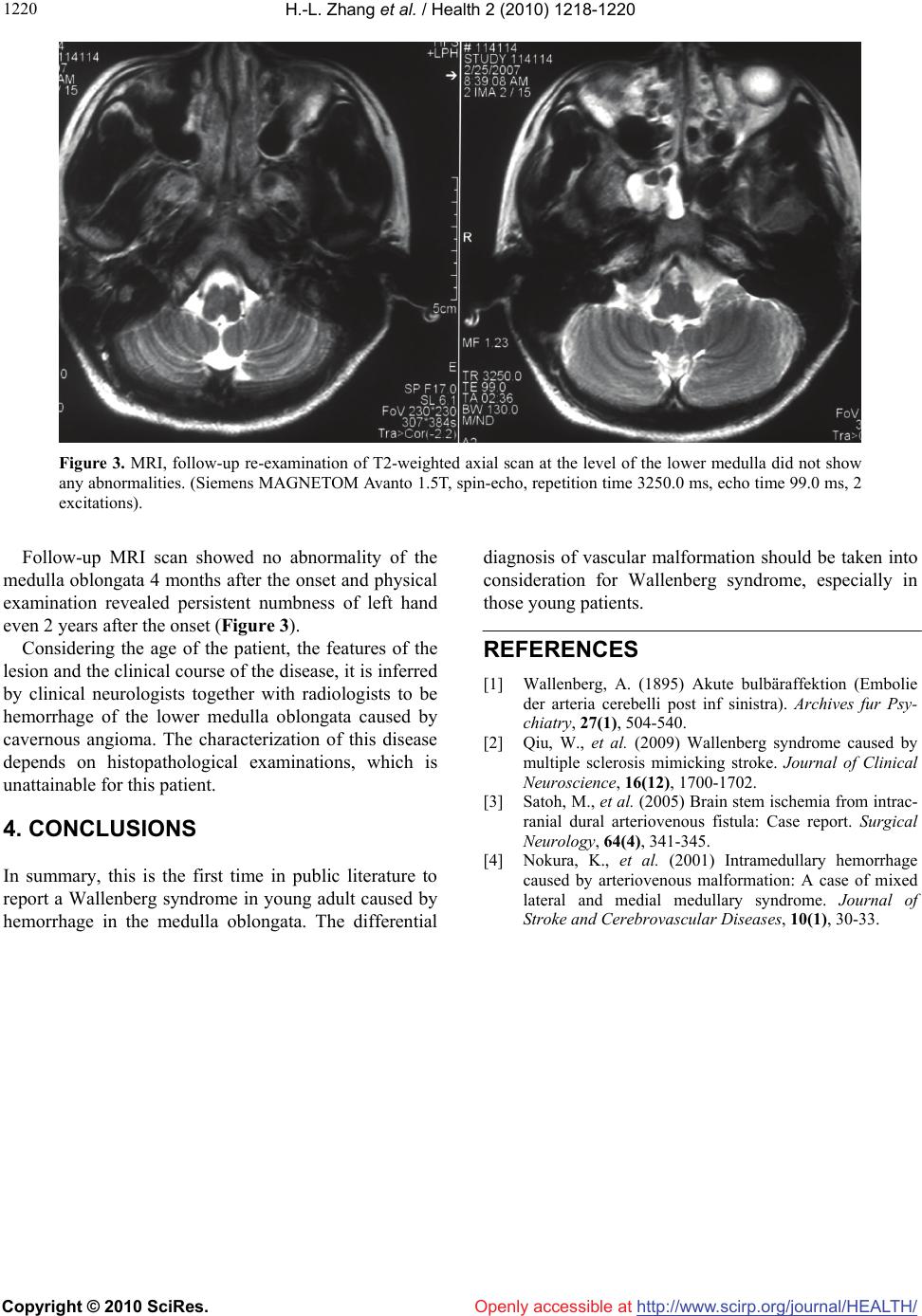 H.-L. Zhang et al. / Health 2 (2010) 1218-1220 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 1220 Figure 3. MRI, follow-up re-examination of T2-weighted axial scan at the level of the lower medulla did not show any abnormalities. (Siemens MAGNETOM Avanto 1.5T, spin-echo, repetition time 3250.0 ms, echo time 99.0 ms, 2 excitations). Follow-up MRI scan showed no abnormality of the medulla oblongata 4 months after the onset and physical examination revealed persistent numbness of left hand even 2 years after the onset (Figure 3). Considering the age of the patient, the features of the lesion and the clinical course of the disease, it is inferred by clinical neurologists together with radiologists to be hemorrhage of the lower medulla oblongata caused by cavernous angioma. The characterization of this disease depends on histopathological examinations, which is unattainable for this patient. 4. CONCLUSIONS In summary, this is the first time in public literature to report a Wallenberg syndrome in young adult caused by hemorrhage in the medulla oblongata. The differential diagnosis of vascular malformation should be taken into consideration for Wallenberg syndrome, especially in those young patients. REFERENCES [1] Wallenberg, A. (1895) Akute bulbäraffektion (Embolie der arteria cerebelli post inf sinistra). Archives fur Psy- chiatry, 27(1), 504-540. [2] Qiu, W., et al. (2009) Wallenberg syndrome caused by multiple sclerosis mimicking stroke. Journal of Clinical Neuroscience, 16(12), 1700-1702. [3] Satoh, M., et al. (2005) Brain stem ischemia from intrac- ranial dural arteriovenous fistula: Case report. Surgical Neurology, 64(4), 341-345. [4] Nokura, K., et al. (2001) Intramedullary hemorrhage caused by arteriovenous malformation: A case of mixed lateral and medial medullary syndrome. Journal of Stroke and Cerebrovascular Diseases, 10(1), 30-33. |

